INTRODUCTION
The advances made in the study of atherosclerosis in recent decades have led to its understanding as an inflammatory disease and have been vital in unveiling the pathophysiology of acute coronary syndrome (ACS).1 The determination of the levels of inflammatory markers is a novel tool useful in establishing the prognosis of patients with ACS.2,3 Knowledge of these markers allows the most effective treatment to be selected, and helps when taking decisions on whether to follow a conservative or invasive strategy and whether revascularization is indicated.4 The level of C-reactive protein (CRP) can be used to identify patients with the most complicated coronary lesions and the greatest degree of intracoronary thrombosis, but can also help identify patients with apparently non-complex lesions that are susceptible to rupture--a problem that would lead to patient instability.5-10
The prognostic value of the CRP concentration is, however, still under study, and it has not yet become a recommended laboratory test for use in risk stratification. Conflicting clinical data exist with respect to its prognostic value, probably a reflection of the different times when samples were taken and the wide variation in the results obtained.2-4,11 Although an increase in the CRP concentration is thought to be due to the activation of the inflammatory process owing to (or perhaps the cause of) coronary instability, the CRP level is directly associated with the degree of myocardial necrosis,12 and does not appear to increase after an episode of ischemia in patients with variant angina with no evidence of myocardial necrosis.13
The kinetics of CRP have been studied in the context of acute myocardial infarction (AMI), but no papers have analyzed the CRP release curve with respect to the new definition of AMI proposed by the European Society of Cardiology and the American College of Cardiology.14 Neither have any clinical studies looked closely at the increase in CRP levels in patients with unstable angina but with no evidence of myocardial necrosis. The aim of the present work was, therefore, to study the kinetics of CRP release in patients with different clinical forms of ACS. Improved knowledge in this area could help us better understand the significance of CRP values, improve pharmacological therapies, and help improve the design of research projects examining the prognostic significance of CRP levels over the ACS spectrum.
METHODS
The study subjects were 110 consecutive patients who were admitted to our heart unit with a final diagnosis of ACS of the following types: ST-elevation acute myocardial infarction (STEMI; n=42), non ST-elevation acute myocardial infarction (NSTEMI; n=35), and unstable angina (n=33). The distinction between infarction and unstable angina was made using the new definition of AMI proposed by the European Society of Cardiology and the American College of Cardiology.14 The following patients were excluded: those with a body temperature of >37.8°C at admission, those with complete left bundle block, those with pacemaker rhythm, and those with serious aortic valve disease, obstructive hypertrophic cardiomyopathy, renal failure (on dialysis), or any chronic inflammatory disease that might alter the significance of the markers studied. Also excluded were those who had undergone surgery in the previous three months, those who had suffered a coronary or cerebral event in that same period, those who had experienced chest pain in the last few days, those with non-coronary chest pain or stable angina, those who were diagnosed with unstable angina not falling into the Braunwald IIIB classification,15 and those who died during their stay in hospital. The 110 patients actually selected therefore originally belonged to a larger population of 150 consecutive patients admitted over a 5 month period, and represent 73.3% of this original group.
All patients underwent a 12-lead electrocardiogram (ECG) at admission. According to the result, and to those of the enzymatic curve, the patients were divided into 3 groups: STEMI, NSTEMI, and unstable angina patients.
Peripheral venous blood was taken for the determination of CRP, troponin I, creatine kinase (CK), and the MB isoenzyme of CK (CK-MB) at admission and again at 6, 12, 18, 24, 30, 36, and 48 h. The concentration of CRP (expressed as mg/L) was further determined every day until discharge. All CRP concentrations were determined by turbidometry using a high sensitivity commercial kit (Hitachi 911; Boehringer Mannheim).16 Troponin I (expressed as ng/mL) was determined by immunoenzyme assay using the Access® system from Beckman. Creatine kinase (expressed as U/L) was determined by an enzymatic kinetic method using the Synchron cx® system from Beckman. The concentration of CK-MB (expressed as U/L) was measured in the same way. The normal values of these biomarkers were taken as: CRP, 3 mg/L; troponin I, 0.1 ng/mL; CK, 195 U/L, and CK-MB, 9 U/L. The area under the receiver operating characteristic (ROC) curve was determined by the linear-trapezoid method of Vollmer et al.17
Since the CRP levels were not normally distributed they are expressed in terms of the median and range (25th and 75th percentiles). Time was expressed in the same way. The Kruskal-Wallis test was used to compare the quantitative variables (CRP, troponin I, CK, and CK-MB) of the 3 patient groups. Spearman correlation coefficients were calculated to determine the correlation of pairs of quantitative variables. To calculate the area under the curve, CRP values were neperian log-transformed to meet the conditions of normality. Significance was set at P<.05 in all tests.
