Coronary chronic total occlusions (CTO) involving bifurcation lesions are a challenging lesion subset that is understudied in the literature. This study analyzed the incidence, procedural strategy, in-hospital outcomes and complications of percutaneous coronary interventions (PCI) for bifurcation-CTO (BIF-CTO).
MethodsWe assessed data from 607 consecutive CTO patients treated at the Institut Cardiovasculaire Paris Sud (ICPS), Massy, France between January 2015 and February 2020. Procedural strategy, in-hospital outcomes and complication rates were compared between 2 patient subgroups: BIF-CTO (n=245=and non–BIF-CTO (n=362).
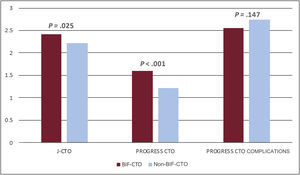
ResultsThe mean patient age was 63.2±10.6 years; 79.6% were men. Bifurcation lesions were involved in 40.4% of the procedures. Overall lesion complexity was high (mean J-CTO score 2.30±1.16, mean PROGRESS-CTO score 1.37±0.94). The preferred bifurcation treatment strategy was a provisional approach (93.5%). BIF-CTO patients presented with higher lesion complexity, as assessed by J-CTO score (2.42±1.02 vs 2.21±1.23 in the non–BIF-CTO patients, P=.025) and PROGRESS-CTO score (1.60±0.95 vs 1.22±0.90 in the non–BIF-CTO patients, P<.001). Procedural success was 78.9% and was not affected by the presence of bifurcation lesions (80.4% in the BIF-CTO group, 77.8% in the non–BIF-CTO-CTO group, P=.447) or the bifurcation site (proximal BIF-CTO 76.9%, mid–BIF-CTO 83.8%, distal BIF-CTO 85%, P=.204). Complication rates were similar in BIF-CTO and non–BIF-CTO.
ConclusionsThe incidence of bifurcation lesions is high in contemporary CTO PCI. Patients with BIF-CTO present with higher lesion complexity, with no impact on procedural success or complication rates when the predominant strategy is provisional stenting.
Keywords
Abbreviations
Coronary chronic total occlusions (CTO) are identified in 18% to 20% of patients with coronary artery disease in contemporary series and their incidence increases with age.1,2 The prevalence of CTO exceeds 40% in patient with diabetes and heart failure.3,4 Most patients are managed medically or are referred for coronary artery bypass grafting (CABG), with less than 10% being treated with percutaneous techniques.5
Coronary bifurcations are by nature prone to the development of atherosclerotic lesions and account for 15% to 20% of all percutaneous coronary interventions (PCI)6 and have lower success rates and higher complication rates than nonbifurcation lesions.7,8 In the context of a CTO, bifurcation lesions often pose an additional challenge, as side branch (SB) wiring and protection can be more difficult. Moreover, contemporary CTO PCI can involve dissection re-entry techniques that cause SB compromise. Conversely, the presence of a SB can be beneficial in selected cases. For example, a proximal SB might offer the possibility of intravascular ultrasound (IVUS)-guided puncture; equally, a SB within the CTO body can be considered as an island and aid access to the CTO by splitting it in 2 parts.
The aim of this study was to determine the incidence, procedural strategy, in-hospital outcomes and complications of CTO PCI involving bifurcation lesions and compare 2 patient cohorts (BIF-CTO and non–BIF-CTO) treated in a high-volume European center in France.
METHODSWe retrospectively assessed data from 607 consecutive patients undergoing CTO PCI between January 2015 and February 2020 at the Institut Cardiovasculaire Paris Sud (ICPS), Massy, France. Of these, 245 patients (40.4%) had a SB ≥ 2mm located within 5mm of the proximal or distal cap or within the occluded segment. Procedural strategy, in-hospital outcomes and complication rates were compared between the 2 patient cohorts (BIF-CTO and non–BIF-CTO). The treatment indication was symptomatic myocardial ischemia and/or evidence of reversible myocardial ischemia on perfusion imaging or stress testing, as proposed in the EuroCTO Club position paper.9 Patients were requested to provide informed consent before the procedure. The study was performed in accordance with the Declaration of Helsinki. Systematic troponin evaluation was performed on day 1 to evaluate myocardial injury.
DefinitionsA coronary CTO is defined as a total occlusion in a coronary artery with noncollateral thrombolysis in myocardial infarction (TIMI) flow grade 0 for at least 3 months.9 Patients were considered to have undergone retrograde CTO PCI if a guidewire was introduced into a collateral channel supplying the target vessel. A procedure was defined as an antegrade wire escalation if no guidewire was introduced into a collateral channel, as previously defined. A procedure was defined as antegrade dissection re-entry (ADR) if wire or device-based vessel dissection was adopted as part of the CTO recanalization strategy, either primarily or as bailout.
A bifurcation lesion is defined as a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant SB.10 Provisional stenting refers to the reconstruction of bifurcation anatomy with a single stent, implanted from the proximal to the distal segment of the main vessel (MV) across the ostium of the SB and followed by the systematic proximal optimization technique.10,11 Two-stent techniques use a second stent implantation in the SB, either upfront or as bailout.10 Specific techniques have been extensively studied in the literature and described in detail by dedicated groups of experts.10,11 Anatomical criteria and the risk of SB occlusion/reaccess are key determinants of the treatment strategy, which is based either on MV stenting first (T/TAP-T/T and Protrusion-technique, culotte stenting) or SB stenting first (mini crush, inverted T/TAP, inverted culotte, DK-crush).10,11
The baseline bifurcation anatomy was assessed using the Medina classification.12 The pattern of bifurcation disease was further classified into ‘true’ bifurcation lesions, in which the stenosis diameters in both the main branch and the SB were>50% and ‘false’ bifurcation lesions, in which only the MV or the SB showed significant narrowing. Bifurcation lesions were divided into 3 types according to the SB take-off from the MV; bifurcation lesions within the occluded segment and those located within 5mm of the proximal or distal CTO cap (figure 1). Lesions were further classified into 5 types to agree with relevant published literature.13 The strategy for CTO revascularization and bifurcation treatment was left to the operator's discretion.
