Health care-associated infective endocarditis (HAIE) is a type of infective endocarditis (IE) with rising incidence and high mortality. Several studies have shown that these IEs have a different demographic and clinical profile than that of classic IEs seen in native or prosthetic valves (older age, more comorbidities, and different causative microorganisms).1–4 Although some studies have focused on HAIE and how it differs from other types of endocarditis,1–6 there are no articles analyzing the differences between the 2 subtypes of HAIE: nosocomial and nosohusial.
We decided to study the epidemiologic changes and relative incidence of HAIEs in the past 33 years at our hospital and the differences between nosocomial and nosohusial IEs in terms of clinical characteristics, treatment, and mortality. Cases of IE were considered nosocomial when they developed during a hospital stay or 2 months thereafter6 and nosohusial (nonnosocomial) when acquired outside the hospital after outpatient medical procedures (endoscopies, intravenous treatments, hemodialysis, catheter users, urinary catheterization, etc) within the following 2 months.6 Nosocomial or nosohusial IEs did not include IEs related to dental work or prosthetic valves not meeting any of the above criteria.
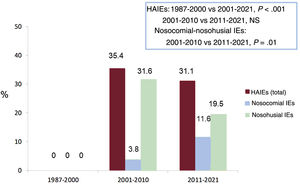
For the study, we assessed 512 consecutive cases diagnosed with IE at our hospital between 1987 and 2021, analyzing the relative incidence of both nosocomial and nosohusial HAIEs during 3 periods (1987-2000, 2001-2010, and 2011-2021), and we then compared the characteristics of nosocomial and nosohusial IEs. For the statistical analysis, the Student t test was used for quantitative variables and the chi-square test for proportions. The study was approved by the ethics committee of the hospital, and informed consent was given by all patients. In our series of 512 IE cases, 106 were HAIE (20.7% of all IEs), 27 were nosocomial (5.3% of all IEs and 25.5% of HAIEs), and 79 were nosohusial (15.4% of all IEs and 74.5% of HAIEs).
Figure 1 shows the percentage of HAIEs, nosocomial IEs, and nosohusial IEs throughout the study period. There were no cases of HAIE in 1987-2000, whereas IE cases represented 35.5% of all cases in 2001-2010 and 31.1% in 2011-2021 (P<.001). Nosocomial IEs rose significantly from 2001-2010 to 2011-2021, climbing from 3.8% to 31.6% of all IEs and from 10.7% to 37.3% of HAIEs (P=.01), whereas the percentage of nosohusial IEs remained essentially unchanged (11.6% and 19.5%, respectively, of all IEs and 89.3% and 62.7% of HAIEs).
Table 1 compares the characteristics of nosocomial and nosohusial IEs throughout the study period. There were no significant differences between the 2 groups in virtually any of the variables analyzed, with similar values for age, percentages of men and women, and types of IEs (native and prosthetic). The causal microorganisms were also the same, with Staphylococcus aureus being the most common in both groups (table 1). There were no differences in causal microorganisms for either type of HAIE between 2001-2010 and 2011-2021. Staphylococci caused 49.1% of all HAIEs in 2001-2010 (57.1% of nosocomial and 48.1% of nosohusial cases) and 48.9% in 2011-2021 (60% of nosocomial and 40% of nosohusial cases); streptococci, 11.5% (14.3% of nosocomial and 11.1% of nosohusial cases) in 2001-2010 and 11.1% (5% of nosocomial and 16% of nosohusial cases) in 2011-2021, and enterococci, 19.7% (14.3% of nosocomial and 20.6% of nosohusial cases) in 2001-2010 and 22.3% (25% of nosocomial and 20% of nosohusial cases) in 2011-2021. Most often the IE site was tricuspid in nosohusial IEs (17.7% vs 0%; P=.018), likely related to a tendency towards a greater percentage of hemodialysis as the portal of entry for this group (22.8% vs 7.4%; P=.077). Other diseases commonly seen along with nosohusial IEs were prior cancer (11.4%), immunosuppression (10.1%), diabetes mellitus (10.1%), chronic liver disease (8.9%), chronic bowel disease (6.3%), and kidney failure not treated by dialysis (table 1). The incidence of serious complications was high in both groups (66.7% and 69.6%, respectively). Surgery was performed during the active phase of the IE in 59.3% of nosocomial IEs and 56.9% of nosohusial IEs (no differences in the type of surgery between the 2 types), and early mortality was also similar between the groups (table 1). Early mortality was slightly higher in the 2011-2021 period in both groups, but with no differences between nosocomial and nosohusial IEs (25% vs 31.5% in 2001-2021 and 36.3% vs 39.1% in 2011-2021, not significant).
