Tako-tsubo syndrome (TKS) is a clinical syndrome characterized by reversible left ventricular dysfunction in the absence of epicardial coronary obstruction. Although several pathogenic mechanisms have been proposed (ie, multivessel epicardial spasm, catecholamine-induced myocardial stunning, spontaneous coronary thrombus lysis, and acute microvascular spasm), its causes are still unknown.1,2 Possible causes of TKS are the presence of vulnerable plaques or flow alteration, but they have not been well elucidated.
In our study, we sought to perform a functional and morphological assessment of the left anterior descending artery (LAD) in TKS patients by using optical coherence tomography (OCT) and pressure-temperature wire.
From January 2016 to May 2017, 14 consecutive TKS patients, admitted to 2 institutions and defined accordingly to Mayo Clinic diagnostic criteria,1 were included. The study was approved by the ethics committee of our center and each patient provided written informed consent. A pressure-temperature guidewire (Certus, St Jude) was introduced in the LAD at the level of the second diagonal branch. After induction of hyperemia with adenosine (140μg/kg/min), fractional flow reserve and the index of microcirculatory resistance (IMR) were measured as previously shown.3 Fractional flow reserve and IMR were considered abnormal if < 0.80 and > 22, respectively.3 OCT acquisition was then performed using a commercially available system for intracoronary imaging (C7XR Fourier-Domain System; LightLab Imaging, Westford, Massachusetts, United States) on the LAD (at least 50mm) during continuous injection of contrast medium (3mL/s, iodixanol 370, visipaque, GE Health Care, Cork, Ireland) through the guide catheter with an injection pump. The presence of coronary plaque on OCT pullback was analyzed offline by 2 independent investigators (LightLab Imaging, Wesrford, Massachusetts, United States).
Thirteen patients (92.8%) were women, with a mean ± standard deviation age of 66.1 ± 11.5 years. Coronary angiography showed no significant stenosis of at least 50% in the LAD. OCT and pressure-temperature wire analysis were performed in 14 and 12 patients, respectively. OCT analysis showed a normal 3-layer vessel wall, without atherosclerotic plaque, images of plaques rupture, plaques erosion, or intraluminal thrombus. None of the patients had fractional flow reserve ≤ 0.80, with a mean value of 0.96 ± 0.18, while 10 (83.3%) patients had microvascular dysfunction with IMR ± standard deviation of 33.8 ± 11.4 (Table).
Baseline Clinical Characteristics of the Tako-tsubo Syndrome Patients
| Patient | Age, y | Sex | Cardiovascular risk factors | Stressful event | Ballooning pattern | Initial EF % | Discharge EF% | Time since symptom to pressure-temperature wire measurement (hours) | FFR | IMR | OCT |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 67 | M | Smoking | Physical | Apical | 40 | 56 | NA | NA | NA | Normal |
| 2 | 71 | F | None | Physical | Apical | 40 | 55 | 4 | 0.96 | 51.8 | Normal |
| 3 | 50 | F | Smoking | Emotional | Apical | 60 | 59 | NA | NA | NA | Normal |
| 4 | 55 | F | Smoking | Emotional | Apical | 34 | 43 (55, 1 month after discharge) | 12 | 0.96 | 43.3 | Normal |
| 5 | 70 | F | Hypertension, hypercholesterolemia | Emotional | Apical | 40 | 51 (63, 1 month after discharge) | 8 | 0.97 | 39.2 | Normal |
| 6 | 86 | F | Hypertension | Physical | Apical | 35 | 55 | 18 | 0.94 | 33 | Normal |
| 7 | 72 | F | None | Emotional | Apical | 50 | 60 | 8 | 0.96 | 37.2 | Normal |
| 8 | 68 | F | Hypertension, hypercholesterolemia | Emotional | Apical | 45 | 50 (65, 1 month after discharge) | 120 | 0.92 | 26.9 | Normal |
| 9 | 63 | F | Hypertension | Emotional | Midventricular | 35 | 45 (55, 1 month after discharge) | 18 | 0.98 | 19 | Normal |
| 10 | 47 | F | Hypertension, hypercholesterolemia | Emotional | Apical | 30 | 60 | 4 | 0.95 | 25.6 | Normal |
| 11 | 61 | F | Hypertension | Physical | Apical | 40 | 60 | 254 | 0.96 | 10.9 | Normal |
| 12 | 83 | F | Hypertension, hypercholesterolemia | Emotional | Apical | 40 | 60 | 27 | 0.98 | 37 | Normal |
| 13 | 59 | F | Hypertension, hypercholesterolemia | Emotional | Apical | 35 | 65 | 11 | 0.98 | 39 | Normal |
| 14 | 64 | F | Hypercholesterolemia | Emotional | Apical | 55 | 60 | 12 | 0.96 | 43 | Normal |
EF, ejection fraction; F, female; FFR, fractional flow reserve; IMR, index of microcirculatory resistance; M, male; NA, not available; OCT, optical coherence tomography.
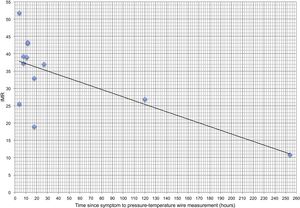
The physiopathology of TKS is unknown, but can be related to intracoronary thrombus, either emerging from a ruptured thin-cap fibroatheroma or plaque erosion in the LAD, which is responsible for the typical left ventricle appearance. Coronary thrombus or at least the coronary plaque, which has led to thrombus formation, may be undetectable by coronary angiography, but may be seen on OCT.4 Nevertheless, our OCT analysis did not show any coronary plaque or thrombotic remnants on LAD, also excluding the presence of any atherosclerotic coronary plaque. This is in contrast with a recent study that showed a high prevalence of atherosclerotic plaques in these patients without any plaque rupture or thrombi.5 Unlike that study, our patients were younger with fewer cardiovascular risk factors, suggesting that the presence of atherosclerotic plaques could be a finding with no causal relationship with TKS. Despite the lack of epicardial lesions, we show that some degree of microvascular dysfunction may be present. In the absence of atherosclerotic alteration on epicardial vessels, this dysfunction can be caused either by thrombi or by intense and temporary spasms in the coronary microcirculation. Thrombi embolism from the epicardial vessel can be excluded by our OCT findings. A significant negative correlation was also found between the extent of microvascular dysfunction and the time from symptom onset to IMR analysis (R, - 0.69; P = .012), in line with previous data6 (Figure). In particular, a normal IMR value was found in a patient studied 10 days after the appearance of initial symptoms, suggesting the reversibility of this microvascular dysfunction.
In conclusion, our study shows that LAD of TKS patients may exhibit some degree of microvascular dysfunction in the absence of atherosclerotic or vulnerable plaque. Future studies are needed to further determine the causes of this dysfunction.
FUNDINGG. Jiménez Brítez received a grant from Coronary and Structural Course in Barcelona 2015 for this study.
.