We report two cases of infected ascending aorta prostheses, evaluate the treatment received, and review the related literature.
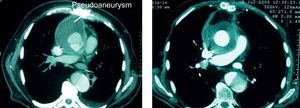
The first case is a 77-year-old man, smoker, with a history of hypertension and gastric ulcer. Seven months after surgery for a type A aortic dissection, with replacement of the supracoronary ascending aorta by a Dacron prosthesis, the patient presented purulent drainage through the sternotomy. Computed tomography study showed an aortic pseudoaneurysm that had fistulized to the skin through the sternum (Fig. 1). The patient was reoperated through a median sternotomy with extracorporeal circulation via the femoral vessels. Following vent placement through a left minithoracotomy, deep hypothermia and circulatory arrest were established, the purulent material was cleaned, and an anastomotic dehiscence was repaired, while retaining the original Dacron prosthesis. The prosthesis and retrosternal space were then covered with abdominal omentum (omentoplasty). Blood cultures were negative, and culture of the fistula drainage and periprosthetic and pseudoaneurysm material yielded Staphylococcus epidermidis. The patient initially received 6 weeks of intravenous treatment with vancomycin, rifampicin, and gentamicin, then oral linezolid and rifampicin for 4 weeks. Owing to hematologic toxicity, linezolid was discontinued and treatment was changed to trimethoprim-sulfamethoxazole, and rifampicin for 26 weeks. Antibiotic therapy was then stopped, and there was no clinical, analytic, microbiologic, or radiologic (computed tomography and technetium-labeled autologous leukocytes) (Fig. 1) evidence of infectious activity. After 36 months of follow-up, there was no evidence of relapse.
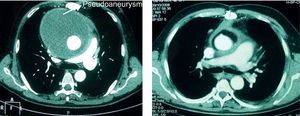
The second case is a 57-year-old man with no previous illnesses, and prolonged fever. Nineteen months before consulting, the patient had underdone surgery to treat an aneurysm of the ascending aorta and aortic insufficiency, involving implantation of a CarboSeal 27 valved Dacron tube graft, with reimplantation of the coronary ostia. Chest computed tomography disclosed a large pseudoaneurysm of the ascending aorta (Fig. 2). Prosthesis replacement was not considered a viable option because of the technical complexity of the procedure and the high surgical risk. The patient was reoperated through a median sternotomy, with extracorporeal circulation via the femoral vessels. Deep hypothermic circulatory arrest was established. Multiple thrombi were removed from the pseudoaneurysm and an anastomotic dehiscence was repaired, while retaining the previously implanted valved tube graft. Omentoplasty was carried out to cover the original prosthesis. Blood cultures were negative, and S. epidermidis was isolated on culture of the periprosthetic and aneurysm material. The patient was treated with intravenous vancomycin and gentamicin during 6 weeks, and with linezolid for an additional 18 weeks. At that time, linezolid was discontinued due to hemotoxicity, and according to the antibiogram, no alternative oral antibiotic option was available. Nonetheless, the patient showed no clinical, analytic, microbiologic, or radiologic signs of infectious activity (Fig. 2), and treatment was stopped. After 36 months of follow-up, there was no evidence of a relapse.
Two cases of infected ascending aorta prostheses are presented. In both patients, echocardiographic study soon after prosthesis implantation showed an absence of pseudoaneurysms, thus indicating that the mechanism for pseudoaneurysm formation was an infectious process. The patients’ clinical course was favorable following local surgical debridement and repair, retention of the original prosthesis and covering with omentum, and prolonged antibiotic therapy.
Infection of the ascending aorta prosthesis is an uncommon (0.9%-2%) but serious condition, with an associated mortality rate higher than 40%.1 The recommended treatment is replacement of the infected prosthesis together with antibiotic therapy, but sometimes, graft replacement is not feasible. There are reported cases in which the infected prosthesis has been retained with therapeutic success; the most widely accepted technique for this purpose is local surgical debridement and repair, supported by omentoplasty.2,3 This option, which should be considered a last resort, is useful when prosthesis replacement is technically impossible or when infection occurs in patients of advanced age or those with severe comorbidities.4 In these cases, retaining the graft originates a high risk of recurrent infection. Therefore, the area should be cleaned and infected necrotic tissue debrided, the anterior mediastinum should be irrigated with antiseptic solutions, and omentum or muscle flap transposition should be carried out to create a barrier and close dead space to control the infection.2 The use of omentoplasty provides the vascularity, easy transposition, and considerable filling potential of the omentum.
There is no consensus as to the optimal antibiotic treatment for infected ascending aorta prostheses or duration of this therapy. In empirical regimens, coverage against methicillin-resistant Staphylococcus aureus and coagulase-negative staphylococci is mandatory, since Staphylococcus spp. are the most common microorganisms isolated.5 Some authors recommend intravenous antibiotic therapy followed by suppressive oral antibiotics for life.4 Our patients received antibiotic therapy of limited duration and have shown no signs of recurrent infection after 3 years of follow-up; hence, we consider that the therapy was adequate. Although the optimum treatment duration remains uncertain, it would be reasonable to administer 4 to 6 weeks of intravenous therapy followed by oral suppressive therapy during at least 24 weeks. Treatment withdrawal can then be evaluated, providing there are no signs of recurrent infection.
There is no definitive evidence regarding treatment for infected ascending aorta prostheses. In the two patients presented, maintaining the prosthesis using the strategy described, followed by adequate prolonged antibiotic therapy and close follow-up, proved to be an effective approach.
.