CTO bifurcation lesions divided according to side branch (SB) take-off from the main vessel. A: bifurcation lesion located within 5mm proximal to CTO cap. B: bifurcation lesion arising within the CTO body. C: bifurcation lesion located within 5mm distal to CTO cap. The final post-PCI angiographic result can be seen at the inserts. CTO, chronic total occlusion; PCI, percutaneous coronary intervention; SB, side branch.
Technical success was defined as angiographic success (final residual stenosis<30% on visual estimation and TIMI flow grade 3 after CTO recanalization). Technical success was defined as residual stenosis of<30% in the MV and a final TIMI flow grade 3 in both branches. Procedural success was defined as angiographic success without the occurrence of in-hospital major adverse cardiac events (MACE).
In-hospital MACE were defined as a composite of non-Q wave and Q wave myocardial infarction (MI), recurrent angina requiring urgent repeat revascularization with PCI or CABG, stroke, death, pericardiocentecis, or surgical drainage of pericardial hematoma. Periprocedural MI definition was derived from the recent Academic Research Consortium-2 consensus document.14
Statistical analysisContinuous variables are expressed as the mean±standard deviation and were compared with 1-way analysis of variance. Categorical variables are expressed as percentages and were compared with the chi-square test. IBM SPSS Statistics version 22 software package (IBM Corporation, United States) and R language were used for all analyses. Two-sided P values<.05 were considered as indicative of statistical significance.
RESULTSDuring a period of approximately 5 years (January 2015 to February 2020), operators from the ICPS, Massy, France performed 607 consecutive CTO PCI procedures. Mean patient age was 63.2±10.6 years (79.6% male). Overall, patients with bifurcation lesions (BIF-CTO, 40.4%) and without bifurcation lesions (non–BIF-CTO, 59.6%) had similar baseline clinical characteristics, with a high prevalence of cardiovascular risk factors (table 1).
Baseline clinical characteristics
| Variable | BIF-CTO(n=245, 40.4%) | Non–BIF-CTO(n=362, 59.6%) | All CTO patients(N=607) | P |
|---|---|---|---|---|
| Age, y | 62.87±10.31 | 63.42±10.91 | 63.19±10.63 | .201 |
| Male sex | 78.4 | 80.4 | 79.6 | .545 |
| BSA, m2 | 2.02±0.23 | 1.99±0.21 | 2.00±0.22 | .269 |
| BMI, kg/m2 | 28.56±5.22 | 28.39±4.95 | 28.94±12.86 | .701 |
| Hypertension | 62.5 | 69.0 | 66.4 | .106 |
| Dyslipidemia | 73.7 | 73.6 | 73.7 | .982 |
| Smoking | 50.0 | 51.9 | 51.9 | .592 |
| Current smoker | 28.0 | 31.9 | 30.3 | |
| Previous smoker | 22.0 | 20.0 | 20.8 | |
| Diabetes mellitus | 31.0 | 34.5 | 33.1 | .630 |
| Medical treatment | 26.3 | 28.4 | 27.6 | |
| Insulin dependent | 4.7 | 6.1 | 5.5 | |
| Family history of CAD | 25.0 | 24.3 | 24.6 | .858 |
| Clinical presentation | .278 | |||
| Stable angina | 62.0 | 53.3 | 56.8 | |
| Acute coronary syndrome | 4.9 | 5.5 | 5.3 | |
| Asymptomatic | 27.8 | 35.6 | 32.5 | |
| Cardiac arrest | 0.8 | 0.6 | 0.7 | |
| Heart failure | 4.5 | 5.0 | 4.8 | |
| Angina | 60 | 52.8 | 56.7 | .174 |
| Class 1 | 1.6 | 0.8 | 1.2 | |
| Class 2 | 42.4 | 41.4 | 41.8 | |
| Class 3 | 15.5 | 9.9 | 12.2 | |
| Class 4 | 0.4 | 0.6 | 0.5 | |
| Killip class | .302 | |||
| Class 1 | 98.8 | 98.3 | 98.5 | |
| Class 2 | 0.0 | 1.1 | 0.7 | |
| Class 3 | 0.8 | 0.3 | 0.5 | |
| Class 4 | 0.4 | 0.3 | 0.3 | |
| Provocation test prior to PCI | 41.2 | 50.4 | 46.7 | .016 |
| Stress test | 0.0 | 3.1 | 1.8 | |
| Myocardial scintigraphy | 2.4 | 2.8 | 2.7 | |
| CMR | 38 | 44.3 | 41.7 | |
| ECHO stress | 0.8 | 0.3 | 0.5 | |
| Creatinine, μmol/L | 92.65±41.51 | 95.17±55.54 | 94.15±50.35 | .883 |
| Clearance, mL/min | 92.62±33.50 | 89.79±32.41 | 90.93±32.85 | .321 |
| Clearance>90 mL/min | 47.5 | 45.7 | 46.4 | .146 |
| Clearance 60-89 mL/min | 34.3 | 38.6 | 36.9 | |
| Clearance 45-59 mL/min | 14.0 | 8.2 | 10.5 | |
| Clearance 30-44 mL/min | 3.4 | 5.4 | 4.6 | |
| Clearance 15-29 mL/min | 0.0 | 0.6 | 0.3 | |
| Clearance<15 mL/min | 0.8 | 1.4 | 1.2 | |
| History of MI | 17.1 | 14.6 | 15.7 | .405 |
| History of CAD | 25 | 24.3 | 24.6 | .858 |
| History of CABG | 7.8 | 7.8 | 7.8 | 1 |
| History of stroke | 2.9 | 2.2 | 2.5 | .614 |
| History of peripheral artery disease | 3.7 | 6.6 | 5.4 | .115 |
| History of heart failure | 4.1 | 3.0 | 3.5 | .490 |
| NYHA class 1 | 18.0 | 16.6 | 17.1 | .316 |
| NYHA class 2 | 3.7 | 2.2 | 2.8 | |
| NYHA class 3 | 1.2 | 0.3 | 0.7 | |
| NYHA class 4 | 0.0 | 0.0 | 0.0 |
BIF-CTO, chronic total occlusion involving bifurcation lesion; BMI, body mass index; BSA, body surface area; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CTO, chronic total occlusion; ECHO, echocardiogram; PCI, percutaneous coronary intervention; CMR, cardiovascular magnetic resonance imaging; MI, myocardial infarction; NYHA; New York Heart Association classification of heart failure.
