Magnetic resonance (MR) is considered the gold standard in the assessment of myocardial morphology, function, perfusion, and viability. However, its main limitation is its scarce availability. In 2014, we installed the first MR scanner exclusively managed by a cardiology department within the publicly-funded Spanish healthcare system with the aim of improving patient-care, training and research in the department. In the time interval analyzed, July 2014 to May 2017, 3422 cardiac MR scans were performed (32minutes used per study; 96% with good quality; 75% with contrast media administration). The most prevalent clinical indications were cardiomyopathy (29%) and ischemic heart disease (12%). Twenty-five percent of studies were conducted in the context of research protocols. Follow-up studies predominated among outpatients, while pretherapeutic assessment was more common in hospitalized patients. The presumptive diagnosis was changed by cardiac MR scanning in up to 20% of patients investigated for ischemic heart disease. The installation and operative management of an MR scanner in our cardiology department has allowed us to integrate this technique into daily clinical practice, modify our clinical protocols, optimize access to this technology among cardiac patients, improve training, and conduct clinical research.
Keywords
Magnetic resonance (MR) is considered the gold standard in the evaluation of myocardial morphology, function, flow, perfusion, and viability, all in a single and completely noninvasive test.
The first work with cardiac MR dates from the beginning of the 1980s,1–4 and Spanish cardiology adopted the technique in the mid-1990s.5–9 During the last decade, its clinical use has become widespread in virtually all third-level Spanish hospitals. The latest available data from the RECALCAR 2015 registry10,11 showed an average of 403 ± 269 studies per tertiary center.
Due to technological advances and rapid improvements in cardiac MR, the initial indications for the modality have been expanded and are undergoing continuous growth. This increase has intensified the problem of waiting lists and complicates access to machine time in most hospitals because the procedures are conducted in integrated systems in radiology departments, which must handle more than just cardiovascular conditions. Accordingly, the Spanish Society of Cardiology and the Spanish Society of Medical Radiology developed a consensus document12 recommending the creation of multidisciplinary heart disease units or committees under the coordination and supervision considered most appropriate in each case, considering the characteristics of each center.
In this article, we present our initial experience with the operative management of the first MR system installed in a cardiology department in a hospital in the Spanish national health system.
STARTING POINT AND OBJECTIVES OF THE MAGNETIC RESONANCE SYSTEM INSTALLATIONAt the end of the 2013, our center had 2 MR systems, both in the radiology department. Cardiovascular studies were performed with a 0.5T system, which could handle about 100 studies annually. The radiology and cardiology departments performed and interpreted the studies together. Due to the low intensity of the magnetic field, the study quality failed to meet recommended standards.12–14 Additionally, the health care delay exceeded 24 months.
Due to the need to improve waiting times and study number and quality, in addition to the limitation on acquisition time in the systems installed at that time and, finally, the desire of the cardiology department to participate in research projects requiring MR, a set of actions was undertaken that led to the installation of an MR system in the cardiology department. The hypothesis was that this action would constitute the ideal setting for the systematic incorporation of best clinical practices, bring patient care closer to the patient's natural environment, and promote the effective participation of professionals, adoption of new forms of action, and research innovation and development. Based on this hypothesis, an MR system was installed in order to improve patient care, training, and research in the cardiology department.
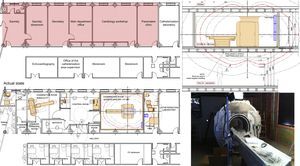
LOCATION, SYSTEM, AND TOOLSAfter a viability plan, it was decided to place the MR system in the area of the cardiology department assigned to procedures (Figure 1). The work took 4 months, from March to July 2014.
Detail of the location and facility modifications required for installation of the magnetic resonance (MR) system. The MR system occupied an area previously assigned to the secretariat, training room, offices, and clinics on the second floor of the building. Installation of the system required a detailed architectural study and an adaptation plan to guarantee that the building, opened in 1975, was capable of supporting the 3800kg weight of the MR system. It was necessary to reinforce the structure and install magnetic shielding in the lower floor, build a Faraday cage, and install a Quench tube to the exterior (detail in the upper right panel). The magnet, due its size and weight, was introduced through the building facade. A comparison is shown of the faculty layout before and after assembly of the MR system. The lower right panel shows the MR system during the installation process.
