Keywords
INTRODUCTION
The use of low dose (75-350 mg) acetylsalicylic acid or aspirin in the secondary prevention of cardiovascular disease (CVD) is fully accepted and 60% of the price of the drug is reimbursed by the Spanish National Health Service (NHS). However, in individuals with no history of CVD, the treatment is less well accepted, despite the fact that 2 meta-analyses of results from 5 studies in over 50 000 patients,1,2 which showed this to be an effective treatment option.3-7 This is at least in part due to the fact that in many countries, including Spain, low dose aspirin is not approved for primary prevention of CVD, and has been associated with gastrointestinal (GI) bleeding and hemorrhagic stroke. Hayden et al1 showed that in a cohort of 1000 individuals with a 5% risk of suffering a fatal or non-fatal coronary event within 5 years (e.g. a 50 year old male with LDL cholesterol of 210 mg/dL and systolic blood pressure of 140 mm Hg), treatment with aspirin would prevent 6-20 myocardial infarctions (MI). However, the treatment would also cause between 0 and 2 hemorrhagic strokes and between 2 and 4 episodes of severe GI bleeding. In individuals with a 1% risk of developing coronary heart disease within 5 years (e.g. a 45 year old male with no risk factors for CVD), it would prevent between 1 and 4 MI, but would cause the same number of hemorrhagic events.
The American Heart Association8 recommends treatment with aspirin in individuals with an annual risk of ≥1%. European guidelines do not specify a risk threshold, though they do recommend primary prevention of CVD with aspirin in individuals with diabetes, well-controlled hypertension, and in males with high multifactorial risk of CVD.9 The consensus document on the use of antiplatelet agents recommends aspirin for primary prevention in high-risk patients, i.e. those with diabetes and hypertension.10
We were unable to find any economic analyses of the use of low-dose aspirin in primary prevention. Existing treatment recommendations have therefore been drawn up without taking into account their possible economic implications. The aim of the present study was to bring economic arguments into the discussion surrounding the use of low-dose aspirin in the primary prevention of CVD and to estimate the budget impact from the perspective of the Spanish NHS.
METHODS
Model Structure
To estimate the cost-effectiveness of low-dose aspirin in the primary prevention of CVD, a Markov model was designed using Data Pro by TreeAgeTM. One-year cycles were used over a 10 year period so as to allow correlations with the second European Joint Task Force risk prediction charts.11 The model consisted of five principal health states: no prior history of CVD (no known heart disease, no peripheral artery disease or cerebrovascular disease), prior history of stroke, prior history of MI, prior history of CVD, and death (Figure 1).
Figure 1. Simplified structure of the health state transition model. ASA indicates acetylsalicylic acid; CHD: coronary heart disease; CVD, cardiovascular disease; MI, myocardial infarction.
All of the hypothetical subjects started the model with no prior history of CVD. Each year, each subject had a risk of CVD (defined as fatal MI, non-fatal MI, or sudden death), stroke (fatal or non-fatal, ischemic, or hemorrhagic), or death through other causes. Independently of those risks, each individual also had a risk of GI bleeding. The distribution of episodes of GI bleeding was assumed to be uniform over the year, and was calculated using a half-cycle correction in the Markov model (assuming that the events occurred in the middle of the year). All risks were dependent on whether the individual had been treated with aspirin or not.
Within the health-state transition model, individuals who experienced fatal events moved to the state "death," those who had a first stroke moved to the state "prior stroke" and those who had a first non-fatal MI moved to the state "prior MI." The remaining individuals remained in the state "no prior CVD."
Individuals with a history of stroke or MI presented a higher risk of experiencing a new event. When an individual with a prior stroke had a non-fatal MI he moved to the state "prior CVD." The same transition was applied to individuals with prior MI who suffered a stroke. Individuals with a prior stroke who had another stroke remained in the state "prior stroke." Individuals with a prior MI who had a further MI remained in the state "prior MI." It was assumed that all individuals would be treated with low-dose aspirin after the first CVD event, independently of the original treatment (placebo or low-dose aspirin). Several surveys have shown that low-dose aspirin is used in approximately 90% of cases after an acute coronary event.11,12
Whether or not an individual is treated with low-dose aspirin in daily practice depends on his risk of CHD and of adverse events. Furthermore, the cost-effectiveness of aspirin will depend on the base-line risk of CHD. The annual risk was calculated using the Framingham algorithm, as the the SCORE algorithm was not available when the model was developed.1,13
For the base case, annual risk was set at 1.5% (a 10 year risk of approximately 15%). The choice of 15% is in line with American and European guidelines on the use of aspirin in primary prevention. Aspirin also reduces the risk to a similar degree as statins (28% with aspirin and 31% with statins in the WOSCOPS study14). Given that aspirin is much cheaper than statins and given that the latter are recommended when there is a 10 year risk of CHD of ≥20%, a lower threshold was used in the present study.