Values are expressed as percentages or as mean±standard deviation.
The angiographic data are summarized in table 2. Bifurcation lesions were more frequently located in the CTO of the left anterior descending artery (42.4%), followed by the right coronary artery (27.3%). CTO not involving BIF were predominantly located in the right coronary artery (67%), followed by the left anterior descending artery (16.1%) and the left circumflex coronary artery (10.5%). A blunt stump or no stump was identified in 69% of BIF-CTO lesions compared with 51.1% of non–BIF-CTO lesions (P<.001). BIF-CTO lesions also had more developed ipsilateral collaterals (48.2% vs 25.8%, P<.001). The characteristics of the remaining lesions and collateral circulation were similar between the 2 groups. The bifurcation was located at the proximal CTO cap in 63.7% of patients, followed by the distal CTO cap (29.8%), and the body of the occluded segment (6.5%).
Angiographic characteristics
| Variable | BIF-CTO(n=245, 40.4%) | Non–BIF-CTO-CTO(n=362, 59.6%) | All CTO patients(N=607) | P |
|---|---|---|---|---|
| Diseased vessels, No. | 1.85±0.72 | 1.86±0.73 | 1.86±0.73 | .907 |
| CTO vessel | ||||
| LM | 0.4 | 0.0 | 0.2 | .224 |
| LAD | 42.4 | 16.1 | 26.7 | <.001 |
| RCA | 27.3 | 67.0 | 51.0 | <.001 |
| LCX | 14.3 | 10.5 | 12.0 | .163 |
| Intermediate branch | 2.0 | 0.3 | 1.0 | .031 |
| Diagonal branch | 1.6 | 0.3 | 0.8 | .070 |
| Marginal branch | 8.6 | 3.6 | 5.6 | .009 |
| RCA branch | 0.8 | 1.4 | 1.2 | .539 |
| CTO location | ||||
| Ostial | 3.2 | 1.9 | 2.1 | .134 |
| Proximal | 39.1 | 38.0 | 38.5 | .115 |
| Mid | 49.1 | 51.0 | 50.5 | .162 |
| Distal | 8.6 | 9.1 | 8.9 | .821 |
| CTO vessel diameter, mm | 2.75±0.26 | 2.76±0.30 | 2.76±0.28 | .781 |
| CTO length, mm | 29.12±20.15 | 27.03±14.82 | 27.87±17.19 | .474 |
| CTO blunt stump | 69 | 51.1 | 58.3 | <.001 |
| Interventional collaterals | 95.1 | 93.1 | 93.9 | .306 |
| Ipsilateral collateral circulation | 48.2 | 25.8 | 34.8 | <.001 |
| Werner classification | .590 | |||
| CC0 | 0.5 | 1.1 | 0.8 | |
| CC1 | 22.4 | 15.3 | 18.2 | |
| CC2 | 77.1 | 83.6 | 81.0 | |
| CTO vessel calcification | .721 | |||
| Mild | 37.6 | 40.2 | 39.1 | |
| Moderate | 58 | 54.3 | 55.8 | |
| Severe | 4.5 | 5.6 | 5.1 | |
| Proximal tortuosity | .907 | |||
| Straight (< 70o 1 bend) | 66.1 | 68.7 | 67.7 | |
| Slight (> 70o 1 bend) | 24.1 | 21.3 | 22.4 | |
| Moderate (> 90o 1 bend,>70o 2 bends) | 0.4 | 0.3 | 0.3 | |
| Severe (> 120o 1 bend,>90o 2 bends) | 6.9 | 7.8 | 7.4 | |
| Non applicable | 2.4 | 1.9 | 2.1 | |
| Distal opacification | .131 | |||
| Absent/cannot be identified | 0.8 | 0.8 | 0.8 | |
| Faint | 43.7 | 35.6 | 38.8 | |
| Good | 55.0 | 63.6 | 60.3 | |
| Distal vessel disease | .202 | |||
| Absent | 20.4 | 25.0 | 23.1 | |
| Moderate | 79.6 | 74.4 | 76.5 | |
| Severe | 0.0 | 0.6 | 0.3 |
BIF-CTO, chronic total occlusion involving bifurcation lesion; CC, collateral channel classification according to Werner classification; CTO, chronic total occlusion; LAD, left anterior descending coronary artery; LCX, left circumflex coronary artery LM, left main coronary artery; RCA, right coronary artery.
Values are expressed as percentages or as mean±standard deviation.
