Congenital aortic valve disease accounts for 3% to 6% of congenital heart diseases, and in many cases requires surgical treatment. The options are limited by the child's weight and development. Percutaneous procedures (balloon valvuloplasty) and surgical interventions (surgical valvuloplasty or aortic valve replacement [AVR]) are both available. The initial approach varies depending on the underlying lesion and the policies of each center, and is a subject of international debate. When surgical repair is unfeasible, the alternative is AVR, and the options depend on the size of the aortic ring. Three techniques predominate in children: prosthesis implantation, Ross surgery, and homograft implantation. They are all known to have certain difficulties and problems.
In 2011, Ozaki et al.1 described an easily reproducible technique used in adults to reconstruct the aortic leaflets with autologous pericardium, known as aortic valve neocuspitization (AVneo). The technique was adopted for the pediatric population by a group in Boston in 20152 and our center incorporated its use in 2019. To our knowledge, this is the first reported series of patients with congenital disease treated in this manner in Spain.
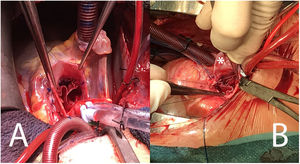
We present the results of 11 patients (comparing those younger and older than 18 years), undergoing surgery between October 2019 and July 2021. Quantitative variables are expressed as the median [interquartile range] and qualitative variables as the number (percentage). The Wilcoxon test was used for quantitative variables and the Fisher test for qualitative variables. None of the patients required conversion to a prosthesis. One underwent on-pump reentry to enlarge a stenotic sinus of Valsalva at the level of the commissures. The demographic, procedure-related, and follow-up data are shown in table 1. In all cases, reconstruction of the 3 leaflets was performed on a bicuspid or unicuspid valve with neoleaflets of the same size (figure 1A). Associated procedures were carried out in 3 patients: subaortic membrane resection, annular enlargement, and sinus of Valsalva enlargement. The median duration of follow-up was 12.09 [5.8-20.6] months, with good gradients (table 1). One patient experienced moderate or greater aortic regurgitation due to mobility loss of 1 leaflet. All patients remain asymptomatic and none have undergone a new procedure.
Demographic, surgical, and postoperative variables
| Total (n=11) | Younger than 18 y (n=6) | Older than 18 y (n=5) | P | |
|---|---|---|---|---|
| Age, y | 15.77 [8.46-29.07] | 9.28 [7.32-10.96] | 29.07 [26.67-32.95] | .006 |
| Males | 5 (45) | 3 (50) | 2 (40) | 1 |
| Weight, kg | 48 [29-67] | 32 [23-48] | 67 [65-78] | .006 |
| Previous surgery | 1 (9) | 1 (17) | 0 | 1 |
| Previous balloon valvuloplasty | 6 (54.6) | 4 (66.7) | 2 (40) | 1 |
| Asymptomatic | 7 (64) | 4 (67) | 3 (60) | 1 |
| Aortic valve morphology | 1 | |||
| Tricuspid | 0 | 0 | 0 | |
| Bicuspid | 8 (73) | 4 (67) | 4 (80) | |
| Unicuspid | 3 (27) | 2 (33) | 1 (20) | |
| Mean peak gradient, mmHg | 70.5 [46-95] | 58 [35-71] | 88 [75.5-99.5] | .16 |
| Mean gradient, mmHg | 42 [35-50] | 35 [21-45] | 46 [41.5-57] | .22 |
| AR ≥ moderate | 9 (82) | 6 (100) | 3 (60) | .18 |
| Aortic ring, mm | 20 [18-24] | 18 [17-20] | 24 [23-27] | .01 |
| Associated procedure | 3 (27) | 3 (50) | 0 | .18 |
| CPB time, min | 150 [143-184] | 169.5 [149-203] | 148 [140-150] | .1 |
| Ischemia time, min | 134 [120-148] | 142 [125-160] | 129 [120-134] | .27 |
| Conversion | 0 | 0 | 0 | 1 |
| Re-entry in CPB | 1 (9) | 1 (17) | 0 | 1 |
| OTI time, h | 3 [2-7] | 3.5 [2-16] | 3 [2-3] | .45 |
| ICU stay, d | 3 [2-4] | 3.5 [2-4] | 3 [3-3] | .44 |
| Hospital stay, d | 7 [7-8] | 7.5 [7-10] | 7 [7-8] | .57 |
| Mortality | 0 | 0 | 0 | 1 |
| Peak gradient at discharge, mmHg | 24 [18-38] | 22 [20-35] | 36 [12-38] | 1 |
| Mean gradient at discharge, mmHg | 16 [8-22] | 14 [10-19.5] | 20 [7-22] | .81 |
| AR ≥ moderate-severe | 0 | 0 | 0 | 1 |
| Reintervention (percutaneous or surgical) | 0 | 0 | 0 | 1 |
| Peak gradient at follow-up, mmHg | 24 [19-30] | 24 [19-45] | 23.5 [14.5-28] | .67 |
| Mean gradient at follow-up, mmHg | 16 [12-21] | 21.5 [21-22] | 12 [11-16] | .083 |
| AR ≥ 3 at follow-up | 1 (9) | 1 (17) | 0 | 1 |
AR, aortic regurgitation; CPB, cardiopulmonary bypass; ICU, intensive care unit; OTI, orotracheal intubation.