The results are presented as cost per life-year gained (LYG) and cost per quality adjusted life year (QALY). Both costs and outcomes were discounted at 3%.
Clinical Data
Efficacy data for aspirin in primary prevention were extracted from published meta-analyses and efficacy data for its use in secondary prevention were taken from the CAPRIE trial.1,2,15
One meta-analysis1 provided detailed information (e.g. annual risk, risk reduction and 95% confidence intervals [CI]) on the impact of aspirin on the risk of CHD (defined as fatal MI, non-fatal MI, and sudden death), total stroke, and all cause mortality, as well as providing information on the relationship between fatal and non-fatal CHD. The other meta-analysis2 provided additional information on the relationship between fatal and non-fatal stroke and the proportion of ischemic strokes.
It was possible to vary the baseline risk of CHD in the health-state transition model, and the risk of stroke is related to the risk of CHD. According to Hayden et al,1 there are 0.54 cerebrovascular events for every cardiovascular event.
Table 1 shows the annual risk of all complications when the baseline annual risk of CHD is set at 1.5%.
The CAPRIE15 study provides results for individuals with a prior history of MI and ischemic stroke, as well as for the total cohort of individuals with a prior vascular event (Table 1). The risk of an event is greater in secondary prevention than in primary prevention although after a second MI or stroke it was not varied in the model, as the CAPRIE study did not specify the risk of new events after suffering 2 or more.
Cost Data
The study was carried out from the perspective of the Spanish NHS, so only direct medical costs were included. All monetary units are in 2003 euros. Costs for the following events were included: fatal MI, non-fatal MI, fatal stroke, non-fatal ischemic stroke, non-fatal hemorrhagic stroke, GI bleeding, and follow-up after a cardiovascular event (MI, stroke, or both).
The majority of costs for Spain were calculated using the SOIKOS Health Care Costs Data-base (2004),16 in which all costs for acute care, except fatal stroke, were provided in terms of diagnostic-related groups. The cost of fatal stroke was calculated from the cost of ischemic stroke, as it was assumed that fatal stroke is related to non-fatal stroke in the same way that fatal MI is related to non-fatal MI. Data from Levy et al17 were used to calculate the cost of follow-up. In that study, a 2 year time horizon was used and costs were divided into disease management costs for the acute phase and for follow-up. For Spain, the costs of hospitalization were obtained from hospital data-bases and national tariffs, and costs of follow-up were calculated using a decision tree. Data on patient management and resource use for the decision tree were obtained from the literature, official national statistics, and local expert opinion (Delphi panel). Costs were for 1999 and were updated using the Spanish medical inflation index (www.ine.es) to obtain values for 2003 (Table 2).
Although low-dose aspirin for primary prevention is currently not reimbursed in Spain, for the purposes of the model it was assumed that such treatment was publically financed, and that patient co-payment would cover 40% of the cost. It was assumed that Spanish NHS would cover the full cost of treatment for secondary prevention, as the majority of patients would be in categories which are fully reimbursed. The price to the public of aspirin 100 mg was 0.082 euros (retail price plus value added tax).18
Utilities
Data on utilities were obtained from the medical literature19,20 and were based on the Time-Trade-Off method.
Utilities for post-MI and post-stroke were 0.88 (95% CI, 0.84-0.93) and 0.68 (95% CI, 0.53-0.83), respectively. The scores for MI were based on 2 to 5 measurements over 1.5 years in 67 patients, and utilities for moderate stroke were based on a meta-analysis of utility studies.19,20 When an MI occurred, a utility score of 0 was applied for 1 week.21 Extracraneal hemorrhaging was determined to have no permanent effects and reduced utility for 2 weeks (utility, 0.5 for 2 weeks).22 If the patient had had stroke and MI, it was assumed that he or she had the worst utility, i.e. the utility score for stroke.
