To analyze the association between the development of network systems of care for ST-segment elevation myocardial infarction (STEMI) in the autonomous communities (AC) of Spain and the regional rate of percutaneous coronary intervention (PCI) and in-hospital mortality.
MethodsFrom 2003 to 2012, data from the minimum basic data set of the Spanish taxpayer-funded health system were analyzed, including admissions from general hospitals. Diagnoses of STEMI and related procedures were codified by the International Diseases Classification. Discharge episodes (n = 302 471) were distributed in 3 groups: PCI (n = 116 621), thrombolysis (n = 46 720), or no reperfusion (n = 139 130).
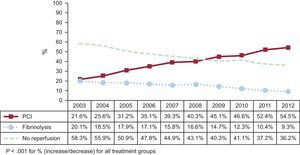
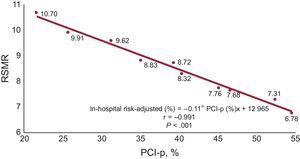
ResultsCrude mortality throughout the evaluation period was higher for the no-PCI or thrombolysis group (17.3%) than for PCI (4.8%) and thrombolysis (8.6%) (P < .001). For the aggregate of all communities, the PCI rate increased (21.6% in 2003 vs 54.5% in 2012; P < .001) with a decrease in risk-standardized mortality rates (10.2% in 2003; 6.8% in 2012; P < .001). Significant differences were observed in the PCI rate across the AC. The development of network systems was associated with a 50% increase in the PCI rate (P < .001) and a 14% decrease in risk-standardized mortality rates (P < .001).
ConclusionsFrom 2003 to 2012, the PCI rate in STEMI substantially increased in Spain. The development of network systems was associated with an increase in the PCI rate and a decrease in in-hospital mortality.
Keywords
Primary percutaneous coronary intervention (PCI) is the preferred reperfusion strategy in patients with ST-segment elevation myocardial infarction (STEMI) if performed by an experienced team within the first 120minutes after the first medical contact. To offer the best reperfusion strategy to the highest proportion of patients within the recommended time intervals, current guidelines recommend the need for optimal organization of STEMI systems of care at the community, regional and national level.1 However, the implementation of these reperfusion networks is strongly influenced by several regional factors such as transport times, the availability of resources and infrastructure, and the characteristics of health care systems.2,3 The heterogeneity of the economic situation and structure of health care systems has led to substantial differences in the current organization of reperfusion networks for STEMI patients across different geographical areas in the world.
During the last few decades, multiple issues regarding the effectiveness of advances in the medical management of STEMI patients have been resolved. However, little information is available on the impact of health care policies on clinical outcomes in patients with heart diseases. There is a wide variation in medical treatment and outcomes among patients with acute myocardial infarction across different countries, as well as between different regions within countries.4,5 In Spain, the RECALCAR study6 documented lower in-hospital mortality in patients with acute myocardial infarction admitted to hospitals with cardiology departments and a higher level of technological development. Spain is politically integrated into 17 different geographic regions (autonomous communities [AC]), each with independent political power over its budget and with the capacity to organize and develop its own health system.
The aim of this study was to analyze, throughout the period from 2003 to 2012, the association between the development of different systems of care for STEMI patients in the AC of Spain, the regional rate of PCI, and in-hospital STEMI mortality. The Spanish taxypayer-funded health system provides an ideal setting for analyzing the impact of different approaches to STEMI treatment: the country has a highly homogeneous population, with different policies being applied to patients with STEMI from the different AC, and a national centralized registry of hospital discharges.
METHODSFor a more detailed description of the methodology used, the reader can consult the .
PopulationWe evaluated the data from the minimum basic data set of the Spanish taxpayer-funded health system, which includes admissions from general hospitals from 2003 to 2012. We used the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) diagnostic codes 410.0x, 410.1x, 410.2x, 410.3x, 410.4x, 410.5x, 410.6x, and 410.8x to identify all patients with a main diagnosis of STEMI (n = 326 144). We chose the main diagnosis because it is considered the primary reason for hospital admission. A total of 23 670 discharges were excluded because of age lower than 35 or higher than 95 years, obstetric discharges, and transfers to other hospitals in the first 2 days of admission to avoid duplicate episodes of patients transferred to other hospitals after PCI.7 The 302 471 discharge episodes remaining after exclusions were distributed in 3 groups depending on clinical management: PCI (n = 116 621), thrombolysis (n = 46 720) or no-PCI or thrombolysis (n = 139 130).