Values are expressed as No. (%) or median [interquartile range].
A: final view of the Ozaki technique following reconstruction of the 3 leaflets. B: most complex case in our series, surgically treated using PhotoFix heterologous pericardium (Cryolife, United States) to create the neoleaflets and a pericardial patch (asterisk) to enlarge the aortic ring.
Ozaki performed the AVneo technique in 1100 adults, with excellent survival and reoperation-free rates (84.6% and 95.8%, respectively, at 12 years) following a mean follow-up of 4.475 years.3 Among the advantages of AVneo is the possibility to use it in any age group3 and valve morphotype.4,5 In addition, the aortic ring motility is preserved.6 This allows annular expansion in systole and improves the effective orifice area, thus providing better hemodynamic results and persistently low gradients over time. Furthermore, the greatly elevated coaptation height reduces stress and tension at the commissures and could be related to the durability observed at mid-term.
The Boston group reported their results in 57 patients (mean age, 12.4 years), with a median follow-up of 8 months. Survival and freedom from reoperation was 91% at 1.5 years, and freedom from moderate or greater aortic regurgitation was 88% at 2 years. The population with congenital disease showed some differential characteristics: in 70%, previous surgery compelled the use of heterologous pericardium, and 28 patients underwent aortic ring enlargement due to hypoplasia.2
In our series, the subgroup of patients younger than 18 years showed a more complex profile than the adults. One patient underwent surgery twice, enlarging the ring to enable implantation of 15-mm neoleaflets (figure 1B), and 50% of patients had an associated procedure. The outcome was favorable in both subgroups, with no deaths or reoperation requirements.
In pediatrics, an outstanding feature of this technique is that it allows growth of the aortic ring as the child develops.3 It is hypothesized that this factor, coupled with the high leaflet coaptation, will result in proper neovalve function for a longer time without developing regurgitation. In contrast, it is currently unknown whether the implanted tissue will be affected by calcification, as has been observed in the literature. Another benefit in pediatrics is that there is no need for anticoagulation. Ozaki prescribed aspirin for 6 months, whereas the Boston group preferred 3 months of anticoagulation and aspirin. In our center, aspirin is maintained indefinitely.
In our opinion, AVneo use in the pediatric population and in young women as an alternative to Ross surgery is a welcome, very positive option. The technique is reproducible and relatively simple, the duration of cardiopulmonary bypass and myocardial ischemia is similar, it can be used on small annuli after enlargement without using the right ventricular outflow tract, and it leaves open the possibility of future Ross surgery, if required. Taken together, these reasons more than justify incorporation of AVneo in our catalog of procedures. It is postulated to be a good option for aortic annuli at least 13mm in size and has shown encouraging results. Nonetheless, caution is required and the mid- and long-term outcomes should be confirmed.
FUNDINGThis study received no funding.
AUTHORS’ CONTRIBUTIONSA. González Rocafort, the first author, conceived the initial idea, collected the data, and produced the initial version of the manuscript. L. Polo López and T. Centella Hernández, both senior authors, revised the initial version. B. Ramchandani Ramchandani and A. González Rocafort analyzed the data. J. Rey Lois and R. Sánchez collaborated in the interpretation of the data. All authors have critically reviewed the manuscript and approved the final version.
CONFLICTS OF INTERESTAll authors declare no conflicts of interest.