Budget Impact
Two sources were used to calculate the number of patients who would be eligible for treatment.23,24 Marrugat et al23 calculated the percentage of the population with low, medium and high risk of CHD by adapting the Framingham risk prediction algorithm for use in Spain. They also classified risk groups according to sex, smoking habit, and diabetes. Baena Díez et al24 reported the percentage of the Spanish population who smoked and were diabetic by age and sex. By combining data from these 2 studies with the size of the Spanish population (www.ine.es), the number of patients with a 10-year risk of suffering an event of >15% and >20% was obtained, as shown in Table 3. In the moderate risk group (10%-19% at 10 years), it was assumed that patients were evenly distributed above and below the 15% mark.
Sensitivity Analysis
Several sensitivity analyses were perfomed using the following variables: baseline risk of CHD, discount rates, risk of GI bleeding, risk of hemorrhagic stroke, cost of complications, and utility values.
Monte Carlo Analysis
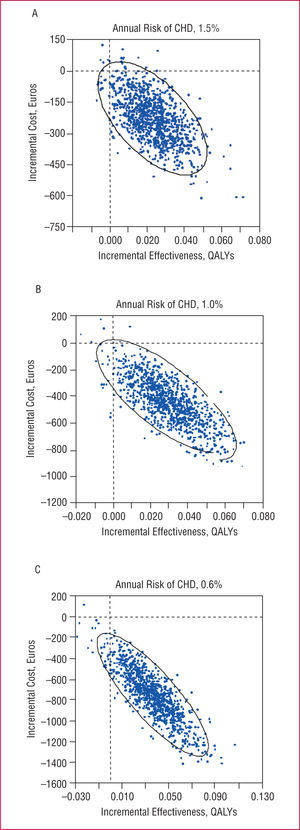
The effects of low-dose aspirin were incorporated in the model as point estimates with 95% CI (Table 1), as were costs and utilities (Table 2). The model was run 1000 times values for the variables in the model were randomly assigned each time. Annual risks for CHD of 0.6% (threshold for treatment recommended by the US Preventive Services Task Force1), 1.0% (threshold recommended by the American Heart Association8), and 1.5% were applied in the Monte Carlo analysis (cost per QALY gained).
RESULTS
Model Validation
To validate the health-state transition model, we compared the number of coronary events avoided as reported by Hayden et al,1 with the number calculated by the model. For a 5 year risk of 5%, Hayden et al1 predicted that 6 to 20 events could be avoided for every 1000 patients treated, whilst the model predicted that the number of events avoided would be between 11 and 17. Given a 5 year risk of 1%, Hayden et al1 predicted that the number of events avoided would be between 1 and 4, whilst the present model predicted that 3 to 4 events would be avoided.
Base Case
For individuals with an annual risk of CHD of 1.5% (risk at 10 years, 14%-15%), the 10 year cost was e 5768 (95% CI, €5366-6185) without low-dose aspirin and €4971 (95% CI, €4383-5581) with aspirin. On average, treatment with low-dose aspirin led to a per-patient saving of e 797 (95% CI, €301-1330) over 10 years. A saving of €19.30 was obtained during the first year, though this was non-significant. Significant savings were seen after 2 years of treatment. The number of life years gained was 8.33 (95% CI, 8.32-8.34) and 8.36 (95% CI, 8.33-8.39), respectively, and the number of QALYs gained was 8.20 (95% CI, 8.16-8.24) and 8.24 (95% CI, 8.18-8.29), respectively.
Sensitivity Analysis
Varying the discount rate between 0% and 6% did not affect the results, as low-dose aspirin provides effectiveness at low cost.
In the base case, the annual risk of CHD was set at 1.5%, which would be cost-saving for the Spanish NHS. The sensitivity analysis indicated that treatment with low-dose aspirin already produces cost-savings (although these were not significant) when the annual risk of CHD is ≥0.244% (Figure 2). An annual risk of CHD of 0.244% is, for example, the risk for a male, non-smoker aged 55 years or over, with no diagnosis of diabetes or hypertension, and with a normal lipid profile.