The AC of Spain are different geographic regions with independent political power over their budgets and organization and management of the public health care. Consequently, the Spanish taxpayer-funded health system is decentralized in “autonomous community health services” (ACHS). Almost all (98.4%) of the Spanish population is covered by the publicly-funded health system. There are 17 AC with populations that range from 300 000 to 8 million inhabitants.8 In this study, we included the 16 ACHS with the capability to deliver PCI treatment during the study period. The single excluded AC has a total population of 300 000 inhabitants.
Reperfusion StrategiesWe used ICD-9-CM and Healthcare Cost and Utilization Project Clinical Classification Software codes to identify whether the patients received thrombolysis (V45.88, 99.10) or PCI (PCI; 00.66, 36.01, 36.02, 36.05, 36.06, and 36.07). Those patients with none of these codes were considered to have received medical therapy alone (no reperfusion). For patients with ≥ 1 procedure code, we considered the least invasive therapy as the intended treatment. For example, patients who underwent thrombolysis and PCI were assigned to the thrombolysis group. The rate of each treatment by ACHS was defined as the proportion between the number of episodes with each type of treatment and the total number of STEMI episodes in the selected population of each region.
The year of the development of organized systems of care for STEMI patients in the different AC9 was double checked using data from the National Cardiac Catheterization and Interventional Cardiology Annual Registry10 and information provided by members of the Interventional Cardiology Working Group of the Spanish Society of Cardiology in each of the 16 AC. In 2003, only 3 of the 16 ACHS had developed organized network systems of care for STEMI, covering 5% of the population of the aggregate of ACHS. In 2012, 10 of 16 ACHS had complete or partial network systems for STEMI patients, covering 61% of the population. The implementation of the organized networks was progressive in most regions.
In-hospital Mortality Risk AdjustmentThe primary outcome measure was all-cause in-hospital mortality, defined as death during the hospitalization documented in the database. The mortality measures use administrative data from the minimum basic data set, and are calculated using multilevel logistic regression models to account for the clustering of observations within hospitals and differences in the number of admissions across hospitals.6,11 For risk adjustment, patient comorbidities were identified from these data for each index hospitalization. This modeling strategy accounts for within-hospital correlation of the observed deaths and reflects the assumption that, after adjustment for patient risk and sampling variability, the remaining variation is due to hospital quality of care. We calculated the risk-standardized in-hospital mortality rate as the ratio of the predicted mortality (which considers, on an individual basis, the ACHS in which the patient is being treated) to the expected mortality (which considers a standard functionality according to the average of all ACHS), multiplied by the crude mortality rate. Thus, if the risk-standardized mortality rate of an ACHS is higher than the crude mortality rate, the probability of a patient dying in that ACHS is higher than the average of the ACHS considered.
Statistical AnalysisCategorical variables are expressed as number (%). Quantitative variables are expressed as mean ± standard deviation. Comparisons of categorical variables were performed with the chi-square test and comparisons of quantitative variables were performed with the ANOVA test, corrected with the Bonferroni test for the level of significance. Poisson and negative binomial regression models were adjusted to assess the impact of interventions on the incidence ratio of outcome measures (PCI procedures and RSMR).
Both the incidence rate ratio and 95% confidence intervals (95%CI) are presented. Interventions were defined as a binary variable and were assigned a value as 1 as each network was set up for each AC and were otherwise assigned a value of 0. Linear regression models were used for correlations to assess the slope, 95%CI, and correlation coefficient of the percentage of primary PCI procedures in relation to the RSMR by ACHS, in 2012. Statistical significance was defined as a P value < .05. Analyses were performed with STATA 13.0.
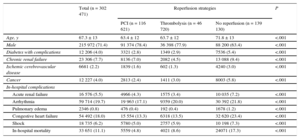
RESULTSWe identified 302 471 patients with STEMI from 2003 to 2012 in the Spanish taxpayer-funded health service database. During this period, 116 621 patients (38.6%) underwent PCI during admission, 46 720 patients underwent thrombolysis (15.4%), and 139 130 received no reperfusion (46%). The baseline characteristics, comorbidities and in-hospital mortality in each group are described in Table 1. The mean age for the overall cohort was 67.3 years. Patients who did not receive PCI or thrombolysis were older, with a higher proportion of women and had a greater number of comorbidities and complications during the hospitalization. For the whole period analyzed, the crude mortality rate was 4.8% in the PCI cohort, 8.6% in the thrombolysis group, and 17.3% in the no-PCI or thrombolysis group (P < .001).
