We are witnessing an increase in the understanding of cardiac amyloidosis due to abnormal deposits of the protein transthyretin (ATTR), both its hereditary form and acquired (or senile) form. Current data from Spain indicate that ATTR is the most common type of cardiac amyloidosis. Heart failure (HF) is the most frequent presentation and close to 35% of patients will have deterioration in left ventricular ejection fraction (LVEF) and short survival.1 Furthermore, a substantial number of patients with ATTR have conduction system abnormalities (7% have advanced atrioventricular block) or left ventricular systolic dysfunction.2 Previous studies have shown a deleterious effect from frequent ventricular pacing and a clinical benefit from cardiac resynchronization therapy (CRT) in selected patients with ATTR.3 Recently, physiological pacing of the left bundle branch (LBBP) has become a safe, feasible alternative for those who require antibradycardia treatment or CRT.4 Our objective was to study the technical viability of LBBP in ATTR and analyze its clinical effects in a pilot experience. The study was approved by the Granada province Research Ethics Committee. Patients gave written consent for study participation and publication.
We present 3 patients with ATTR, HF, and left ventricular systolic dysfunction requiring permanent ventricular pacing; because they remained symptomatic, LBBP was performed with the aim of optimizing CRT and preventing LVEF deterioration as a consequence of the permanent pacing (table 1).
Baseline characteristics and outcomes at 3 months after the start of LBBP treatment
| Patient 1 | Patient 2 | Patient 3 | ||||
|---|---|---|---|---|---|---|
| Sex | Male | Male | Male | |||
| Age, y | 83 | 72 | 84 | |||
| Type of ATTR | Acquired | Hereditary (p.Val142Ile) | Acquired | |||
| Carpal tunnel syndrome | + | + | - | |||
| Polyneuropathy | + | + | - | |||
| Hypertension | + | + | - | |||
| Pulmonary hypertension | - | + | - | |||
| Glomerular filtration rate < 45 mL/min/1.73 m2 | + | + | + | |||
| CVE | - | - | - | |||
| AF | Permanent | Paroxysmal | Paroxysmal | |||
| Indication | SND | cAVB | SND | |||
| Treatment | ||||||
| RAASI | No | Enalapril | Candesartan | |||
| Beta-blockers | No | No | Bisoprolol | |||
| MRA | Spironolactone | No | Spironolactone | |||
| Tafamidis | No | Yes | No | |||
| Diuretics | Furosemide 120 mg | Furosemide 120 mg | Furosemide 80 mg | |||
| SGLT2i | No | No | No | |||
| Rhythm | Permanent AF | Permanent AF | Paroxysmal AF | |||
| Previous device | CRT-P (basal inferolateral coronary sinus) | No | CRT-P (mid inferolateral coronary sinus) | |||
| Baseline | 3 mo | Baseline | 3 mo | Baseline | 3 mo | |
| NYHA | III | II | IV | III | III | II |
| LVEF, % | 37 | 37 | 43 | 57 | 30 | 49 |
| QRS, ms | 156 | 128 | 186 | 138 | 248 | 148 |
| BNP, pg/mL | 1513 | 1411 | 1469 | 1150 | 959 | 564 |
| Emergency department visits due to cardiac cause (6 mo) | 2 | 1 | 2 | 0 | 1 | 0 |
| Hospitalization for HF (1 y) | 1 | 0 | 1 | 0 | 0 | 0 |
| [0,1-7]Electric parameters relating to left bundle branch pacing | ||||||
| QRSd, ms | 128 | 138 | 148 | |||
| LVAT, ms | 88 | 92 | 96 | |||
| Left bundle capture threshold, V × 0.4 ms | 0.75 | 0.75 | 1 | |||
| Mode | VVIR | DDD | DDDR | |||
| Percentage ventricular pacing | 97 | 99.6 | 99.9 |
AF, atrial fibrillation; ATTR, transthyretin amyloidosis; BNP, brain natriuretic peptide; cAVB, complete atrioventricular block; CRT-P, cardiac resynchronization therapy; CVE, cerebrovascular event; HF, heart failure; LVAT, left ventricular activation time; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonists; NYHA, New York Heart Association functional class; RAASI, renin-angiotensin-aldosterone system inhibitors; SGLT2i, sodium-glucose cotransporter type 2 inhibitor; SND, sinus node dysfunction.