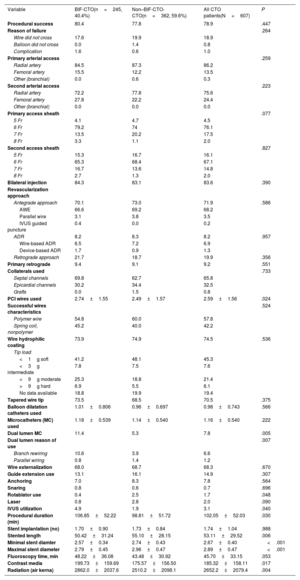
The procedural characteristics are summarized in table 3. Procedural success was 78.9% (BIF-CTO 80.4% vs non–BIF-CTO-CTO 77.8%; P=.447). The main reason for failure was unsuccessful wire crossing. The radial artery was used for primary arterial access in 86.2% of patients (P=.259 for the 2 cohorts) and for secondary arterial access in 75.6% of patients (P=.223 for the 2 cohorts). Bilateral injection was applied in 83.6% of patients. The predominant approach was antegrade wire escalation (66.6% in BIF-CTO vs 69.2% in non–BIF-CTO-CTO; P=.586). ADR was used in 8.2% of patients (6.9% wire-based ADR and 1.3% device-based ADR; P=.957). Retrograde techniques were applied in 21.7% of CTO involving a bifurcation and 18.7% of CTO without a bifurcation (P=.356). Septal collateral channels were used in 65.8% of retrograde cases, followed by epicardial channels (32.5%; P=.73 between the 2 arms). Hydrophilic wires were used in 74.5% of patients, with soft and intermediate stiffness wires (≤ 3 gr tip load) with success in 52.9% of CTOs (P=.58 between the 2 treatment arms). Dual lumen microcatheters were more frequently used in BIF-CTO (11.4% vs 5.3% of non–BIF-CTO; P=.005). IVUS use was higher in BIF-CTO (4.9% vs 1.9%, P=.040). Procedural duration, contrast media use and radiation dosage were also higher in patients with BIF-CTO.
Procedural data
| Variable | BIF-CTO(n=245, 40.4%) | Non–BIF-CTO-CTO(n=362, 59.6%) | All CTO patients(N=607) | P |
|---|---|---|---|---|
| Procedural success | 80.4 | 77.8 | 78.9 | .447 |
| Reason of failure | .264 | |||
| Wire did not cross | 17.6 | 19.9 | 18.9 | |
| Balloon did not cross | 0.0 | 1.4 | 0.8 | |
| Complication | 1.6 | 0.6 | 1.0 | |
| Primary arterial access | .259 | |||
| Radial artery | 84.5 | 87.3 | 86.2 | |
| Femoral artery | 15.5 | 12.2 | 13.5 | |
| Other (branchial) | 0.0 | 0.6 | 0.3 | |
| Second arterial access | .223 | |||
| Radial artery | 72.2 | 77.8 | 75.6 | |
| Femoral artery | 27.8 | 22.2 | 24.4 | |
| Other (branchial) | 0.0 | 0.0 | 0.0 | |
| Primary access sheath | .077 | |||
| 5 Fr | 4.1 | 4.7 | 4.5 | |
| 6 Fr | 79.2 | 74 | 76.1 | |
| 7 Fr | 13.5 | 20.2 | 17.5 | |
| 8 Fr | 3.3 | 1.1 | 2.0 | |
| Second access sheath | .827 | |||
| 5 Fr | 15.3 | 16.7 | 16.1 | |
| 6 Fr | 65.3 | 68.4 | 67.1 | |
| 7 Fr | 16.7 | 13.6 | 14.8 | |
| 8 Fr | 2.7 | 1.3 | 2.0 | |
| Bilateral injection | 84.3 | 83.1 | 83.6 | .390 |
| Revascularization approach | ||||
| Antegrade approach | 70.1 | 73.0 | 71.9 | .586 |
| AWE | 66.6 | 69.2 | 68.2 | |
| Parallel wire | 3.1 | 3.8 | 3.5 | |
| IVUS guided puncture | 0.4 | 0.0 | 0.2 | |
| ADR | 8.2 | 8.3 | 8.2 | .957 |
| Wire-based ADR | 6.5 | 7.2 | 6.9 | |
| Device-based ADR | 1.7 | 0.9 | 1.3 | |
| Retrograde approach | 21.7 | 18.7 | 19.9 | .356 |
| Primary retrograde | 9.4 | 9.1 | 9.2 | .551 |
| Collaterals used | .733 | |||
| Septal channels | 69.8 | 62.7 | 65.8 | |
| Epicardial channels | 30.2 | 34.4 | 32.5 | |
| Grafts | 0.0 | 1.5 | 0.8 | |
| PCI wires used | 2.74±1.55 | 2.49±1.57 | 2.59±1.56 | .024 |
| Successful wires characteristics | .524 | |||
| Polymer wire | 54.8 | 60.0 | 57.8 | |
| Spring coil, nonpolymer | 45.2 | 40.0 | 42.2 | |
| Wire hydrophilic coating | 73.9 | 74.9 | 74.5 | .536 |
| Tip load | ||||
| <1g soft | 41.2 | 48.1 | 45.3 | |
| <3g intermediate | 7.8 | 7.5 | 7.6 | |
| <9g moderate | 25.3 | 18.8 | 21.4 | |
| >9g hard | 6.9 | 5.5 | 6.1 | |
| No data available | 18.8 | 19.9 | 19.4 | |
| Tapered wire tip | 73.5 | 68.5 | 70.5 | .375 |
| Balloon dilatation catheters used | 1.01±0.806 | 0.96±0.697 | 0.98±0.743 | .566 |
| Microcatheters (MC) used | 1.18±0.539 | 1.14±0.540 | 1.16±0.540 | .222 |
| Dual lumen MC | 11.4 | 5.3 | 7.8 | .005 |
| Dual lumen reason of use | .007 | |||
| Branch rewiring | 10.6 | 3.9 | 6.6 | |
| Parallel wiring | 0.8 | 1.4 | 1.2 | |
| Wire externalization | 68.0 | 68.7 | 68.3 | .670 |
| Guide extension use | 13.1 | 16.1 | 14.9 | .307 |
| Anchoring | 7.0 | 8.3 | 7.8 | .564 |
| Snaring | 0.8 | 0.6 | 0.7 | .696 |
| Rotablator use | 0.4 | 2.5 | 1.7 | .048 |
| Laser | 0.8 | 2.8 | 2.0 | .090 |
| IVUS utilization | 4.9 | 1.9 | 3.1 | .040 |
| Procedural duration (min) | 106.85±52.22 | 98.81±51.72 | 102.05±52.03 | .030 |
| Stent implantation (no) | 1.70±0.90 | 1.73±0.84 | 1.74±1.04 | .988 |
| Stented length | 50.42±31.24 | 55.10±28.15 | 53.11±29.52 | .006 |
| Minimal stent diamter | 2.57±0.34 | 2.74±0.43 | 2.67±0.40 | <.001 |
| Maximal stent diameter | 2.79±0.45 | 2.96±0.47 | 2.89±0.47 | <.001 |
| Fluoroscopy time, min | 48.22±36.08 | 43.48±30.92 | 45.70±33.15 | .053 |
| Contrast media | 199.73±159.69 | 175.57±156.50 | 185.32±158.11 | .017 |
| Radiation (air kerna) | 2862.0±2037.6 | 2510.2±2098.1 | 2652.2±2079.4 | .004 |
ADR, antegrade dissection re-entry; AWE, antegrade wire escalation; BIF-CTO, chronic total occlusion involving bifurcation lesion; CTO, chronic total occlusion; FR, French size; IVUS, intravascular ultrasound; MC, microcatheter; PCI, percutaneous coronary intervention.
