The hybrid algorithm was designed to assist with initial and subsequent crossing strategy selection in chronic total occlusion (CTO) percutaneous coronary interventions (PCIs). However, the success of the initially selected strategy has received limited study.
MethodsWe examined the impact of adherence to the hybrid algorithm recommendation for initial CTO crossing technique selection in 4178 CTO PCIs from a large multicenter registry.
ResultsThe initial crossing strategy was concordant with the hybrid algorithm recommendation in 1833 interventions (44%). Patients in the concordant group had a similar age to those in the discordant group but a lower mean J-CTO score (2.0 ± 1.4 vs 2.8 ± 1.1; P < .01). The concordant group showed higher technical success with the first crossing strategy (68% vs 48%; P < .01) and higher overall technical success (88% vs 83%; P < .01) with no difference in the incidence of in-hospital major adverse events (1.8% vs 2.3%; P = .26). In multivariable analysis, after adjustment for age, prior myocardial infarction, prior PCI, prior coronary artery bypass grafting, J-CTO score, and scheduled CTO PCI, nonadherence to the hybrid algorithm was independently associated with lower technical success of the initial crossing strategy (odds ratio, 0.55; 95% confidence interval, 0.48-0.64; P < .01).
ConclusionsAdherence to the hybrid algorithm for initial crossing strategy selection is associated with higher CTO PCI success but similar in-hospital major adverse cardiac events.
Keywords
The aim of the 2012 hybrid algorithm for chronic total occlusion (CTO) percutaneous coronary intervention (PCI)1 is to use lesion characteristics to guide selection of the initial and subsequent CTO crossing strategies. After dual injection, 4 angiographic characteristics are evaluated and used to select the optimal initial crossing strategy: a) proximal cap ambiguity, b) distal vessel quality, c) presence of interventional collateral vessels, and d) lesion length. Use of the hybrid algorithm has been associated with high technical success (89%-95%),2–5 with the initially selected crossing strategy being successful in 55% to 60% of interventions.3,5 No studies have assessed whether use of the hybrid algorithm-suggested initial crossing technique is associated with higher technical success.
We analyzed a large multicenter registry to determine the impact of adherence to the hybrid algorithm recommendation on in-hospital outcomes of CTO PCI.
METHODSBetween January 2012 and October 2019, 5748 CTO PCIs were performed at 28 centers in the US, Europe, Canada, and Asia and were included in the PROGRESS-CTO registry (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention, NCT02061436). All participating centers were high-volume centers performing at least 40 CTO PCIs per year. After the exclusion of procedures with missing data on proximal cap ambiguity, distal cap quality, presence of interventional collaterals, and lesion length, as well as procedures in which more than 1 CTO PCI was attempted, 4178 CTO PCIs remained and were included in the present analysis.
Coronary CTOs were defined as coronary lesions with Thrombolysis in Myocardial Infarction (TIMI) grade 0 flow of at least 3 months duration. Occlusion duration was clinically estimated based on the first onset of angina, prior history of myocardial infarction (MI) in the target vessel territory, or comparison with a prior angiogram. Calcification was assessed by angiography as mild (spots), moderate (involving ≤ 50% of the reference lesion diameter), and severe (involving > 50% of the reference lesion diameter). Moderate proximal vessel tortuosity was defined as the presence of at least 2 bends > 70° or 1 bend > 90° in the CTO vessel and severe tortuosity as 2 bends > 90° or 1 bend > 120°. The proximal cap was considered ambiguous when there was uncertainty about its location and its shape. Interventional collaterals were defined as collaterals considered amenable to crossing by a guidewire and a microcatheter by the operator before an attempt to cross them was made. The distal landing zone was considered of poor quality when it was less than 2mm in diameter and/or was diffusely diseased.
Antegrade wire escalation (AWE) was defined as an antegrade PCI during which the guidewire crossed the lesion from the “true to true” lumen. Antegrade dissection/re-entry (ADR) was defined as an antegrade PCI during which a guidewire was intentionally introduced into the subintimal space proximal to the lesion or during which re-entry into the distal true lumen was attempted following intentional or inadvertent subintimal guidewire or device crossing. A procedure was defined as “retrograde” if an attempt was made to cross the lesion through a collateral vessel or bypass graft supplying the target vessel distal to the lesion.
