The new hypertension (HTN) guidelines of the American College of Cardiology/American Heart Association (ACC/AHA)1 use lower blood pressure (BP) values than in previous guidelines2,3 (≥ 130/80mmHg) to define HTN and therapeutic targets. In the United States population this means an increase of 13.7% in patients diagnosed with HTN and 1.9% in those requiring pharmacological treatment; in addition, 14.4% of hypertensive patients on treatment will require treatment intensification.4 Our aim was to evaluate the potential impact of the new ACC/AHA guidelines in the general population of Toledo.
RICARTO is an observational epidemiological study of a cohort undergoing follow-up for a minimum of 5 years.5 The target population consist of patients aged 18 years or older in the Toledo health care area (n=424 172). Cardiovascular risk was calculated with the ASCVD Pooled Cohort Risk Equations Risk Calculator. The protocol was approved by the Complejo Hospitalario de Toledo Ethics Committee. BP was taken as the mean of 3 readings measured with an Omron HEM-907.
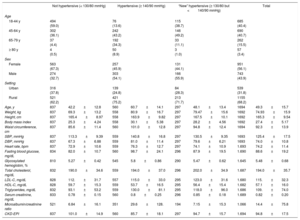
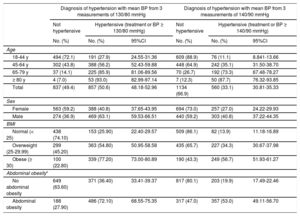
The study included 1694 patients (59.2% were women; mean age, 49.35±15.73 years). The epidemiological data are shown in Table 1. Patients with systolic BP between 130 and 140mmHg were younger and had less obesity than those with BP ≥ 140mmHg (P <.001). A total of 21.4% of patients were receiving treatment with antihypertensives (10.9% angiotensin II receptor blockers; 9.1%, diuretics; 7.1%, angiotensin-converting enzyme inhibitors; 4.6%, calcium channel blockers; 3.9%, beta blockers; 1.2%, alpha blockers). The prevalence of HTN according to the 2 criteria is shown in Table 2. The overall frequency of HTN was 33.1% and 50.6% depending on the criteria used, a difference of 17.5% (P <.001), representing a 52.9% increase. The difference was 22.3% (54.6% increase) in men and 13.8% in women (51.1% increase) (P <.001).
Characteristics of the Individuals Studied
| Not hypertensive (< 130/80 mmHg) | Hypertensive (≥ 140/90 mmHg) | “New” hypertensive (≥ 130/80 but <140/90 mmHg) | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Age | ||||||||
| 18-44 y | 494 (59.0) | 76 (13.6) | 115 (38.7) | 685 (40.4) | ||||
| 45-64 y | 302 (36.1) | 242 (43.2) | 146 (49.2) | 690 (40.7) | ||||
| 65-79 y | 37 (4.4) | 192 (34.3) | 33 (11.1) | 262 (15.5) | ||||
| ≥ 80 y | 4 (0.5) | 50 (8.9) | 3 (1.0) | 57 (3.4) | ||||
| Sex | ||||||||
| Female | 563 (67.3) | 257 (45.9) | 131 (44.1) | 951 (56.1) | ||||
| Male | 274 (32.7) | 303 (54.1) | 166 (55.9) | 743 (43.9) | ||||
| Setting | ||||||||
| Urban | 316 (37.8) | 139 (24.8) | 84 (28.3) | 539 (31.8) | ||||
| Rural | 521 (62.2) | 421 (75.2) | 213 (71.7) | 1155 (68.2) | ||||
| Age, y | 837 | 42.2±12.8 | 560 | 60.7±14.1 | 297 | 48.1±13.4 | 1694 | 49.3±15.7 |
| Weight, kg | 837 | 69.3±13.2 | 558 | 80.9±16.7 | 297 | 79.47±15.6 | 1692 | 74.93±15.9 |
| Height, cm | 837 | 165.4±8.97 | 558 | 163.9±9.82 | 297 | 167.5±10.1 | 1692 | 165.3±9.54 |
| Body mass index | 837 | 25.3±4.24 | 558 | 30.1±5.38 | 297 | 28.2±4.56 | 1692 | 27.4±5.17 |