Values are expressed as percentages or as mean±standard deviation.
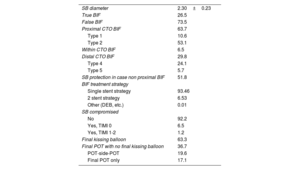
The angiographic and procedural characteristics of the BIF-CTO cohort (n=245) are summarized in table 4. A proximal optimization technique was applied in all treated bifurcation lesions. The SB diameter was 2.30±0.23mm. True bifurcations [Medina (1,1,1), (1,0,1), (0,1,1)] were observed in 26.5% of the lesions. Dissection of the SB ostium occurred in 6.5%. A single stent strategy was adopted in 93.4% of treated bifurcations, followed by 2-stent techniques in 6.5% (13 patients treated with T/TAP technique, 2 with mini crush, 1 with culotte). Of these, an upfront 2 stent strategy was adopted in 3 patients (1.2%). Kissing balloon dilatation was applied to 63.3% of patients. SB TIMI III flow was preserved in 92.2% of patients. SB compromise had no impact on procedural success (P=.081).
BIF-CTO cohort
| SB diameter | 2.30±0.23 |
| True BIF | 26.5 |
| False BIF | 73.5 |
| Proximal CTO BIF | 63.7 |
| Type 1 | 10.6 |
| Type 2 | 53.1 |
| Within CTO BIF | 6.5 |
| Distal CTO BIF | 29.8 |
| Type 4 | 24.1 |
| Type 5 | 5.7 |
| SB protection in case non proximal BIF | 51.8 |
| BIF treatment strategy | |
| Single stent strategy | 93.46 |
| 2 stent strategy | 6.53 |
| Other (DEB, etc.) | 0.01 |
| SB compromised | |
| No | 92.2 |
| Yes, TIMI 0 | 6.5 |
| Yes, TIMI 1-2 | 1.2 |
| Final kissing balloon | 63.3 |
| Final POT with no final kissing balloon | 36.7 |
| POT-side-POT | 19.6 |
| Final POT only | 17.1 |
BIF, bifurcation; BIF-CTO, chronic total occlusion involving bifurcation lesion; CTO, chronic total occlusion; DEB, drug eluting balloon; FKB, final kissing balloon; POT, proximal optimization technique; SB, sidebranch; TIMI, thrombolysis in myocardial infarction.
Values are expressed as percentages or as mean±standard deviation.
Baseline SB wiring was performed in all the bifurcations located proximal to the CTO, but in only 51.8% of the SB located within and distal to the CTO. Dual lumen microcatheters were used for SB wiring in 10.6% of the patients.
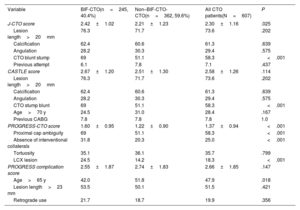
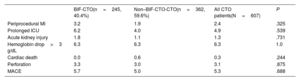
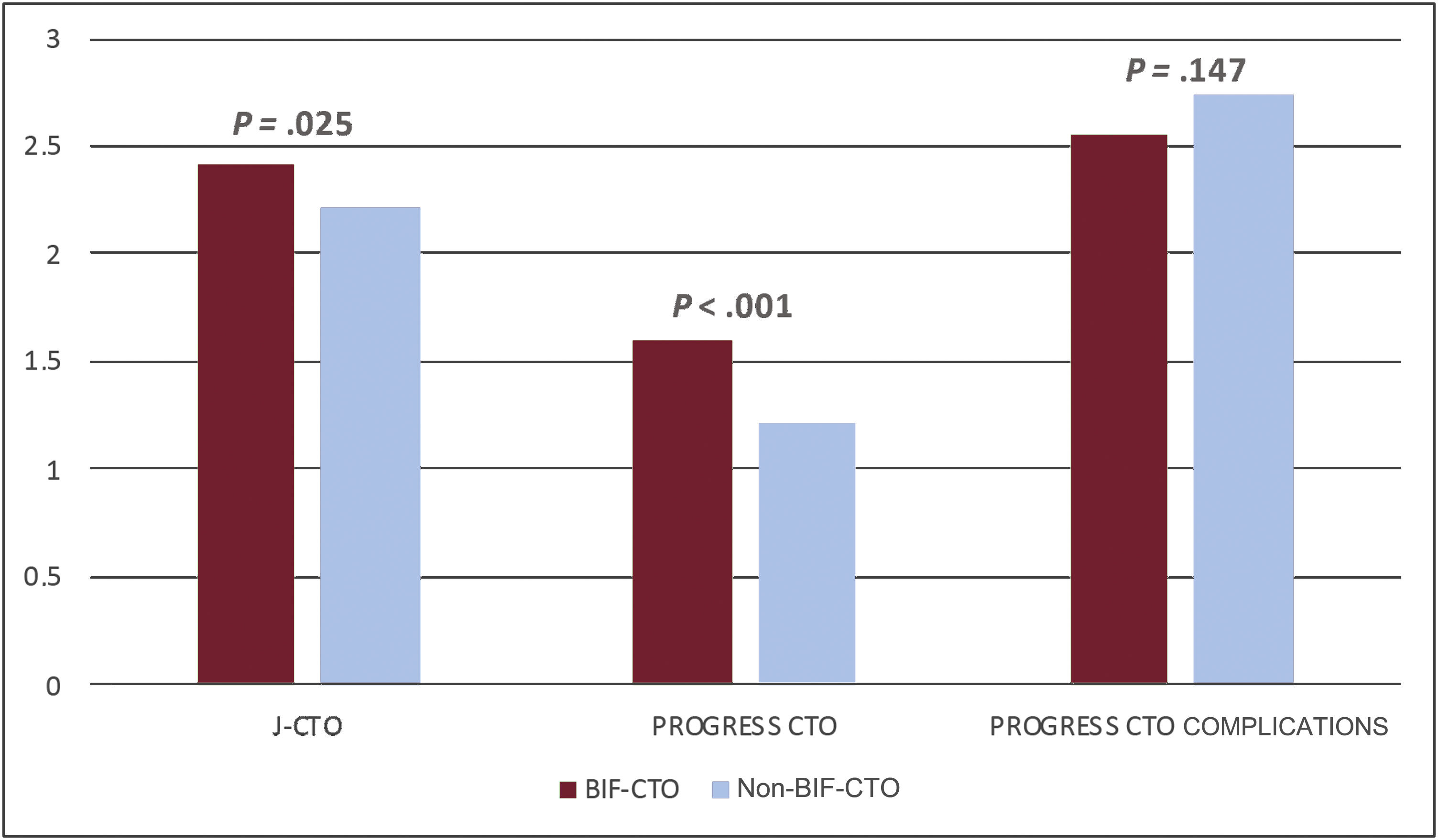