Technical success was defined as successful CTO revascularization with achievement of < 30% residual diameter stenosis within the treated segment and restoration of TIMI grade 3 antegrade flow. Procedural success was defined as the achievement of technical success without any in-hospital major adverse cardiac events (MACEs). In-hospital MACEs included any of the following adverse events prior to hospital discharge: death, MI, recurrent symptoms requiring urgent repeat target vessel revascularization with PCI or coronary artery bypass grafting (CABG), tamponade requiring either pericardiocentesis or surgery, and stroke. MI was defined using the Fourth Universal Definition of Myocardial Infarction (type 4 MI).6 The Japan-Chronic Total Occlusion (J-CTO) score was calculated as described by Morino et al.,7 the PROGRESS-CTO score as described by Christopoulos et al.,8 and the PROGRESS-CTO Complications score as described by Danek et al.9
Adherence of the initial crossing technique to the hybrid algorithm recommendation was assessed as follows. a) The retrograde approach had to be the initial strategy if all 3 criteria were met (proximal cap ambiguity, poor distal landing zone, and presence of interventional collaterals). When none of the criteria were satisfied or when interventional collaterals were present but the proximal cap was not ambiguous and the distal zone was of good quality, the initial crossing strategy had to be antegrade. If the proximal cap was ambiguous or a poor distal landing zone was present or 2 of any of the 3 criteria were satisfied, either antegrade or retrograde crossing was considered concordant with the hybrid algorithm. b) In patients with a lesion length > 20mm that were allowed an initial antegrade crossing strategy by the hybrid algorithm, the initial crossing strategy had to be ADR. c) When the lesion length was ≤ 20mm and an initial antegrade crossing strategy was considered concordant with the hybrid algorithm, the initial crossing strategy had to be AWE.
Statistical analysisCategorical variables are expressed as percentages and were compared using Pearson chi-square test or 2-tail Fisher exact test. Continuous variables are presented as mean ± standard deviation or median [interquartile range], unless otherwise specified, and were compared using t test or Wilcoxon rank-sum test, as appropriate. Multivariable logistic regression was used to examine the association between adherence to the hybrid algorithm recommendation for initial crossing technique selection and technical success with the first crossing strategy and overall technical success. Variables associated with technical success with the first crossing strategy and overall technical success in univariable analysis (P < .10) were included in the model. Specifically, age, prior MI, prior PCI, prior CABG, J-CTO, scheduled (non-ad hoc) PCI, and nonadherence to the hybrid algorithm were included in the multivariable logistic regression model of technical success with the first crossing strategy. Age, prior MI, prior PCI, prior CABG, J-CTO, and nonadherence to the hybrid algorithm were included in the multivariable logistic regression model for technical success. All statistical analyses were performed with JMP 14.0 (SAS Institute, Cary, North Carolina, United States). A 2-sided P value of .05 was considered statistically significant.
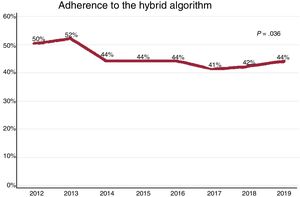
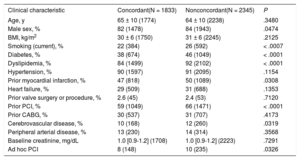
RESULTSThe initial crossing strategy was concordant with the hybrid algorithm recommendation in 1833 of the 4178 procedures (44%). Adherence to the hybrid algorithm did not increase over time (figure 1). The clinical characteristics of the study patients are shown in Table 1. Compared with the discordant group, patients in the concordant group had a similar age but were less likely to have diabetes (38% vs 46%; P < .01) or prior PCI (59% vs 66%; P < .01) and had higher left ventricular ejection fraction (55% [45%-60%] vs 52% [40%-60%]; P < .01).