Figure 2. Impact of annual risk of CHD on cost (based on an annual risk of CHD of 0.244%, the threshold at which treatment with low-dose aspirin produces cost savings). CHD indicates: coronary heart disease.
The decision to treat or not with low-dose aspirin depends on both the risk of CHD and on the risk of adverse effects. In the base case, the risk of stroke was 1.02 times higher with low-dose aspirin than with placebo. The 95% CI published by Hayden et al were 0.85-1.23. Even when the upper limit is applied, treatment with low-dose aspirin is still cheaper and more effective than placebo (Table 4). In the base case, the risk of GI bleeding was 1.7 times greater with aspirin than with placebo. The 95% CI published by Ha yden et al were 1.4-2.1. Again, even when the upper limit was applied, treatment with low-dose aspirin was still cheaper and more effective than placebo. Even when the 2 upper limits for stroke and GI bleeding were applied, treatment with aspirin still led to significant cost-savings, even after reducing the annual risk of EC to 0.6% (the threshold for treatment recommended by the US Preventive Services Task Force1).
Changing the cost of complications based on the 95% CI shown in table 2 did not affect the results of the cost-effectiveness analysis, and nor did using the 95% CI for the MI and stroke utility values.
Monte Carlo Analysis
When applying annual risks of CHD of 0.6%, 1.0%, and 1.5%, treatment with aspirin in Spain was the dominant option in 98.0%, 97.1%, and 97.8% of cases, respectively (Figure 3).
Figure 3. Monte Carlo analysis (cost/QALY). QALY indicates quality adjusted life year; CHD, coronary heart disease.
Budget Impact Analysis
By running the model at annual risks of 1.5% and 2% (10 year annual risk of ≥15% and 20%) and combining the results with the number of patients who were eligible for treatment (Table 3), it was calculated that an investment of e 22.3 million could lead to a saving of e 26.5 million (net savings) for the Spanish NHS in the first year, if all eligible patients (annual risk of ≥1.5%) were treated with low dose aspirin. After year 3, an investment of e 64.1 million would mean a saving of approximately e 149.4 million if all eligible patients were treated.
DISCUSSION
This economic analysis has shown that the use of low dose aspirin as primary prevention in patients with a moderately increased risk of CHD (10 year risk of 15%), leads to significant cost savings from the public payer perspective. Treatment with low dose aspirin to prevent a first cardiovascular event in patients with moderately increased risk of CHD would save money for the Spanish NHS. In addition to the clinical benefit then (for example, in terms of LYG), there are also economic arguments to support the use of aspirin in primary prevention. Many other primary prevention interventions, and indeed many secondary prevention interventions, are not actually cost saving.
Plans Rubio25 reviewed the cost-effectiveness of cardiovascular prevention programs in Spain in terms of the net cost per LYG. The cost-effectiveness ratios ranged from 2600 to 80 000 $/LYG in males and 4500 to 230 000 $/LYG in women. In males aged 40 to 59 years, interventions classified in increasing order of cost-effectiveness were: stopping smoking cessation (2608-3738 $/LYG), treatment of moderate to severe hypertension (8564-38 678 $/LYG), treatment of mild hypertension (11 906-59 840 $/LYG), diet treatment (16 143-20 158 $/LYG), and medical treatment for hypercholesterolemia ($33 850-81 010/LYG). In women, the classification was: stopping smoking cessation (4482-5756 $/LYG), treatment of moderate to severe hypertension (9585-57 983 $/LYG), treatment of mild hypertension (15 248-86 075 $/LYG), diet treatment (57 175-62 154 $/LYG), and medical treatment for hypercholesterolemia (104 100-259 150 $/LYG). Given that the cost of aspirin is lower and it produces more life years or QALYs, it does not make sense to calculate the incremental cost-effectiveness ratio. In fact, the negative values are difficult to interpret.
The cost of aspirin is very low and the possible savings to the Spanish NHS could be high. In the web-page of the Organization for Economic Co-operation and Development (www.oecd.org) there is information on spending on drugs and health. In 2001, Spain spent €64 500 million on health, and 17.8% (according to the latest available figures, from 1990) were spent on drugs €11 500 million). If all eligible patients took aspirin, financing aspirin for the primary prevention of CHD would mean an increase in the drug budget of €22.3 million (0.2%), but would lead to a decrease in the overall health care budget of €26.5 million (0.04%).