Procedural complexity was higher in BIF-CTO patients, as assessed by the Multicenter Chronic Total Occlusion Registry of Japan (J-CTO) (2.42±1.02 vs 2.21±1.23; P=.025) and Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS-CTO) (1.60±0.95 vs 1.22±0.90; P<.001) scores (figure 2). The PROGRESS-CTO complication score was similar in the 2 study cohorts (table 5). The complication rate was also similar between the 2 study cohorts (table 6). Periprocedural MI, as assessed by high sensitivity troponin T, was 2.4% overall and was higher for BIF-CTO patients, but without statistical significance (3.2% vs 1.9%; P=.325). The perforation rate was 3.1% and cardiac death was 0.3% overall. Prolonged stays in the intensive care unit, acute kidney injury and perforation rates were numerically higher in patients with BIF-CTO, but differences were nonsignificant.
Central illustration. CTO PCI predictive scores in 2 treatment cohorts (BIF-CTO and non–BIF-CTO-CTO patients). BIF-CTO, chronic total occlusion involving bifurcation lesion; CTO, chronic total occlusion; J-CTO, Multicenter Chronic Total Occlusion Registry of Japan; PCI, percutaneous coronary intervention; PROGRESS-CTO, prospective global registry for the study of chronic total occlusion intervention.
Predictive scores
| Variable | BIF-CTO(n=245, 40.4%) | Non–BIF-CTO-CTO(n=362, 59.6%) | All CTO patients(N=607) | P |
|---|---|---|---|---|
| J-CTO score | 2.42±1.02 | 2.21±1.23 | 2.30±1.16 | .025 |
| Lesion length>20mm | 76.3 | 71.7 | 73.6 | .202 |
| Calcification | 62.4 | 60.6 | 61.3 | .639 |
| Angulation | 28.2 | 30.3 | 29.4 | .575 |
| CTO blunt stump | 69 | 51.1 | 58.3 | <.001 |
| Previous attempt | 6.1 | 7.8 | 7.1 | .437 |
| CASTLE score | 2.67±1.20 | 2.51±1.30 | 2.58±1.26 | .114 |
| Lesion length>20mm | 76.3 | 71.7 | 73.6 | .202 |
| Calcification | 62.4 | 60.6 | 61.3 | .639 |
| Angulation | 28.2 | 30.3 | 29.4 | .575 |
| CTO stump blunt | 69 | 51.1 | 58.3 | <.001 |
| Age>70 y | 24.5 | 31.0 | 28.4 | .167 |
| Previous CABG | 7.8 | 7.8 | 7.8 | 1.0 |
| PROGRESS-CTO score | 1.60±0.95 | 1.22±0.90 | 1.37±0.94 | <.001 |
| Proximal cap ambiguity | 69 | 51.1 | 58.3 | <.001 |
| Absence of interventional collaterals | 31.8 | 20.3 | 25.0 | <.001 |
| Tortuosity | 35.1 | 36.1 | 35.7 | .799 |
| LCX lesion | 24.5 | 14.2 | 18.3 | <.001 |
| PROGRESS complication score | 2.55±1.87 | 2.74±1.83 | 2.66±1.85 | .147 |
| Age>65 y | 42.0 | 51.8 | 47.9 | .018 |
| Lesion length>23 mm | 53.5 | 50.1 | 51.5 | .421 |
| Retrograde use | 21.7 | 18.7 | 19.9 | .356 |
CABG, coronary artery bypass grafting; CASTLE, coronary artery bypass graft history, age, stump anatomy, tortuosity, length of occlusion, calcification; CTO, chronic total occlusion; J-CTO, Multicenter Chronic Total Occlusion Registry of Japan; LCX, left circumflex coronary artery; PROGRESS-CTO, prospective global registry for the study of chronic total occlusion intervention.