The first patient was an 83-year-old man with acquired ATTR who had a syncopal episode caused by sinus node dysfunction (SND) and nodal escape, with slight wall hypertrophy and mildly reduced LVEF. The patient had a dual chamber pacemaker, and 2 years later, in light of the etiological diagnosis, development of atrioventricular disease, and LVEF deterioration requiring permanent pacing, he was changed to conventional CRT. His progress was unfavorable, and he developed atrial fibrillation, had a deterioration in functional class and was hospitalized for HF, triggering the decision to use LBBP.
The second patient was a 72-year-old man with hereditary ATTR (p.Val142Ile variant) and paroxysmal atrial fibrillation with a severe deterioration in HF functional class since the diagnosis of the disease (1 admission and 2 visits to the emergency department for HF). He subsequently developed atrioventricular block, and was treated with LBBP with the aim of avoiding LVEF deterioration.
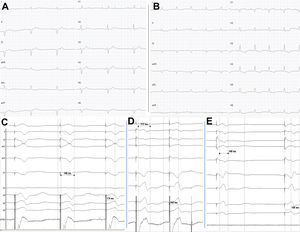
The third patient was an 84-year-old man who was under follow-up for ventricular hypertrophy of unknown etiology since diagnosis 4 years prior. During the follow-up, he developed difficult-to-control persistent atrial fibrillation, left bundle branch block, and progressive left ventricular systolic dysfunction. After the onset of the syncopal sinus node dysfunction, a CRT device was implanted (QRSd, 160ms). Eventually, 1 year later, once considered a nonresponder and with deterioration in functional class, it was decided to use LBBP, and a QRSd of 140ms was obtained (figure 1).
A: baseline electrocardiogram with first-degree AVB and right bundle branch block and left axis deviation. B: LBBP; typical rsr’ morphology with normal axis. C: typical “W” morphology in V1 before lead penetration of IVS. D: initial penetration of the IVS with shortening of the paced QRS interval (212ms) and of the LVAT interval (162ms). E: capture of the left bundle with rsr’ morphology in V1, narrower QRS interval (148ms) and shorter LVAT (108ms). AVB, atrioventricular block; IVS, interventricular septum; LBBP, left bundle branch pacing; LVAT, left ventricular activation time. gr1.
In the 3 patients, a guide catheter was used for septal pacing (C315 HIS, Medtronic Inc, USA). Over that, a lead was introduced (Select-Secure model 3830 69cm, Medtronic Inc., USA), connected to the polygraph to record intracavity signal. The guide catheter was positioned 2 cm apically to the His bundle electrogram and, using 6 to 8 clockwise turns, the lead penetrated the interventricular septum until capture of the left bundle branch was achieved. In the 3 patients, the following 4 criteria were used for LBBP (figure 1):5
- •
Shortening of the spike-R wave interval in V6
- •
rsr’/rsR’ morphology in V1
- •
Narrowing of the QRS complex after septal penetration
- •
Change in selective-nonselective capture
In our experience, the success rate of the implant was 100%, with no incidents of note. In all cases, a paced QRS that was narrower than before was achieved.
Although the 3 patients were of advanced age, had atrial fibrillation (paroxysmal in 2 and permanent in 1), chronic kidney disease (stage G3a), and advanced HF (New York Heart Association [NYHA] functional class III-IV/IV), at 3 months after starting LBBP, all had improved functional class, with a slight reduction in natriuretic peptide levels (table 1). Regarding LVEF, 2 patients had an increase, but the first did not. Lastly, although statistical inferences are not possible due to the small sample size, there was a reduction in the number of hospitalizations after 1 year and emergency department visits for HF at 6 months after LBBP (table 1).
In conclusion, this study is limited by its small sample size, its retrospective design, the variability in echocardiographic measurements, and the short follow-up. However, in our initial small cohort of patients with ATTR, LBBP proved to be a viable and effective therapeutic option in the short-term (3 months) for the optimization of CRT and which allowed improvement in HF symptoms. This hypothesis should be confirmed in larger, prospective studies.
FUNDINGThis study did not receive any specific funding from public sector, commercial, or not-for-profit funding bodies.
AUTHORS’ CONTRIBUTIONSF.J. Bermúdez-Jiménez collected and analyzed the data; he wrote the manuscript with the help of the other authors. M. Molina-Lerma and P. Sánchez-Millán performed and supervised the technical procedures. J. Jiménez-Jáimez and R. Macías-Ruiz conceived the idea presented. M. Álvarez supervised the overall process. All authors discussed the results and contributed to the final manuscript.
CONFLICTS OF INTERESTThe authors have nothing to declare.