Risk Factors and In-hospital Complications in the Different Groups
| Total (n = 302 471) | Reperfusion strategies | P | |||
|---|---|---|---|---|---|
| PCI (n = 116 621) | Thrombolysis (n = 46 720) | No reperfusion (n = 139 130) | |||
| Age, y | 67.3 ± 13 | 63.4 ± 12 | 63.7 ± 12 | 71.8 ± 13 | <.001 |
| Male | 215 972 (71.4) | 91 374 (78.4) | 36 398 (77.9) | 88 200 (63.4) | <.001 |
| Diabetes with complications | 12 206 (4.0) | 3321 (2.8) | 1349 (2.9) | 7536 (5.4) | <.001 |
| Chronic renal failure | 23 306 (7.7) | 8136 (7.0) | 2082 (4.5) | 13 088 (9.4) | <.001 |
| Ischemic cerebrovascular disease | 6681 (2.2) | 1839 (1.6) | 602 (1.3) | 4240 (3.0) | <.001 |
| Cancer | 12 227 (4.0) | 2813 (2.4) | 1411 (3.0) | 8003 (5.8) | <.001 |
| In-hospital complications | |||||
| Acute renal failure | 16 576 (5.5) | 4966 (4.3) | 1575 (3.4) | 10 035 (7.2) | <.001 |
| Arrhythmia | 59 714 (19.7) | 19 963 (17.1) | 9359 (20.0) | 30 392 (21.8) | <.001 |
| Pulmonary edema | 2346 (0.8) | 476 (0.4) | 192 (0.4) | 1678 (1.2) | <.001 |
| Congestive heart failure | 54 492 (18.0) | 15 554 (13.3) | 6318 (13.5) | 32 620 (23.4) | <.001 |
| Shock | 18 735 (6.2) | 5780 (5.0) | 2757 (5.9) | 10 198 (7.3) | <.001 |
| In-hospital mortality | 33 651 (11.1) | 5559 (4.8) | 4021 (8.6) | 24071 (17.3) | <.001 |
PCI, percutaneous coronary intervention.
Unless otherwise indicated, data are expressed as No. (%) or mean ± standard deviation.
There were important changes in clinical management throughout the study period (Figure 1). The percentage of patients who were treated with PCI progressively increased with a concomitant moderate reduction in the fibrinolysis rate. The percentage of patients not receiving PCI or thrombolysis substantially decreased during the study period. The distribution of the selected episodes between AC closely followed the distribution of the Spanish population. For all groups, there was a steady decrease in crude (13.1% in 2003; 9.2% in 2012; P < .001) and risk-adjusted in-hospital mortality (10.7% in 2003; 6.8% in 2012; P < .001) rates from 2003 to 2012.
Changes in reperfusion strategies in the treatment of STEMI in the Spanish taxpayer-funded health system between 2003 and 2012. There were important changes in the reperfusion strategies applied throughout the study period. The percentage of patients treated with PCI progressively increased with concomitant moderate reductions in the thrombolysis rate. PCI, percutaneous coronary intervention.
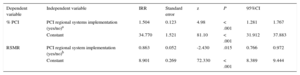
There was a correlation between PCI rates and risk-standardized mortality rates throughout the study period (Figure 2). In-hospital risk-adjusted mortality decreased from 10.70 to 6.78 when the percentage of patients with PCI increased from 21.6% to 55%, respectively. In addition, there was a significant association between the development of regional network programs for STEMI treatment, an increase in PCI procedures, and in-hospital mortality reduction. The implementation of these strategies was associated with a 50% increase in the number of PCI procedures (P < .001) with a 14% reduction in RSMR (P = .015) (Table 2).
Association between PCI rates and mortality in the treatment of STEMI patients in the Spanish taxpayer-funded health service between 2003 and 2012. There was a significant correlation between PCI rates and risk-standardized mortality rates during the study period. PCI, percutaneous coronary intervention; PCI-p, primary percutaneous coronary intervention; RSMR, risk-standardized mortality rates.