Clinical characteristics of the study patients, classified according to adherence to the hybrid algorithm for selection of the initial crossing strategy
| Clinical characteristic | Concordant(N = 1833) | Nonconcordant(N = 2345) | P |
|---|---|---|---|
| Age, y | 65 ± 10 (1774) | 64 ± 10 (2238) | .3480 |
| Male sex, % | 82 (1478) | 84 (1943) | .0474 |
| BMI, kg/m2 | 30 ± 6 (1750) | 31 ± 6 (2245) | .2125 |
| Smoking (current), % | 22 (384) | 26 (592) | < .0007 |
| Diabetes, % | 38 (674) | 46 (1049) | < .0001 |
| Dyslipidemia, % | 84 (1499) | 92 (2102) | < .0001 |
| Hypertension, % | 90 (1597) | 91 (2095) | .1154 |
| Prior myocardial infarction, % | 47 (818) | 50 (1089) | .0308 |
| Heart failure, % | 29 (509) | 31 (688) | .1353 |
| Prior valve surgery or procedure, % | 2.6 (45) | 2.4 (53) | .7120 |
| Prior PCI, % | 59 (1049) | 66 (1471) | < .0001 |
| Prior CABG, % | 30 (537) | 31 (707) | .4173 |
| Cerebrovascular disease, % | 10 (168) | 12 (260) | .0319 |
| Peripheral arterial disease, % | 13 (230) | 14 (314) | .3568 |
| Baseline creatinine, mg/dL | 1.0 [0.9-1.2] (1708) | 1.0 [0.9-1.2] (2223) | .7291 |
| Ad hoc PCI | 8 (148) | 10 (235) | .0326 |
BMI, body mass index; CABG, coronary artery bypass grafting; CAD, coronary artery disease; PCI, percutaneous coronary intervention.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Numbers in parentheses refer to the number of patients.
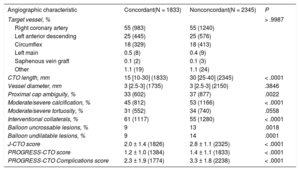
The angiographic characteristics of the study lesions are shown in Table 2. The J-CTO (2.0 ± 1.4 vs 2.8 ± 1.1; P < .01), PROGRESS-CTO (1.2 ± 1.0 vs 1.4 ± 1.1; P < .01), and PROGRESS-CTO Complications (2.3 ± 1.9 vs 3.3 ± 1.8; P < .01) scores were lower in the concordant group than in the discordant group.
Angiographic characteristics of the study lesions, classified according to adherence to the hybrid algorithm for selection of the initial crossing strategy
| Angiographic characteristic | Concordant(N = 1833) | Nonconcordant(N = 2345) | P |
|---|---|---|---|
| Target vessel, % | > .9987 | ||
| Right coronary artery | 55 (983) | 55 (1240) | |
| Left anterior descending | 25 (445) | 25 (576) | |
| Circumflex | 18 (329) | 18 (413) | |
| Left main | 0.5 (8) | 0.4 (9) | |
| Saphenous vein graft | 0.1 (2) | 0.1 (3) | |
| Other | 1.1 (19) | 1.1 (24) | |
| CTO length, mm | 15 [10-30] (1833) | 30 [25-40] (2345) | < .0001 |
| Vessel diameter, mm | 3 [2.5-3] (1735) | 3 [2.5-3] (2150) | .3846 |
| Proximal cap ambiguity, % | 33 (602) | 37 (877) | .0022 |
| Moderate/severe calcification, % | 45 (812) | 53 (1166) | < .0001 |
| Moderate/severe tortuosity, % | 31 (552) | 34 (740) | .0558 |
| Interventional collaterals, % | 61 (1117) | 55 (1280) | < .0001 |
| Balloon uncrossable lesions, % | 9 | 13 | .0018 |
| Balloon undilatable lesions, % | 9 | 14 | .0001 |
| J-CTO score | 2.0 ± 1.4 (1826) | 2.8 ± 1.1 (2325) | < .0001 |
| PROGRESS-CTO score | 1.2 ± 1.0 (1384) | 1.4 ± 1.1 (1833) | < .0001 |
| PROGRESS-CTO Complications score | 2.3 ± 1.9 (1774) | 3.3 ± 1.8 (2238) | < .0001 |
CTO, chronic total occlusion; J-CTO, Japan-Chronic Total Occlusion; PROGRESS-CTO, Prospective Global Registry of Chronic Total Occlusion Interventions.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Numbers in parentheses refer to the number of patients.