The system installed was a Philips Achieva DS 1.5T (Philips Healthcare; the Netherlands), with gradient strengths of up to 66 mT/m and a speed of up to 180 T/m/s. Chest and cardiac coils were equipped. A postprocessing system was implemented (IntelliSpacePortal, Philips Healthcare), based on client-server technology, which allows the concurrent use of the system from virtual work stations at any point of access to the hospital network, with a capacity for analysis and quantification of cardiac MR studies in line with the current literature.
By analyzing the different suppliers’ offers, the participation of the cardiology department was decisive in the selection of these systems. The funding model for this initiative was the result of a public-private collaboration. The cardiology department workforce was strengthened with the recruitment of 2 cardiologists. The employment of diagnostic radiology technicians, required for the development of the program, was financed with research funding from the cardiology department.
The safety and scan features of the MR system were adjusted to meet the current guidelines of the Society of Cardiovascular Magnetic Resonance (SCMR).14–16 In addition, the studies were interpreted in accordance with the current recommendations of the SCMR17 and the European Association of Cardiovascular Imaging. M.B.P. developed an information management system dedicated to the cardiac MR process, which allowed the analysis of data for this manuscript.
All of the information and images obtained from the MR studies are sent in DICOM format to the picture archiving and communication system (PACS) of the center for storage and safekeeping in accordance with current legislation.
TRAINING AND HUMAN RESOURCES PLANGiven the complexity of the technology deployed, an initial training plan was implemented, with the collaboration of the manufacturer. This program included an MR safety session for the entire department and a practical course on clinical applications.
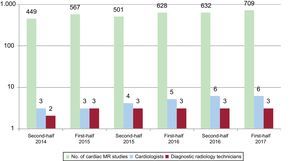
In May 2017, the personnel involved in the cardiac MR program comprised a stable team of 3 diagnostic radiology technicians and 6 cardiologists with specific training; the changes over time in human resources are shown in Figure 2. The cardiologists involved are accredited or in the process of accreditation, a requirement considered essential by the department to guarantee quality according to current consensus guidelines.12 The training of staff linked to the cardiac MR program was accompanied by a series of stays in national centers of excellence (), totaling 39 months of training (median, 6 months/cardiologist).
ACTIVITY PROGRAMMINGEach day, a diagnostic radiology specialist and a cardiologist are exclusively dedicated to cardiac MR (). The partnership with the radiology department during the development of the project has been fluid and collaborative. Initially, a radiologist was available 1 day a week, but due to the workload in the radiology development, a work station was installed in that department to allow the radiologist to remotely collaborate in a simple and immediate way.
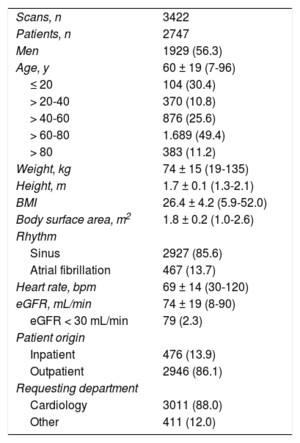
NUMBER OF STUDIES AND PROCEDURES PERFORMEDFrom its installation and implementation on July 23, 2014 to May 31, 2017, 3422 MR studies have been performed in 2747 patients. In this period, the system was used on 719 days, with an average of 4.8 studies per day. The baseline characteristics of the population and the temporal variation in the number of studies are shown in Table 1 and Figure 3, respectively. The cardiology department was the largest applicant for studies, and most of the patients were outpatients. A total of 272 studies (8.0% of the total) were derived from hospital centers to which third-level hospital services are provided. The study could not be completed in 50 patients (1.5%) due to their refusal or the presence of metallic material that contraindicated it. During the test, the scan was interrupted in 37 patients (1.1%); the most frequent reasons were the development of anxiety or claustrophobia symptoms (n = 22, 59.5%), extravasation of contrast medium (n = 6, 16.2%), heart failure decompensation (n = 6; 16.2%), and mild allergy to contrast medium (n = 3, 8.1%).