| Waist circumference, cm | 837 | 85.6±11.4 | 560 | 101.0±12.8 | 297 | 94.8±12.4 | 1694 | 92.3±13.9 |
| SBP, mmHg | 837 | 113.3±9.39 | 559 | 140.8±16.8 | 297 | 130.5±9.35 | 1693 | 125.4±17.5 |
| DBP, mmHg | 837 | 67.3±6.88 | 559 | 81.0±11.4 | 297 | 79.6±6.21 | 1693 | 74.0±10.8 |
| Heart rate, bpm | 837 | 72.9±10.6 | 559 | 76.3±12.7 | 297 | 74.1±10.9 | 1.693 | 74.2±11.4 |
| Fasting blood glucose, mg/dL | 834 | 82.0±10.7 | 560 | 98.7±24.1 | 296 | 87.9±19.5 | 1.690 | 88.6±19.2 |
| Glycosylated hemoglobin, % | 810 | 5.27±0.42 | 545 | 5.8±0.86 | 290 | 5.47±0.62 | 1.645 | 5.48±0.68 |
| Total cholesterol, mg/dL | 832 | 190.0±34.6 | 559 | 194.0±37.0 | 296 | 202.0±34.9 | 1.687 | 194.0±35.7 |
| LDL-C, mg/dL | 828 | 112.±31.7 | 557 | 115.0±33.0 | 295 | 123.0±31.6 | 1.680 | 115.±32.3 |
| HDL-C, mg/dL | 828 | 59.7±15.3 | 559 | 53.7±16.5 | 295 | 56.4±15.4 | 1.682 | 57.1±16.0 |
| Triglycerides, mg/dL | 832 | 93.1±53.2 | 559 | 130.0±81.1 | 295 | 118.0±96.0 | 1.686 | 109.±74.0 |
| Serum creatinine, mg/dL | 833 | 0.78±0.15 | 560 | 0.8±0.25 | 296 | 0.85±0.18 | 1.689 | 0.82±0.20 |
| Microalbumin/creatinine ratio | 521 | 6.84±16.1 | 351 | 29.6±128. | 194 | 7.15±15.3 | 1.066 | 14.4±75.8 |
| CKD-EPI | 837 | 101.0±14.9 | 560 | 85.7±18.1 | 297 | 94.7±15.7 | 1.694 | 94.8±17.5 |
CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
Values are expressed as No. (%) or mean±standard deviation.
Frequency of Hypertension According to the 2 Criteria Used, in Different Ages and Types of Patients
| Diagnosis of hypertension with mean BP from 3 measurements of 130/80 mmHg | Diagnosis of hypertension with mean BP from 3 measurements of 140/90 mmHg | |||||
|---|---|---|---|---|---|---|
| Not hypertensive | Hypertensive (treatment or BP ≥ 130/80 mmHg) | Not hypertensive | Hypertensive (treatment or BP ≥ 140/90 mmHg) | |||
| No. (%) | No. (%) | 95%CI | No. (%) | No. (%) | 95%CI | |
| Age | ||||||
| 18-44 y | 494 (72.1) | 191 (27.9) | 24.55-31.36 | 609 (88.9) | 76 (11.1) | 8.841-13.66 |
| 45-64 y | 302 (43.8) | 388 (56.2) | 52.43-59.88 | 448 (64.9) | 242 (35.1) | 31.50-38.70 |
| 65-79 y | 37 (14.1) | 225 (85.9) | 81.06-89.56 | 70 (26.7) | 192 (73.3) | 67.48-78.27 |
| ≥ 80 y | 4 (7.0) | 53 (93.0) | 82.99-97.14 | 7 (12.3) | 50 (87.7) | 76.32-93.85 |
| Total | 837 (49.4) | 857 (50.6) | 48.18-52.96 | 1134 (66.9) | 560 (33.1) | 30.81-35.33 |
| Sex | ||||||
| Female | 563 (59.2) | 388 (40.8) | 37.65-43.95 | 694 (73.0) | 257 (27.0) | 24.22-29.93 |
| Male | 274 (36.9) | 469 (63.1) | 59.53-66.51 | 440 (59.2) | 303 (40.8) | 37.22-44.35 |
| BMI | ||||||
| Normal (< 25) | 438 (74.10) | 153 (25.90) | 22.40-29.57 | 509 (86.1) | 82 (13.9) | 11.18-16.89 |
| Overweight (25-29.99) | 299 (45.20) | 363 (54.80) | 50.95-58.58 | 435 (65.7) | 227 (34.3) | 30.67-37.98 |
| Obese (≥ 30) | 100 (22.80) | 339 (77.20) | 73.00-80.89 | 190 (43.3) | 249 (56.7) | 51.93-61.27 |
| Abdominal obesity* | ||||||
| No abdominal obesity | 649 (63.60) | 371 (36.40) | 33.41-39.37 | 817 (80.1) | 203 (19.9) | 17.49-22.46 |
| Abdominal obesity | 188 (27.90) | 486 (72.10) | 68.55-75.35 | 317 (47.0) | 357 (53.0) | 49.11-56.70 |
95%CI, 95% confidence interval; BMI, body mass index; BP, blood pressure.
