During cardiogenesis,1 the sinus venosus is closed by the left and right venous valves. The left venous valve becomes incorporated into the septum secundum. The more prominent right venous valve directs oxygenated blood from the left side through the foramen ovale. It subsequently involutes during development to form the eustachian and thebesian valves. Disruption of this process is believed to be responsible for a wide variety of abnormalities2: prominent eustachian valve, Chiari network (2%-15%)1 and, in the most extreme case, cor triatriatum dexter (CTD), in which the right atrium is completely divided into 2 compartments by a membrane that restricts flow toward the right ventricle.
CTD can be associated with right ventricular hypoplasia, pulmonary atresia, and Ebstein abnormality.3,4 The redundant eustachian valve combined with septal defect can lead to paradoxical embolism or platypnea-orthodeoxia syndrome.1
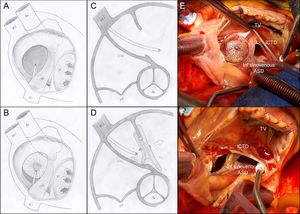
One variant is incomplete CTD (iCTD), in which the valve remnant, without completely dividing the right atrium, is prolonged with the anterior border of the atrial septum,3 thus generating septal misalignment with atrial septal defect (ASD) (Figure 1).
Schematic representation of iCTD and ASD without retroaortic border and with misalignment. Viewed from the right atrium without the device (A) and during deployment of the left disc (B). Transesophageal echocardiography, short-axis basal view at 45° without (C) and with (D) the device. The membrane does not allow ready adaptation of the right disc, and so the risk of embolization is increased. E and F, surgery; ASD in the inferior venous sinus, iCDT and device closing the fossa ovale (E) and after withdrawing the device (F). Ao, aorta; ASD, atrial septal defect; iCDT, incomplete cor triatriatum dexter; IVC, inferior vena cava; SVC, superior vena cava; TV, tricuspid valve.
We describe 7 patients in whom this finding was associated with complications or the impossibility of percutaneous ASD closure: 6pediatric patients (2-13 years) and 1 adult patient aged 63years, all diagnosed with moderate-large ASD, with hemodynamic repercussions and anatomic features considered amenable to percutaneous closure.
In 6 patients, transesophageal echocardiography (TEE) pointed to a common anatomy consisting of a membrane that extended from the anterior border of the inferior vena cava to the atrioventricular border of the ASD, and, in some cases, as far as the retroaortic margin, which pulled this structure, leading to misalignment with the rest of the septum secundum.
In 4 patients, percutaneous closure was attempted; in 2, initial closure was achieved, with a 10.5-mm device in 1 patient and a 15mm device in the other. In both patients, the device was embolized early to the ascending aorta, then recaptured with a loop, and, finally, a new oversized device (14 and 22mm) was placed to achieve stable and successful closure. In the other 2 patients, closure was not achieved because it was not possible to trap the anterior border of the defect, not even with oversized devices.
In view of prior experience and after confirmation of a less favorable anatomy by TEE, 2 patients were not considered suitable for percutaneous closure.
One of these was a 63-year old woman who was referred from another center for persistent right ventricular dilatation and pulmonary hypertension after percutaneous closure of an ostium secundum atrial septal defect. With TEE and surgery, the device closed an extensive fossa ovale, but a large residual defect of the inferior venous sinus along with iCTD and misalignment remained (Figure 1).
iCTD is present in up to 5%3 of cases of ASD referred for percutaneous closure. Diagnosis is usually inadvertent through transthoracic echocardiography; it should be suspected in cases of defect with septal misalignment.
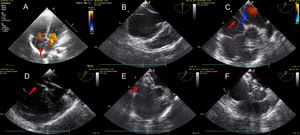
The TEE view that best identified the structure was the short-axis basal view (middle esophagus at 30-60°). Given its oblique arrangement, this view can enable complete visualization of misalignment with the rest of the septum secundum. The 4 chamber view (middle esophagus and 0°) can be misleading, unless a vertical sweep is performed that identifies the entire trajectory. The bicaval view (middle esophagus at 90-110°) was not useful (Figure 2). The usefulness of intracardiac echocardiography for diagnosis has been reported,4 although this technique is not used in pediatric patients given the caliber of the introducer.
Echocardiographic images of iCTD (red arrows). A: transthoracic echocardiography, 4 chamber apical view. B: transesophageal echocardiography, bicaval view at 86°. C: short-axis basal view at 47° with Color Doppler, the best view for visualizing iCTD and ASD. D: similar view with catheter arriving in the left atrium through the defect and iCTD. E: iCTD prevents appropriate expansion of the right disk of the device. F: placement of the oversized device, trapping the iCTD membrane with successful ASD closure. ASD: atrial septal defect; iCTD: incomplete cor triatriatum dexter.
Unlike in other series,4 in our experience this abnormality is associated with complications during percutaneous closure of the ASD: the device was embolized in 2patients and contraindicated in a further 2. The anterior border of the defect, formed by the insertion of this membrane, lies outside the right atrial disc of the device, making capture hard despite traction maneuvers, and left a residual atrioventricular shunt. Device oversizing enables it to be attached to the anterior border by folding the membrane between the discs. This approach, however, was not useful in 2 patients, probably because of the greater rigidity.
In conclusion, the importance of ruling out this abnormality during anatomical study of ASD is highlighted. The presence of such a defect increases the difficulty and risk of complications during the procedure. Sometimes, the use of an oversized device can overcome some of the difficulties associated with the procedure, but when the continuity of the membrane is very extensive (from the retroaortic margin to the atrioventricular border), more rigid (echocardiographically thick), or the defect is very large, surgical correction is considered the best option.
Conflicts Of InterestA. Á. Sánchez-Recalde is Associate Editor of Revista Española de Cardiología.