Baseline Characteristics of the Study Population
| Scans, n | 3422 |
| Patients, n | 2747 |
| Men | 1929 (56.3) |
| Age, y | 60 ± 19 (7-96) |
| ≤ 20 | 104 (30.4) |
| > 20-40 | 370 (10.8) |
| > 40-60 | 876 (25.6) |
| > 60-80 | 1.689 (49.4) |
| > 80 | 383 (11.2) |
| Weight, kg | 74 ± 15 (19-135) |
| Height, m | 1.7 ± 0.1 (1.3-2.1) |
| BMI | 26.4 ± 4.2 (5.9-52.0) |
| Body surface area, m2 | 1.8 ± 0.2 (1.0-2.6) |
| Rhythm | |
| Sinus | 2927 (85.6) |
| Atrial fibrillation | 467 (13.7) |
| Heart rate, bpm | 69 ± 14 (30-120) |
| eGFR, mL/min | 74 ± 19 (8-90) |
| eGFR < 30 mL/min | 79 (2.3) |
| Patient origin | |
| Inpatient | 476 (13.9) |
| Outpatient | 2946 (86.1) |
| Requesting department | |
| Cardiology | 3011 (88.0) |
| Other | 411 (12.0) |
BMI, body mass index; eGFR, estimated glomerular filtration rate.
Unless otherwise indicated, the data represent No. (%) or mean (range).
Contrast medium administration (gadobutrol 1 mmol/mL) was indicated in 2573 studies (75.2%); the dose administered to all patients with an estimated glomerular filtration rate > 30mL/min was 0.15 mmol/kg. No contrast medium was administered to patients with an estimated glomerular filtration rate < 30mL/min.
The study duration was a median of 32 [interquartile range, 11] minutes. The increase in activity allowed the delay to be reduced from 24 months to 10 days for outpatients and to less than 24hours for admitted patients.
STUDY QUALITY AND INDICATIONSStudy quality was classified as good or acceptable in 95.6% of the cases, and the images were completely interpretable.17 The quality was classified as poor in 4.3%, but the study could still be interpreted, with the remaining 0.1% of the studies not interpretable. The variables significantly associated with a poor quality study were older age (50 vs 72 years, P < .01), obesity (body mass index, 26.3 vs 28.9, P < .01), the presence of arrhythmias (2% in sinus vs 17.8% in atrial fibrillation, P < .01), and a higher heart rate (69 vs 83 bpm, P < .01).
After study interpretation, the MR report was issued on the same day of the scan for 78.3% of the studies and in the first 72hours for 88.2%.
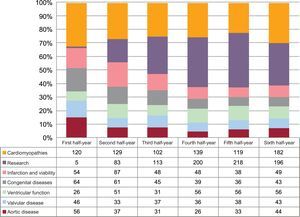
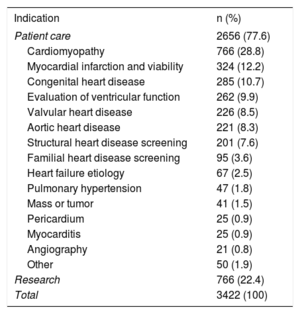
The number of studies by indication for cardiac MR in the center is shown in Table 2. The 2 most frequent indications were cardiomyopathies and research studies, which constituted almost 45% of requests. The temporal variation in the specific weight of the 6 most frequent clinical indications (85.3% of the total number of clinical studies) and of the research studies is shown in Figure 3. The latter indication has markedly increased in recent years and currently accounts for 32% of the activity.