In absolute terms, the impact was higher in obese patients: the frequency of HTN rose from 56.7% to 77.2% (a 20.5% difference; 36.1% increase) in obese patients and from 24.7% to 41.2% (16.5% difference; 66.8% increase) in nonobese patients (P <.001 for all differences). In overweight individuals, a similar effect to obese patients was observed, and the prevalence rose from 34.3% to 54.8% (20.5% difference; 59.8% increase). In patients with abdominal obesity, HTN rose from 53.0% to 72.1% (19.1% difference; 36% increase), similar to the findings for obese patients; in contrast, in those without abdominal obesity, the frequency of HTN rose from 19.9% to 36.4% (16.5% difference; 82.9% increase) (P <.001 for all differences).
The estimated cardiovascular risk was ≥ 10% in 30.8% of the population (46.8% in hypertensive individuals and 7.1% in nonhypertensive individuals). In normotensive patients who would be hypertensive according to the new guidelines, 3.9% (2.2% of women and 6.1% of men) had a risk ≥ 10%. Furthermore, 54.8% of the 464 hypertensive patients who were well-controlled (BP <140/90mmHg) would become poorly-controlled with BP <130/80mmHg (P <.001).
This study demonstrates that the use of the ACC/AHA guidelines on HTN in this sample of the Spanish population would result in a significant 17.5% increase in the frequency of HTN, with this increase being higher in male patients (22.3%), and those who are obese (20.5%), overweight (20.5%) or have abdominal obesity (19.1%). Due to a high cardiovascular risk, 3.9% of the “new” hypertensive patients would require pharmacological treatment. More than half (55%) of patients currently controlled on treatment would require intensification of their antihypertensive treatment to be controlled according to the new guidelines.
The lower BP levels recommended by the new 2017 ACC/AHA guidelines are based on randomized and observational studies. The observational data demonstrated a gradual increase in mortality as BP increased beyond levels of> 115/75mmHg, and the studies carried out on treatment in hypertensive patients reported a reduction in morbidity and mortality at systolic BP levels <130mmHg. In the SPRINT study they demonstrated that in hypertensive patients with high risk, intensive treatment (BP 121/69mmHg) reduced morbidity and mortality vs standard treatment (BP 136/76mmHg).6
The ACC/AHA guidelines indicate a prevalence of BP between ≥ 130/80 and ≥ 140/90mmHg of 14%,1 very similar to the findings by Muntner et al.4 (13.7%) and our findings (17.5%). In the United States population, the proportion of hypertensive patients requiring treatment intensification to reach the new targets was 14.4%, somewhat different to the 55% found in this study. We consider these figures to be relevant, at a time when, as some authors have pointed out, hypertension may need to be redefined and its treatment improved.
FUNDINGThe RICARTO study was funded from 2011 to 2013 by the government of Castile-La Mancha with a grant for Research in Biomedicine and Health Sciences (record no. PI-2010/043) from the Castile-La Mancha Social and Healthcare Foundation (FISCAM).
The Spanish Society of Primary Care Physicians (Fundación SERMERGEN) assisted in funding the RICARTO study from 2013 with an unconditional grant.