Association Between the Implementation of STEMI Regional Network Systems, PCI Treatment, and RSMR
| Dependent variable | Independent variable | IRR | Standard error | z | P | 95%CI | |
|---|---|---|---|---|---|---|---|
| % PCI | PCI regional systems implementation (yes/no)a | 1.504 | 0.123 | 4.98 | < .001 | 1.281 | 1.767 |
| Constant | 34.770 | 1.521 | 81.10 | < .001 | 31.912 | 37.883 | |
| RSMR | PCI regional system implementation (yes/no)b | 0.863 | 0.052 | -2.430 | .015 | 0.766 | 0.972 |
| Constant | 8.901 | 0.269 | 72.330 | < .001 | 8.389 | 9.444 |
95%CI, 95% confidence interval; IRR, incidence rate ratio; PCI, percutaneous coronary intervention; RSMR, risk-standardized mortality rates; STEMI, ST-segment elevation myocardial infarction.
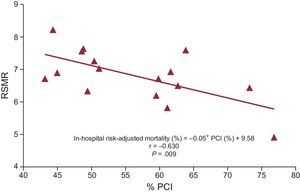
The implementation of regional network programs for the treatment of STEMI was highly unequal among the different regions in Spain. Figure 3 shows the starting year of the network programs in the different AC. In programs initiated between 2005 and 2010 (Balearic Islands, Catalonia and the Principality of Asturias), where the impact of the program can be assessed in comparison with previous years, there was a consistent and significant increase in the percentage of patients treated with PCI accompanied by a decrease in mortality (Figure 3). In the evaluation of the individualized data for each AC in 2012, a strong relationship was found between the percentage of PCI procedures and the risk reduction in standardized in-hospital mortality (Figure 4).
Changes in reperfusion strategies in the distinct autonomous communities in Spain from 2003 to 2012 and impact on mortality. The starting year of the network program for the treatment of STEMI is identified as a vertical arrow for each of the communities. In programs initiated between 2005 and 2010 (Balearic Islands, Catalonia and the Principality of Asturias), where the impact of the program could be assessed in comparison with previous years, a significant increase in the percentage of patients treated with PCI with a decrease in mortality was consistently observed. PCI, percutaneous coronary intervention; RSMR, risk-standardized mortality rates; STEMI, ST-segment elevation myocardial infarction.
= Year of implementation of the STEMI network program.Association between the PCI rate in the treatment of STEMI patients and in-hospital mortality in each autonomous community in Spain in 2012. In the evaluation of individualized data for each autonomous community in 2012, a relationship was found between the percentage of PCI procedures and the risk-standardized hospital mortality rate. PCI, percutaneous coronary intervention; RSMR, risk-standardized mortality rates.
The main findings of our study are the following: a) both the PCI rate and the percentage of STEMI patients receiving PCI or thrombolysis in Spain increased substantially throughout the study period, b) different health policies across the AC in Spain led to unequal access to PCI in this clinical setting, and c) there was a clear and consistent association between the development of regional network systems of care for STEMI and the PCI rate and mortality.
Current guidelines recommend the implementation of STEMI reperfusion networks to offer the best and most timely reperfusion strategy to a higher percentage of patients, which has led to the widespread use of mechanical reperfusion in many areas of the world during the last few years. The data from our study also show a marked increase in the PCI rate across all AC in Spain. The number of STEMI networks substantially increased in Spain during the last few years, when the country joined the “stent for life” initiative. From 2009, 6 networks were created in 6 different communities, increasing the population coverage and the number of procedures across the country. These data have also been observed in other countries across Europe. Kristensen et al.2 described a significant increase in the rate of primary PCI in most countries across Europe, which was especially marked for those countries involved in the Stent for Life project.
Of interest, this increase in the rate PCI procedures was observed in some AC before the implementation of their STEMI networks. Therefore, in our opinion, the increase in the rate of PCI observed in Spain during the study period might not only be due to the implementation of STEMI reperfusion networks across distinct AC. Other factors, such as the previous implementation of small local networks by some hospitals, might also have played a role in these findings.