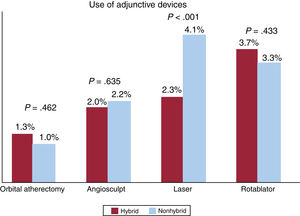
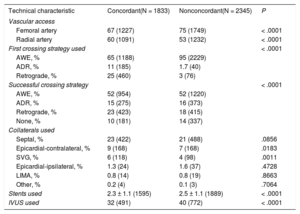
The techniques used for CTO crossing are presented in table 3. The most common first crossing strategy in the concordant group was AWE (65%), followed by retrograde (25%) and ADR (11%), whereas AWE was the initially attempted crossing technique in 95% of the interventions in the discordant group (figure 2A,B). If the hybrid algorithm had been followed in the discordant group for the CTO PCIs in which AWE was inappropriately the first crossing strategy, ADR and the retrograde approach would have been the initial crossing technique in 41% and 9% of procedures, respectively, whereas, for the remaining interventions, either ADR or the retrograde approach would have been the first crossing strategy (figure 2C). AWE was the most common final crossing technique in both groups (52%). In contrast, the retrograde approach was more likely to be the successful crossing technique for the concordant group (23% vs 18%; P < .01). A lower number of crossing strategies was used in the concordant group (1.3 ± 0.6 vs 1.6 ± 0.7; P < .01). The use of adjunctive devices for lesion preparation was similar in the 2 groups (8% vs 9%; P = .08) (figure 3). However, laser was used more often in the discordant group (2.3% vs 4.1%; P < .01).
Technical characteristics of the study procedures, classified according to adherence to the hybrid algorithm for selection of the initial crossing strategy
| Technical characteristic | Concordant(N = 1833) | Nonconcordant(N = 2345) | P |
|---|---|---|---|
| Vascular access | |||
| Femoral artery | 67 (1227) | 75 (1749) | < .0001 |
| Radial artery | 60 (1091) | 53 (1232) | < .0001 |
| First crossing strategy used | < .0001 | ||
| AWE, % | 65 (1188) | 95 (2229) | |
| ADR, % | 11 (185) | 1.7 (40) | |
| Retrograde, % | 25 (460) | 3 (76) | |
| Successful crossing strategy | < .0001 | ||
| AWE, % | 52 (954) | 52 (1220) | |
| ADR, % | 15 (275) | 16 (373) | |
| Retrograde, % | 23 (423) | 18 (415) | |
| None, % | 10 (181) | 14 (337) | |
| Collaterals used | |||
| Septal, % | 23 (422) | 21 (488) | .0856 |
| Epicardial-contralateral, % | 9 (168) | 7 (168) | .0183 |
| SVG, % | 6 (118) | 4 (98) | .0011 |
| Epicardial-ipsilateral, % | 1.3 (24) | 1.6 (37) | .4728 |
| LIMA, % | 0.8 (14) | 0.8 (19) | .8663 |
| Other, % | 0.2 (4) | 0.1 (3) | .7064 |
| Stents used | 2.3 ± 1.1 (1595) | 2.5 ± 1.1 (1889) | < .0001 |
| IVUS used | 32 (491) | 40 (772) | < .0001 |
ADR, antegrade dissection/re-entry; AWE, antegrade wire escalation; IVUS, intravascular ultrasound; LIMA, left internal mammary artery; SVG, saphenous vein graft.
Data are expressed as No. (%) or mean ± standard deviation.
Numbers in parentheses refer to the number of patients.
A: crossing strategies followed in procedures concordant with the hybrid algorithm, and B: procedures in which the hybrid algorithm was not followed. C: illustration of crossing techniques that would have been used as the initial crossing technique if operators had followed the hybrid algorithm in the discordant group. ADR, antegrade dissection re-entry; AWE, antegrade wire escalation; CTO, chronic total occlusion; J-CTO, Japanese-Chronic Total Occlusion; PCI, percutaneous coronary intervention.