The validity of these results is supported by the sensitivity analysis. Given a 10 year risk of ≥3%, aspirin is cost-effective (though the results are not significant), and the saving can be noted from the first year of treatment on. The model also predicted a number of coronary events which was very smilar to that published by Hayden et al, which further supports the validity of the results presented.
It may appear surprising that the Monte Carlo analysis showed aspirin to be the dominant treatment option in a higher percentage of patients when the annual risk was lower. However, this can be explained by the fact that aspirin's effectiveness does not depend on the annual risk of CHD, so that aspirin will always be more effective in the prevention of CHD. This increased effectiveness is defined as a reduction in relative risk which does not depend on the level of baseline risk. In the lowest risk group, the reduction in relative risk is maintained, but there is a smaller reduction in absolute risk and a reduction in the standard error. An analysis of Figure 3 shows a tighter clustering of results and lower ranges for the groups with a lower annual risk of CHD. Furthermore, at lower annual risks, hemorrhagic complications such as GI bleeding and hemorrhagic stroke become more relevant, as the risk of these complications does not vary with the annual risk of CHD. When the annual risk of CHD falls below 0.6%, the number of cases in which aspirin is dominant begins to decrease, to 93% with an annual risk of 0.5%, and under 90% when the annual risk is 0.4%, due to the additional cost of bleeding related complications.
This analysis supports international recommendations for the primary prevention of CVD and shows that, from an economic perspective, clinical concerns about GI bleeding or hemorrhagic stroke due to treatment with aspirin are less relevant in patients with no increased risk of GI bleeding. This latter group was excluded from individual studies included in the meta-analysis.3-7
The Framingham equation has been widely used both in Spain and throughout Europe, although it may overestimate coronary risk. Adaptations of the formula for use in Spain have appeared recently,23,24,26 together with the SCORE project, which is based on low and high risk European populations.13 Applying these new equations may lead to fewer indivudals being included in the high risk group (≥20% at 10 years), which would affect the budget impact of risk-modifying treatments, including low-dose aspirin. These equations were published after the present model was developed though they would not affect the results of the cost-effectiveness anaysis presented here, as the model is based on a hypothetical patient with a certain level of risk of suffering an event. Demographic characteristics are not taken into account in the cost-effectiveness analysis.
A limitation of the present study is that it used results from meta-analyses which in turn included different baseline risks of CHD, from different periods, and using different doses of aspirin (75-500 mg/day). As unpublished data relating to the meta-analyses and the individual studies on which they were based were unavailable some additional assumptions had to be made, such as that regarding the risk of death unrelated to CVD. Additionally, some costs (fatal events, follow-up) were obtained from patients with diabetes, which might have led to an overestimation of costs and, thereby, to an overestimation of the benefits of treatment with aspirin. Nevertheless, we believe that the results are valid as there are no data available which show that a fatal MI or stroke are more expensive in patients with diabetes, and because the authors studied presented treatment costs separately. These assumptions did not change the clinical results and the sensitivity analyses did not reveal any significant impact of these data on the costs obtained in the final results.17
In this analysis, the impact of low-dose aspirin may have been underestimated, as only the effects on non-fatal MI, fatal MI and death were assessed. But CHD also includes stable and unstable angina, though the meta-analyses of primary prevention did not include these 2 variables. Only 2 of the studies reviewed included the effect of treating angina with aspirin,4,7 and both showed fewer cases of angina in individuals who were taking aspirin, though the differences between treatments were not statistically significant.
CONCLUSIONS
Using low-dose aspirin for primary prevention in patients with a 10 year risk of ≥15% would lead to considerable cost savings for the Spanish NHS.
Studied financed by Bayer Healthcare AG.
Correspondence: Dra. C. Piñol.
Unidad de Farmacoeconomía y RR.II. Q.F.Bayer, S.A.
Pau Clarís, 196. 08037 Barcelona. España.
E-mail: carmen.pinol.cp@bayer.es
Received October 20, 2005.
Accepted for publication May 4, 2006.