Values are expressed as percentages or as mean±standard deviation.
Complications
| BIF-CTO(n=245, 40.4%) | Non–BIF-CTO-CTO(n=362, 59.6%) | All CTO patients(N=607) | P | |
|---|---|---|---|---|
| Periprocedural MI | 3.2 | 1.9 | 2.4 | .325 |
| Prolonged ICU | 6.2 | 4.0 | 4.9 | .539 |
| Acute kidney injury | 1.8 | 1.1 | 1.3 | .731 |
| Hemoglobin drop>3 g/dL | 6.3 | 6.3 | 6.3 | 1.0 |
| Cardiac death | 0.0 | 0.6 | 0.3 | .244 |
| Perforation | 3.3 | 3.0 | 3.1 | .875 |
| MACE | 5.7 | 5.0 | 5.3 | .688 |
BIF-CTO, chronic total occlusion involving bifurcation lesion; CTO, chronic total occlusion; ICU, intensive coronary unit; MACE, major adverse cardiac events; MI, myocardial infarction.
Values are expressed as percentages or as mean±standard deviation.
Our study evaluated the incidence, procedural strategy, in-hospital outcomes and complications of CTO PCI involving bifurcation lesions treated in a high-volume European center at Massy, France. The main findings of our study were the following: a) the incidence of bifurcation-CTO was high; b) procedural complexity, as assessed by J-CTO and PROGRESS-CTO scores, was higher in CTO involving bifurcation lesions; c) the success rate of CTO PCI was high overall and was not affected by the presence of bifurcations at CTO lesions; d) the complication rate was unchanged between the 2 study cohorts, as was the PROGRESS-CTO complication score; e) the default bifurcation treatment strategy was a provisional approach, as is the case in nonocclusive coronary artery disease.
Incidence of bifurcation-coronary chronic total occlusionsPrevious series on bifurcation-CTO lesions reported an incidence ranging from 26.5% to 67%.13,15–18 In line with our study (40.4% incidence), Ojeda et al.17 (30.3%), Galassi et al.16 (26.5%) and Baystrukov et al.13 (54.3%) reported single-center experiences and used the same definitions (proximal, within the CTO body, distal bifurcation). Chen et al.18 reported proximal and distal SB arising from the CTO segment (47% incidence), whereas Nikolakopoulos et al.15 reported only bifurcation-CTOs with SB arising within 5mm of the proximal or distal cap (67% incidence).
Procedural success rate, revascularization strategy, predictive scoresProcedural success in our study was high, averaging 78.9%. Dedicated groups of experts worldwide have consistently reported success rates in the range of 90% in the last few years.5,19–23 In our study, the procedural complexity of the treated patients was relatively high (J-CTO score 2.30±1.16) compared with that reported in studies based on large scale European24 and Japanese registries.25 Of note, in 2018 the EuroCTO Club reported a mean J-CTO score of 2.37±1.14 in failed cases vs 2.08±1.15 in successful cases (P<.001; 17 626 procedures cohort).24
As per European practice,24 the predominant revascularization strategy was the antegrade approach (71.9%), followed by retrograde (19.9%) and ADR (8.2%). CTO crossing was successful with soft and moderate stiffness wires in most cases, reflecting contemporary technique and wire technology development.24
The overall J-CTO score and PROGRESS-CTO score in our study were 2.30±1.16 and 1.37±0.94, respectively. Procedural complexity was higher in CTOs involving a bifurcation lesion than in non–BIF-CTO, as assessed by both J-CTO score (2.42±1.01 vs 2.21±1.23; P=.025) and PROGRESS-CTO score (1.60±0.95 vs 1.22±0.90; P<.001) (figure 2). Similar to our study, Nikolakopoulos et al.15 reported a higher J-CTO score in BIF-CTO patients. All the other relevant studies reported data from relatively small cohorts and identified no differences in procedural complexity.13,16–18 The PROGRESS-CTO complication score was 2.66±1.85 overall and was similar in both arms (P=.147).
Coronary chronic total occlusions and bifurcation approachProcedural success was similar in the 2 treatment cohorts (80.4% for BIF-CTO patients, 77.8% for non–BIF-CTO patients; P=.447), even though procedural complexity was higher in patients with BIF-CTO, as assessed by J-CTO and PROGRESS-CTO scores (figure 2). All other relevant studies reported lower procedural success rates in CTO involving bifurcation lesions, with Galassi et al.16 reporting a single operator experience and Nikolakopoulos et al.15 reporting data from a global US registry. Compared with the above studies, in our cohort the provisional stenting strategy for bifurcation treatment was predominant (93.4%) and ADR techniques were infrequently adopted (8.2%).
Bifurcation treatment has greatly evolved over the years and has reached a period of standardization in terminology and practice.10 Provisional stenting has been established as the preferred treatment modality, since complex coronary interventions with 2 stents have been associated with greater periprocedural MI, target lesion revascularization, and mortality.26–28 In our study, the provisional strategy was the predominant approach and was applied in 93.46% of bifurcations, matching the results of other contemporary European cohorts.17 The ADR approach, by definition responsible for controlled vessel dissection in contemporary CTO PCI, had low adoption in our center (8.2% in BIF-CTO patients), accounting, to a certain extent, for the low use of techniques requiring 2-stent implantation (6.5%).