Indications for Cardiac Magnetic Resonance Studies
| Indication | n (%) |
|---|---|
| Patient care | 2656 (77.6) |
| Cardiomyopathy | 766 (28.8) |
| Myocardial infarction and viability | 324 (12.2) |
| Congenital heart disease | 285 (10.7) |
| Evaluation of ventricular function | 262 (9.9) |
| Valvular heart disease | 226 (8.5) |
| Aortic heart disease | 221 (8.3) |
| Structural heart disease screening | 201 (7.6) |
| Familial heart disease screening | 95 (3.6) |
| Heart failure etiology | 67 (2.5) |
| Pulmonary hypertension | 47 (1.8) |
| Mass or tumor | 41 (1.5) |
| Pericardium | 25 (0.9) |
| Myocarditis | 25 (0.9) |
| Angiography | 21 (0.8) |
| Other | 50 (1.9) |
| Research | 766 (22.4) |
| Total | 3422 (100) |
Of the cardiac MRs requested with a clinical indication, 15.3% did not find structural heart disease, and 406 patients were classed as normal. The proportion of normal studies was higher among outpatients than among inpatients (17.1% vs 5.5%, P < .05). The most frequently issued diagnoses in relation to the most common clinical indications are shown in Table 3. As examples of health care utility, MR ruled out the presence of previous infarction in 20.6% of the studies requested due to suspected ischemic heart disease; it ruled out structural heart disease in 19.3% of the studies requested due to suspected cardiomyopathy and in 16.2% of those requested for evaluation of ventricular function due to insufficient echocardiography results. It also detected previously unknown disease, such as silent myocardial infarction in 28.6% and previous myopericarditis in 9.5% of scans requested for the etiological study of heart failure, and diagnosed bicuspid aortic valve in 10.8% of those studies requested due to aortic dilatation.
Main Diagnoses Recorded in the Cardiac Magnetic Resonance Report in Relation With Each of the Main Clinical Indications
| Indication | n (%) | Diagnosis | n (%) |
|---|---|---|---|
| Cardiomyopathy | 766 (28.8) | Hypertrophic cardiomyopathy | 183 (23.9) |
| Normal | 148 (19.3) | ||
| Dilated cardiomyopathy | 94 (12.3) | ||
| Intermediate phenotype* | 39 (5.1) | ||
| Myopericarditis | 36 (4.7) | ||
| Others | 266 (34.7) | ||
| Myocardial infarction and viability | 324 (12.2) | Chronic ischemic heart disease | 198 (61.0) |
| Acute ischemic heart disease | 60 (18.4) | ||
| Normal | 18 (5.6) | ||
| Nonischemic dilated cardiomyopathy | 6 (1.9) | ||
| Myopericarditis | 5 (1.5) | ||
| Others | 38 (11.6) | ||
| Congenital heart disease | 285 (10.7) | Coarctation of the aorta | 54 (19.0) |
| Bicuspid aortic valve | 48 (16.8) | ||
| Ventricular septal defect | 22 (7.8) | ||
| Tetralogy of Fallot | 22 (7.8) | ||
| Interatrial communication | 22 (7.8) | ||
| Others | 116 (40.8) | ||
| Ventricular function | 262 (9.9) | Chronic ischemic heart disease | 45 (17.3) |
| Valvular heart disease (≥ moderate) | 45 (17.3) | ||
| Normal | 42 (16.2) | ||
| Dilated cardiomyopathy | 32 (12.2) | ||
| Toxic cardiomyopathy | 15 (5.6) | ||
| Others | 82 (31.4) | ||
| Valvular heart disease | 226 (8.5) | Aortic regurgitation | 96 (42.6) |
| Aortic stenosis | 24 (10.4) | ||
| Mitral/tricuspid valve disease | 24 (10.4) | ||
| Bicuspid aortic valve | 24 (10.4) | ||
| Normal | 6 (2.7) | ||
| Others | 53 (23.5) | ||
| Aorta | 221 (8.3) | Aortic dilatation | 118 (53.3) |
| Bicuspid aortic valve | 24 (10.8) | ||
| Normal | 20 (9.0) | ||
| Aortic regurgitation | 16 (7.2) | ||
| Aortic stenosis | 11 (4.8) | ||
| Others | 33 (14.9) |
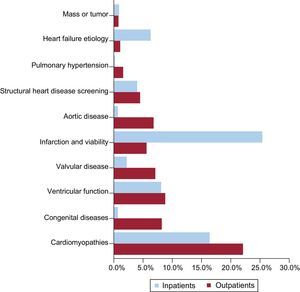
The different proportions in the MR indications between outpatients and inpatients are shown in Figure 4. For hospitalized patients, more studies were requested for therapeutic purposes, such as to establish the presence of myocardial infarction and/or for viability assessment (25.4% vs 5.6%, P < .01) and for the etiological study of heart failure (6.3% vs 1.1%, P < .01). In outpatients, the main differences were found in prospective monitoring of chronic disease, such as congenital heart disease (8.2% vs 0.7%, P < .01), aortic disease (6.8% vs 0.7%, P < .01), valvular diseases (7.1% vs 2.2%, P < .01), and pulmonary hypertension (1.6% vs 0.2%, P < .05).