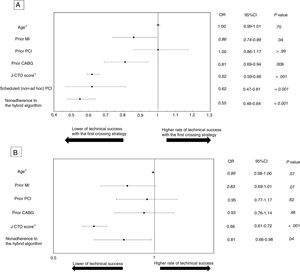
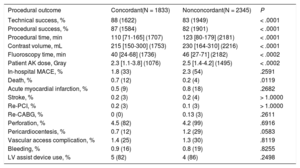
Procedural outcomes are described in table 4. Technical success with the initial crossing strategy was more frequently achieved in the concordant group than in the discordant group (68% vs 48%; P < .01). Overall technical success (88% vs 83%; P < .01) and procedural success (87% vs 82%; P < .01) were both higher in the concordant group whereas there was no difference in in-hospital MACE rates. Perforation incidence was also similar in the 2 groups (4.5% vs 4.2%; P = .692). The crossing strategy causing the perforation was specified in 113 of the 181 perforations: retrograde crossing was the most common technique implicated (n = 53), followed by AWE (n = 51) and ADR (n = 9). In multivariable analysis, after adjustment for age, prior MI, prior PCI, prior CABG, J-CTO score, and non-ad hoc CTO PCI, nonadherence to the hybrid algorithm was independently associated with lower technical success with the initial crossing strategy (odds ratio, 0.55; 95% confidence interval, 0.48-0.64; P < .01) (figure 4A). Similarly, in a second multivariable analysis, nonadherence to the hybrid algorithm was independently associated with lower overall technical success (odds ratio, 0.81; 95% confidence interval, 0.66-0.98; P = .04) (figure 4B). The effect of nonadherence to the hybrid algorithm on technical success with the first crossing strategy was dependent on the J-CTO score (P < .001), whereas the interaction between the J-CTO score and nonadherence was not significant for overall technical success (P = .912). In CTO PCIs in which in-hospital death occurred, the retrograde approach was attempted in 13 of the 16 interventions, followed by AWE (8 of 16) and ADR (5 of 16) and it was the first crossing strategy in 9 of the procedures. In-hospital death more frequently occurred in interventions in which retrograde crossing was the first crossing technique (1.7% vs 0.9% vs 0.2% with retrograde, ADR, and AWE, respectively; P < .001). Among retrograde cases, septal collaterals were used for crossing in 8, epicardial collaterals in 5, and saphenous vein grafts in 2. The techniques used after successful collateral crossing were reverse controlled antegrade and retrograde tracking (CART) (9), guide catheter extension reverse CART (1), knuckle wire technique (1), and true-to-true-lumen (1).
Procedural outcomes of the study procedures, classified according to adherence to the hybrid algorithm for selection of the initial crossing strategy
| Procedural outcome | Concordant(N = 1833) | Nonconcordant(N = 2345) | P |
|---|---|---|---|
| Technical success, % | 88 (1622) | 83 (1949) | < .0001 |
| Procedural success, % | 87 (1584) | 82 (1901) | < .0001 |
| Procedural time, min | 110 [71-165] (1707) | 123 [80-179] (2181) | < .0001 |
| Contrast volume, mL | 215 [150-300] (1753) | 230 [164-310] (2216) | < .0001 |
| Fluoroscopy time, min | 40 [24-68] (1736) | 46 [27-71] (2182) | < .0002 |
| Patient AK dose, Gray | 2.3 [1.1-3.8] (1076) | 2.5 [1.4-4.2] (1495) | < .0002 |
| In-hospital MACE, % | 1.8 (33) | 2.3 (54) | .2591 |
| Death, % | 0.7 (12) | 0.2 (4) | .0119 |
| Acute myocardial infarction, % | 0.5 (9) | 0.8 (18) | .2682 |
| Stroke, % | 0.2 (3) | 0.2 (4) | > 1.0000 |
| Re-PCI, % | 0.2 (3) | 0.1 (3) | > 1.0000 |
| Re-CABG, % | 0 (0) | 0.13 (3) | .2611 |
| Perforation, % | 4.5 (82) | 4.2 (99) | .6916 |
| Pericardiocentesis, % | 0.7 (12) | 1.2 (29) | .0583 |
| Vascular access complication, % | 1.4 (25) | 1.3 (30) | .8119 |
| Bleeding, % | 0.9 (16) | 0.8 (19) | .8255 |
| LV assist device use, % | 5 (82) | 4 (86) | .2498 |
AK, air kerma; CABG, coronary artery bypass grafting; LV, left ventricular; MACE, major adverse cardiac event; Re-PCI, repeated percutaneous coronary intervention.