Implementation of reperfusion networks in STEMI is highly influenced by a large number of regional conditions (eg, distance from the tertiary center, transfer times, quality of emergency medical services, the availability of catheterization laboratories, political and economic conditions). Thus, guidelines emphasize the need for these networks to be customized and refined by regional health system leaders. In fact, there are substantial differences in the management of STEMI between different countries of the world, related to huge socioeconomic, demographic, epidemiological, and health care organization variables.12–15 Puymirat et al.16 found significant differences between European Regions, with in-hospital mortality ranging from 4.1% (northern countries) to 10.1% (eastern countries). Describing reperfusion therapy in 37 European countries, Kristensen et al.2 reported that there are still large national variations in treatment strategies for patients admitted with STEMI. Despite the recommendations of international guidelines, a substantial number of patients are still not offered any reperfusion therapy, especially in some southern and eastern European countries. Variation in PCI uptake cannot be explained solely by economic incentives, illness severity, or patient preferences and the barriers to PCI implementation are a complex mix of medical, organizational, patient-related, regulatory, and economic factors.2 Substantial differences have been described even between highly developed STEMI treatment systems.17
In line with these findings, our data also show major differences in the PCI rate across different regions in Spain. The Spanish taxpayer-funded health system has important particularities. There are 17 AC with the power to develop their own health policies, each with its own political and economic interests. In fact, several studies performed in Spain have shown marked differences between regions and hospitals in the management of patients with myocardial infarction.6,18–21 In addition to the implementation of regional STEMI systems, other factors are probably involved in the disparities found between the distinct AC, such as differences in cardiovascular risk factors22 and socioeconomic development.23
While multiple issues regarding the effectiveness of several technological advances in the prognosis of patients with acute coronary syndromes have been resolved in the last few decades, the impact of health planning and health care management on patient outcomes has received less attention. In the RECALCAR project, designed to assess the relationship between organizational aspects and management in STEMI patients, a strong association was observed between the technological equipment of hospitals, the role of cardiology departments at discharge, the performance of PCI procedures and in-hospital mortality rates.6 Importantly, differences in PCI treatment and the development of regional STEMI treatment systems showed a clearly significant association with in-hospital mortality in our series. Equally, other factors developed during the study period (newer antithrombotic drugs, intensive statin use, aldosterone antagonists, reduction in times to admission) might also have contributed to reducing in-hospital mortality in patients in this study.
LimitationsOur study has several limitations. This is an observational study and therefore we cannot exclude a certain selection bias and the potential effect of unmeasured confounding. This is also a retrospective study based on administrative data and also has the limitations inherent to risk adjustment of mortality. However, the use of administrative registries to assess results for health care services has been successfully validated by comparing the results obtained with data from hospital records and has also been successfully applied to research on health services outcomes.11,24–26 The performance of PCI in these patients referred to the whole period of hospitalization, and not only to the first hours after admission. However, several registries have shown that almost 80% of PCI procedures in STEMI patients correspond to primary PCI performed during the early reperfusion phase. On the other hand, the performance of angiography but not PCI in some patients due to their coronary anatomy was not a controlled variable in the analysis, although the number of these patients was small. In addition, the association between PCI and mortality observed in our series might be, at least partially, due to significant differences in major comorbidities between patients undergoing PCI or to other factors not assessed in our study.
CONCLUSIONSOur data clearly show a substantial increase in the rate of PCI in STEMI patients in Spain across the study period. The implementation of regional PCI network systems, with major differences between AC, led to notorious differences in in-hospital mortality in this population. In our opinion, this highlights the impact of health care policies on outcomes in real-world patients, thus encouraging the establishment of political measures at national and AC levels based on the regionalization of heart care services27 and the development of regional network systems covering the highest possible percentage of patients.
FUNDINGThe work for this article was funded by unconditional grants from Fundación Interhospitalaria para Investigación Cardiovascular and Laboratorios Menarini (RECALCAR Project). J.V. Segura is partially supported by the Ministerio de Economía y Competividad of Spain, Grant No. MTM2014-56233-P.
CONFLICTS OF INTERESTNone declared.
- -
Current guidelines recommend the need for optimal organization of STEMI systems of care at the community, regional and national level.
- -
However, the implementation of these reperfusion networks is strongly influenced by several regional factors such as transport times, the availability of resources and infrastructure, and the characteristics of health care systems.
- -
There is scarce information on the impact of health care policies on clinical outcomes in patients with heart diseases.
- -
The rate of PCI in STEMI patients substantially increased in Spain throughout the study period.
- -
The implementation of regional network systems of care for STEMI, with major differences between AC, led to notorious differences in in-hospital mortality in this population.
- -
These data highlight the impact of health care policies on outcomes in real-world patients, thus encouraging the establishment of political measures at different geographic levels based on the regionalization of heart care services.
The authors thank the Spanish Ministry of Health, Social Services, and Equality for the help provided to the Spanish Society of Cardiology to develop the RECALCAR study, with special gratitude to the General Directorate of Public Health, Quality, and Innovation.