The integration of MR into daily clinical practice has enabled modification of health care protocols. MR has replaced nuclear medicine in the evaluation of myocardial viability and computed tomography in the assessment and monitoring of chronic aortic disease, with a consequent reduction in ionizing radiation. Likewise, MR has been standardized for the study of cardiomyopathies and congenital heart diseases, family screening of patients with a suboptimal ultrasound window, and preimplantation assessment of the arrhythmic substrate and ventricular function in implantable cardioverter-defibrillator patients. Other functions are applied to selected patients, such as the precise monitoring of ventricular size and function, evaluation of the right ventricle prior to cardiac valvular surgery, or preimplantation assessment of long-term ventricular assist devices.
RESEARCH AND TRAININGIn total, MR studies performed for research projects comprised 766, which represented 22.4% of all studies conducted in the period evaluated. The main research lines focused on cardiotoxicity (484 studies, 63.2%), acute myocardial infarction (170, 22.2%), cellular therapy (21, 2.7%), brain damage in atrial fibrillation (16, 2.1%), safety of intracardiac devices (9, 1.2%), and others (66, 8.6%). Before installation of the cardiac MR, the department was involved in just 1 research study requiring MR; moreover, the scans had to be outsourced. During these 3 years, the department has participated in 12 studies requiring cardiac MR. Through some of these projects, collaborations have been established with centers of excellence such as the CIBERCV (Biomedical Research Networking Center on Cardiovascular Diseases) and the Centro Nacional de Investigaciones Cardiovasculares (National Center for Cardiovascular Research) or with public-private innovation projects. In addition, the amount obtained in competitive research funds and clinical trials has increased to 1 million euros, exceeding the total cost of the MR system. The cumulative impact factor in publications indexed by the cardiology service has jumped from 34.86 (13 publications) in 2013 to 117.85 (39 publications) in 2016.
Integration of the MR within the cardiology department has also had an impact on the training provided. Before 2014, our cardiology medical residents moved to external centers to undergo cardiac MR training. As a whole, 29 months of training have been performed in the 2014 to 2017 period (80.1% of the total time). Looking to the future, at the time of writing this work, the relevant applications have been received, and 37 months of medical residents and postresident training have been committed as personnel external to the center up to 2020. Finally, in relation to the project presented, a monographic practical course on cardiac MR was designed and implemented in 2016 for radiologists, cardiologists, and diagnostic radiology technicians; most attendees were external to the center.
The increase in training activity has made the service more attractive for medical residents choosing cardiology, with the department jumping from number 971, the last place to be filled in 2014, to number 564 in 2017, becoming the first center in the autonomous community of Salamanca to run out of available places.