Comparison of the characteristics of nosocomial and nosohusial infective endocarditis cases in our setting (2001-2021)
| Nosocomial IEs (n = 27) | Nosohusial IEs (n = 79) | P | |
|---|---|---|---|
| Age, y | 67±11 | 66±15 | .542 |
| Women | 10 (37.1) | 35 (44.3) | .509 |
| Site | |||
| Aortic | 12 (44.5) | 22 (27.8) | .110 |
| Tricuspid | 0 | 14 (17.7) | .018 |
| Mitral | 15 (55.5) | 41 (51.9) | .742 |
| Pulmonary | 0 | 2 (2.6) | .403 |
| Type of EI | |||
| Native | 17 (62.9) | 50 (55.5) | .657 |
| Prosthetic | 10 (37.1) | 29 (44.5) | |
| Microorganisms | |||
| Staphylococcus aureus | 8 (29.6) | 22 (27.8) | .859 |
| Streptococcus epidermis | 7 (25.9) | 15 (18.9) | .442 |
| S viridans | 4 (14.8) | 9 (10.3) | .639 |
| Enterococci spp. | 5 (18.5) | 19 (21.1) | .553 |
| Other | 3 (11.2) | 12 (13.3) | .599 |
| Comorbidities | |||
| Diabetes mellitus | 4 (14.8) | 8 (10.1) | .506 |
| Cancer | 3 (11.2) | 9 (11.4) | .929 |
| Chronic hepatopathy | 4 (14.8) | 7 (8.9) | .381 |
| Immunosuppression | 3 (11.2) | 8 (10.1) | .869 |
| Severe kidney failure | 6 (22.5) | 21 (22.4) | .589 |
| Intestinal disease | 2 (7.4) | 5 (6.3) | .845 |
| Portal of entry | |||
| Hemodialysis | 2 (7.4) | 18 (22.8) | .077 |
| Intravascular catheter | 8 (29.6) | 16 (20.2) | .314 |
| Bladder catheter | 6 (22.2) | 10 (12.6) | .231 |
| Gastrointestinal endoscopy | 4 (14.8) | 19 (24.1) | .314 |
| Cardiac catheterization | 2 (7.4) | 6 (7.6) | .974 |
| Other | 3 (11.2) | 10 (12.6) | .832 |
| Serious complications | 18 (66.7) | 55 (69.6) | .774 |
| Total complicationsa | |||
| Heart failure | 12 (44.4) | 40 (48.7) | .578 |
| Neurological | 2 (7.4) | 6 (7.6) | .974 |
| Renal | 1 (3.7) | 2 (2.5) | .751 |
| Strokes | 5 (18.5 | 9 (11.4) | .345 |
| Abscesses | 5 (18.5) | 9 (11.4) | .345 |
| Mycotic aneurysms | 1 (3.7) | 0 | .085 |
| Surgery in active phaseb | 16 (59.3) | 45 (56.9) | .834 |
| Urgent/emergent | 3 (11.2) | 8 (10.1) | .973 |
| Elective | 13 (48.1) | 37 (46.8) | .906 |
| Early mortalityc | 9 (33.3) | 28 (35.4) | .842 |
| Total mortalityd | 10 (37.0) | 30 (38.0) | .930 |
IE, infective endocarditis.
The data are expressed as No. (%) or mean ± standard deviation.
Total complications: at least 1 of the following: heart failure, stroke or other neurologic complications, acute kidney failure with glomerular filtration rate <30mL/min/m2, embolic phenomena, abscesses in the myocardium or other regions, and mycotic aneurysms.
In conclusion, HAIEs represented a third of all IEs at our hospital in the past 2 decades, with nosohusial IEs generally predominant. However, a significant rise was seen in nosocomial IEs in recent years, most likely in relation to changes in the demographic and comorbidity profile of the inpatient population and the increase in the number of invasive procedures among these patients. Unlike other studies,5 we found no clinically or statistically significant differences between nosocomial and nosohusial IEs in the overall series or in the 2 time periods. In our experience, the microbiological profile and characteristics of these IEs are similar, indicating that treatment should not differ and that the prognosis does not necessarily vary in terms of complications or mortality. The mortality of the group studied is very high, probably due to the risk profile of the patients.
FUNDINGNo funding has been received.
AUTHORS’ CONTRIBUTIONSG. Heredia Campos wrote the scientific letter. G. Heredia Campos, A. Resúa Collazo, C. Fernández-Avilés, P. Anguita Gámez, J.C. Castillo Domínguez, and M. Anguita Sánchez collaborated in creating the database. P. Anguita Gámez, J.C. Castillo Domínguez, and M. Anguita Sánchez performed the statistical analysis. M. Anguita Sánchez supervised and directed the writing of the scientific letter.
CONFLICTS OF INTERESTNone.