Data are expressed as No. (%) or median [interquartile range].
Numbers in parentheses refer to the number of patients.
A: multivariable analysis of technical success with the first crossing strategy. B: multivariable analysis of overall technical success. 95%CI, 95% confidence interval; CABG, coronary artery bypass grafting; MI, myocardial infarction; J-CTO, Japanese-Chronic Total Occlusion; OR, odds ratio; PCI, percutaneous coronary intervention. *Estimates for age and J-CTO score are provided by a 1-year or 1-point change, respectively.
Six deaths were attributed to perforation, the most common cause of death. Retrograde crossing was the technique causing the perforation in 3 of these cases, as well as AWE in 1, ADR in 1, and both retrograde crossing and ADR in the last 1 (the technique leading to perforation in that patient was not specified). Other causes of death were cardiogenic shock (n = 4), hemorrhagic shock (n = 2), periprocedural MI (n = 1), multiple organ failure (n = 1), and ischemic bowel after a prolonged ICU stay post-salvage PCI (n = 1); 1 death was described as cardiovascular without further specification. The concordant group showed a lower procedural time (110 [71-165] vs 123 [80-179] minutes; P < .01), contrast volume (215 [150-300] vs 230 [164-310] mL; P < .01), and air kerma radiation dose (2.3 [1.1-3.8] vs 2.5 [1.4-4.2] Gray; P < .01).
DISCUSSIONThe major findings of our study are that adherence to the hybrid algorithm for the selection of the initial CTO crossing strategy a) occurred in slightly less than 50% of CTO PCIs and in less complex lesions and was associated with b) higher use of the retrograde approach, c) higher technical success of the first crossing strategy and higher overall technical success, and d) similar rates of in-hospital MACEs compared with interventions in which the hybrid algorithm was not followed for initial crossing strategy selection.
There are several potential explanations for the 44% adherence to the hybrid algorithm recommendation in the study patients. First, equipment availability varies from site to site. For example, the CrossBoss catheter and the Stingray Device (Boston Scientific) are not available at many locations.10 In addition, although ADR use is high in Europe and the US (used in 23%-58% of cases), it is used in less than 2% of cases in Japan.5,11–14 Second, the potential risk of each approach varies. For example, even if the hybrid algorithm recommends retrograde as the first approach, the risk may be high if epicardial collaterals are used, compelling the operator to attempt antegrade crossing. Operator experience is critical for both initial and subsequent technique selection and clinical judgment cannot be replaced by an algorithm.
In the present study, ad hoc procedures were more common in the discordant group than in the concordant group. Previous work showed that AWE was the first crossing strategy in the overwhelming majority of interventions when CTO PCI was performed as an ad hoc procedure, in contrast to planned CTO PCI (91% vs 76%; P < .001).15 Adequate planning is critical for CTO interventions.16 Ad hoc CTO PCI probably does not allow enough time for a thorough lesion study and less challenging strategies are thus preferred for the initial crossing. In addition, angiographic characteristics that are not captured by the hybrid algorithm, such as moderate/severe calcification, which was more prevalent in the discordant group, have been associated with higher risk of perforation and could have discouraged the operators from attempting ADR or retrograde crossing.17,18 Furthermore, it is likely that, due to the higher “risk profile” of patients in the discordant group, who more often had diabetes and had a lower left ventricular ejection fraction, operators were reluctant to use techniques requiring more contrast and a longer procedural time.19 Finally, it is plausible that many interventionalists preferred to start crossing attempts by trying AWE, even briefly, before escalating to more complex techniques.