In the context of CTO PCI, the presence of dissection affecting the SB origin has been identified as a predictor for the adoption of the 2-stent strategy,17 leading to a 46% adoption of 2-stent techniques in a single operator cohort.16 Larger studies reported the use of the 2-stent technique in the range of 8% to 8.9%.17,29 Adachi et al.29 reported that 2-stent techniques were more efficient in preserving SB patency for bifurcations located within the CTO body. Ojeda et al.30 reported no differences in procedural and mid-term clinical outcomes between 1-stent and 2-stent techniques for the treatment of CTO bifurcation lesions. Interestingly, a single center randomized study comparing the mini crush technique and the provisional approach in CTOs involving bifurcation lesions revealed no differences in angiographic or clinical success but did reveal improved 1-year outcomes with the mini crush technique.13
Side branch patencySB patency with TIMI III flow was achieved in 92.2% of the bifurcations treated. Baseline SB wiring, a well identified predictor of procedural success in non-CTO bifurcation PCI, 31 was achieved in all SBs located proximal to the CTO, but in only 51.8% of the SBs located within or distal to the CTO. A previous study reported unsuccessful baseline SB wiring in 25% of nonproximal BIF-CTO,17 which can be largely attributed to dissections involving the carina during CTO crossing. A dual lumen microcatheter was used for SB wiring in 10.6% of the patients.
SB compromise is a well identified cause of periprocedural myocardial injury in coronary interventions.32 In the context of CTO PCI, Adachi et al.29 identified the presence of stenosis in the SB, bifurcations located within the occluded segment and subintimal tracking at the SB ostium as independent predictors of a suboptimal result in SB. In that study, a suboptimal SB result itself, had an impact on target lesion revascularization of the main branch for lesions located in the right coronary artery.29 Another single-center CTO PCI study identified SB occlusion as the only parameter associated with troponin elevation during the procedure.33 Elevation of cardiac biomarkers reflects myocardial necrosis and has been linked to an increased risk of future cardiac events.33–35
ComplicationsIn this study, the presence of a bifurcation had no impact on the in-hospital complication rate following CTO revascularization. In our cohort, the key determinants for this result were operator expertise, a predominantly provisional stenting strategy for bifurcation treatment (93.4%), and low adoption of dissection re-entry techniques for CTO crossing (8.2%). Prior studies identified higher periprocedural MI17 and more frequent coronary perforation and cardiac tamponade in CTOs with bifurcation lesions.16 In the first study, ADR was applied in up to 31% of the cases and in the second study, 1-stent techniques for bifurcation treatment were applied in only 54% of the patients. In our cohort, periprocedural MI was documented in 2.4% of the patients overall. Of note, periprocedural MI in CTOs involving bifurcations seems to affect MACE-free survival and mortality at 12 months.17,36
LimitationsOur study has a number of limitations. First, all patients in our registry were treated by experienced operators, with varied experience in CTO treatment and extensive experience in the treatment of bifurcation lesions. The data presented in this study reflect their practice and might not be generalizable to centers with limited complex PCI experience. Second, this is an observational retrospective single center study, with all the inherent bias of this kind of design. Yet, no randomized data are available on this topic. Third, the angiographic data were estimated by visual assessment only; no quantitative coronary angiographic analysis or core laboratory adjudication was performed. Fourth, no follow-up was available in our study.
CONCLUSIONSCoronary CTO and bifurcation lesions are both cornerstone anatomical entities in the field of complex PCI, which has evolved dramatically over the last decade due to technique standardization and technological advances. These entities coexist in 40.4% of contemporary CTO PCI, increasing the procedural complexity of treated patients. The presence of bifurcation has no impact on the procedural success rate, which remains high. The complication rate of CTO PCI is unaffected by the presence of bifurcation. A provisional approach provides excellent results and should be the preferred treatment strategy, as is in nonocclusive coronary artery disease. Further studies are required to investigate CTO PCI involving bifurcation lesions, focusing on procedural effectiveness, safety, and long-term outcomes.
- -
The incidence of bifurcation lesions in CTO ranges from 26.5% to 67% in contemporary literature.
- -
Prior studies have shown that the procedural success rate of CTO PCI is lower in CTOs involving bifurcations than in CTOs without bifurcations.
- -
The complication rate of PCI for CTOs has been reported to be higher in CTOs involving bifurcations.
- -
The incidence of bifurcation lesions in CTO was 40.4%.
- -
BIF-CTO patients presented with higher lesion complexity, as assessed by the J-CTO score and PROGRESS-CTO score.
- -
In contemporary CTO PCI, the presence of a bifurcation in a CTO lesion had no impact on the procedural success rate or the complication rate when ADR adoption was low and a provisional stenting strategy was the predominant approach.
This study received no funding.
AUTHORS’ CONTRIBUTIONSN.V. Konstantinidis: conceptualization, methodology, formal analysis, investigation, resources, writing original draft, reviewing, editing. B. Chevalier: methodology, investigation, resources, writing, reviewing and editing, validation, supervision. T. Hovasse: investigation, resources. P. Garot: investigation, resources. H. Benamer, T. Unterseeh, S. Champagne, F. Sanguineti, A. Neylon, A. Avran, Y. Louvard: investigation, resources. T. Moysiadis: formal analysis, data curation. T. Lefèvre : conceptualization, methodology, investigation, resources, writing, reviewing, editing, validation, supervision.
CONFLICTS OF INTERESTP. Garot is a medical shareholder of CERC, a CRO dedicated to cardiovascular research. He has received speaker's fees from Abbott, Biosensors, Boston Scientific, Edwards, Terumo, and GE Healthcare outside the submitted work. F. Sanguineti has received support for attending the PCR London Valve and the EBC Main meeting. A. Neylon has received honoraria from Medtronic, Shockwave Medical, and Boston Scientific. She has received support for attending meetings from Medtronic. She is a medical shareholder of CERC, a CRO dedicated to cardiovascular research. T. Lefèvre has received speaker's fees from Terumo, Boston Scientifics, and Edwards. He has a leadership role in the European Society of Cardiology, Euro PCR, and London Valve. The remaining authors have no conflicts of interest to disclose.
.