LESSONS LEARNED AND RECOMMENDATIONSThis is the first work to analyze the patient care, research, and training outcomes of the installation of an MR system in a cardiology department of the Spanish national health system. Similar experiences have been published in the United Kingdom18 and Germany,19,20 countries that also have publicly-funded health systems. The results reported in the present work are comparable to those of other groups, except in the distribution of study indication, which would be affected by the situation in each hospital. In our center, the installation of the MR system has proven to be a useful health care tool that systematically incorporates best practices and eliminates waiting lists, increases the effective participation of department staff, promotes training, and improves research.
The enormous usefulness of cardiac MR is now beyond doubt.21–23 If its availability were unlimited, it would be the most used noninvasive diagnostic technique for the evaluation of most cardiovascular diseases. However, as with any cutting-edge technology, its implementation is not without problems.24,25 The main limitations are the high cost of the system, the complexity of its installation due to the logistical, infrastructure, and environmental requirements and, to some extent, the specialization and training of the personnel involved, because its implementation involves a profound modification of the standard functioning and dynamics of a cardiology department. In our experience, the main challenge in the implementation and current operation of cardiac MR has been and remains the training and incorporation of specialized personnel that maximize its performance. Collective effort and collaboration are paramount to ensure that this technique is truly practical and efficient. The guidelines for proper functioning and development must take into account the following considerations: a) identification of the short-, mid-, and long-term needs and objectives of cardiac MR; b) analysis of daily compulsory tasks; c) definition of the knowledge, skills, and abilities (competencies) required for the proper performance of the tasks associated with cardiac MR; d) periodic evaluation of the performance of these tasks for each staff member; and e) definition of points or areas for improvement resulting from the previous analyses.
In a European public health environment similar to ours, the cost-effectiveness of cardiac MR in the context of ischemic heart disease has been proven.26 However, incorporation of MR in a cardiology department could be interpreted as an unnecessary expense in times of an economic downturn. Indeed, in our experience, other departments interpreted this investment as signifying a cut to other, more important, activities. As happened in our case, the hospital management must explain the source of the funding and its objectives to all hospital departments and support innovative projects whose future evaluation and profitability are established in advance in the 3 classic areas: patient care, training, and research.27–29 Cardiac MR has improved departmental training and has opened lines of collaboration with requests for competitive research projects, not only with centers of excellence,30,31 but also with other hospital departments we previously did not collaborate with so actively. From a health care point of view, the new system may have helped to improve the health care outcomes of the department, as shown by the RECALCAR registry data,10,11 although it is difficult to assess the specific weight of the implementation of this technique in the general results.
One of the main barriers to the widespread adoption of this technique in cardiology departments is the cost of the system and personnel involved in its use. We know that a public-private collaboration and establishment of a training program were the 2 elements of success in our innovative model. In relation to the economic cost and profitability, no studies have shown that the use of MR in cardiology departments is cost-effective, except with regard to ischemic heart disease.26 However, in our experience, it should be noted that, in 3 years of operation, the funds obtained from research projects that prioritized MR have exceeded the initial cost of the MR system and its installation.
CONCLUSIONSThe installation and operative management of cardiac MR in a cardiology department of the Spanish national health system is a useful health care tool that systematically incorporates better health care practices and eliminates waiting lists, achieves the effective participation of department staff, improves training, and promotes research.
FUNDINGThe present work was funded by the Instituto de Salud Carlos III (Spanish Ministry of Economy, Industry, and Competitiveness) within the RIC (Red de Investigación Cardiovascular [Cardiovascular Research Network]), the Proyecto de Investigación de Excelencia (PIE14/00066), the Action Plan for the promotion of clinical and translational research, ERDF (European Regional Development Fund) and CIBERCV funding, and by the Regional Health Service of Castile and León within the GRS1203/A/15 research project and the 2015 program for the recognition and encouragement of professionals who are completing their residency.
CONFLICTS OF INTERESTNone declared.
The authors thank Pedro Vara, Leticia Vicente, Irene Martínez, Iván Zamarro, M. Jesús García-Sánchez, Jendri Pérez, Olga Durán, Marta Alonso, Carlos Lugo, and Carolina Ingaramo for their help in obtaining the data reviewed in this article.