Several CTO crossing algorithms have been proposed.20–22 The Asia Pacific algorithm emphasizes coronary artery computed tomography (CCTA) assessment, along with conventional angiography and intravascular ultrasound-guided entry, in patients with proximal cap ambiguity because it may be superior to angiography for the analysis of proximal cap ambiguity.21,23 The modified hybrid algorithm proposed by the EuroCTO Club is more granular, incorporating even specific devices, but thus more complicated.20 The most recent algorithm published by a panel of Japanese CTO PCI experts focuses not only on the characteristics of the lesion, but also on the duration of guidewire manipulation, proposing a limit of 20minutes for a switch from primary antegrade crossing to another technique. Furthermore, this algorithm suggests that termination of the intervention should be considered after 3hours of guidewire manipulation.24
A recent global expert consensus document for CTO PCI concluded that antegrade crossing should generally be preferred over retrograde crossing as the initial crossing strategy, because of the higher risk of complications with the latter. However, the retrograde approach remains critical in cases of blunt stump or proximal cap ambiguity that cannot be clarified with other modalities, such as intravascular ultrasound and CCTA.16
Our study demonstrated higher use of the retrograde approach when the hybrid algorithm was followed, which may partly explain the higher success rates achieved. Retrograde techniques have significantly contributed to the increased technical success in CTO PCI.25,26 They are especially useful in more complex subsets, such as in patients with prior CABG in whom the use of saphenous vein grafts for retrograde crossing increases the chance for successful recanalization of flush aorto-ostial occlusions, many of which are only approachable via retrograde crossing.27,28 On the other hand, while the hybrid group had a lower PROGRESS-CTO Complications score and the 2 groups had similar rates of in-hospital MACEs, mortality was higher in the concordant group, a finding that is likely related to higher use of retrograde crossing as the first crossing strategy in this group, an approach associated with a higher rate of in-hospital death in our analysis.19 Use of the retrograde approach is currently decreasing.29,30 In our results, laser was used more frequently when the hybrid algorithm was not followed due to the higher rate of balloon undilatable and uncrossable lesions compared with the concordant group.
LimitationsOur study has a number of limitations. PROGRESS-CTO is an observational retrospective study without core laboratory assessment of the study angiograms or clinical event adjudication. The procedures were performed in dedicated, high-volume CTO centers by experienced operators, limiting extrapolation to less experienced operators and lower volume centers.
CONCLUSIONSAdherence to the hybrid algorithm recommendation for initial crossing strategy for CTO PCI is associated with higher technical success and similar in-hospital MACEs.
FUNDINGThe PROGRESS-CTO registry has received support from the Abbott Northwestern Hospital Foundation, Minneapolis, Minnesota.
CONFLICTS OF INTERESTK. Alaswaad indicates consulting fees from Terumo and Boston Scientific and has worked as an unpaid consultant for Abbott Laboratories. J.J. Khatri indicates research grant support from Asahi Intecc and speaking/proctor fees from Abbott Vascular. F.A. Jaffer indicates consulting fees from Abbott Vascular, Boston Scientific, and Siemens and has received research grants from Canon, Siemens, and the National Institutes of Health. M. Patel indicates speakers bureau for Astra Zeneca. E. Mahmud indicates consulting fees from Medtronic and Corindus; speaker's fees from Medtronic, Corindus, and Abbott Vascular; educational program fees from Abbott Vascular; and clinical events committee fees from St. Jude. B.K. Jefferson indicates honoraria/consulting/speaking fees from Abbott, Boston Scientific, CSI, and Medtronic. R.W. Yeh indicates a career development award (1K23HL118138) from the National Heart, Lung, and Blood Institute. B.V. Rangan indicates research grants from InfraReDx Inc and The Spectranetics Corporation. S. Garcia indicates consulting fees from Medtronic. S. Banerjee indicates research grants from Gilead and the Medicines Company, consultant/speaker honoraria from Covidien and Medtronic, ownership in MDCARE Global (spouse), and intellectual property in HygeiaTel. M.N. Burke indicates consulting and speaker honoraria from Abbott Vascular and Boston Scientific. D. Karmpaliotis indicates speaker honoraria from Abbott Vascular, Boston Scientific, Medtronic, and Vascular Solutions. E.S. Brilakis indicates consulting/speaker honoraria from Abbott Vascular, the American Heart Association (associate editor Circulation), Biotronik, Boston Scientific, the Cardiovascular Innovations Foundation (Board of Directors), CSI, Elsevier, InfraRedx, GE Healthcare, Siemens, Teleflex, and Medtronic; research support from Siemens, Regeneron, and Osprey; and is a shareholder in MHI Ventures. All other co-authors have nothing to disclose.
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the Minneapolis Heart Institute Foundation (MHIF), Minneapolis, Minnesota. REDCap is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.