RESULTS
The demographic characteristics and cardiovascular risk factors of the studied population were similar to those of other Spanish patients.18 No significant differences were seen in these respects between the 3 patient groups, although the unstable angina patients showed a trend towards being older, having ischemic heart disease, and of receiving treatment with beta-blockers (Table 1). The median CRP value differed from baseline at 6 h (5 [2-9] mg/L at baseline compared to 6 [3-10] mg/L at 6 h; P=.004). Although the CRP levels were similar in all 3 groups at admission, the maximum values reached in each differed significantly P<.001) (Figure 1). The highest CRP level was seen at 48 h after admission. The maximum value in the STEMI group was reached later than in the other groups. Table 2 shows the CRP concentrations at admission, the maximum CRP levels, and the time elapsed before these were reached.
Figure 1. Time course of C-reactive protein concentration in each type of acute coronary syndrome. The normal reference value used was 3 mg/L.
The correlation between the CRP concentration and that of troponin I at admission was not significant (r=0.135). However, the maximum CRP value was influenced by the degree of myocardial necrosis (r=0.496; P<.001). This positive correlation was seen in all patients with AMI.
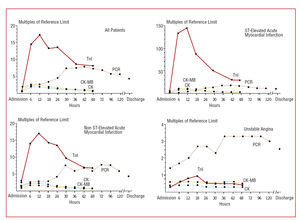
The highest CRP concentration was seen later than the peaks of the other markers of myocardial necrosis (P<.001), for all groups together and for each group separately (Figure 2).
Figure 2. Time courses of increase in levels of troponin I (TnI), creatine kinase (CK), CK-MB, and C-reactive protein, for the patients as a whole and by individual group. The normal values for the levels of these biomarkers were taken as: CRP, 3 mg/L; troponin I, 0.1 ng/mL; CK, 195 U/L; and CK-MB, 9 U/L.
Twenty four of the 35 NSTEMI patients (68.6%) and 16 of the 33 (48.5%) with unstable angina underwent percutaneous revascularization during their stay in hospital; no differences were seen in the CRP peak reached in these patients or in the time taken to reach them.
All but 3 STEMI patients received fibrinolytic treatment. At admission, patients with ECG signs of reperfusion had CRP concentrations of 4 mg/L compared to 5 mg/L in those who did not respond to fibrinolysis, and a maximum of 41 mg/L compared to 50 mg/L respectively; thus, these values were similar in patients who showed and who did not show signs of reperfusion. However, the area under the serum CRP time curve was smaller in patients who showed signs of reperfusion (663 [188-1.244] compared to 770 [310-2.067] mg/L*h in those who showed no such signs), although the difference was not significant (P=.102) (Figure 3). Reperfusion success was understood as a reduction in ST elevation of about 70% at 3 h after starting fibrinolytic treatment compared to that recorded at admission.19 The area under the CRP time curve was significantly greater in STEMI patients than in NSTEMI patients (761 [344-1426] mg/L*h compared to 345 [150-987] mg/L*h), and that of the NSTEMI patients greater than that of the unstable angina patients (206 [119-492] mg/L*h). The correlation between the area under the CRP time curve and the degree of myocardial necrosis was r=0.511 (P<.001).
Figure 3. Area under the CRP time curve in patients receiving fibrinolytic treatment depending on whether or not they showed electrocardiographic signs of reperfusion.
Finally, at discharge (8 [7-11] days), an overall 19% of patients had CRP values equal to or lower than those recorded at admission. This percentage was slightly lower (but not significantly so) in the STEMI patients (12%) than in the NSTEMI (21%) or unstable angina patients (26%).
DISCUSSION
The present results describing the dynamics of CRP clearly show that acute ischemic heart disease--even unstable angina--is associated with an inflammatory process. The CRP concentration at admission was similar in all 3 patient groups, but at 12 h after the onset of symptoms these values depended on the degree of myocardial necrosis incurred.
In patients with ACS, an increase in the CRP level at admission is associated with a poorer short term and long term prognosis.2,3 The majority of authors concur in that the admission CRP value reflects the baseline inflammatory status of the patient; thus, patients with ACS and high CRP levels at admission usually experience more important cardiovascular complications during follow-up. However, and in agreement with recent findings, the concentrations of CRP increase 12 h after the onset of symptoms.1.2 This increase in CRP concentration does not depend exclusively on the degree of necrosis since, unlike that reported by Liuzzo et al,20 the present patients with unstable angina and no increase in the concentration of myocardial damage markers showed a typical CRP curve with significant changes in concentration over time. This shows that: a) individual variability in the immune response and systemic inflammatory activation during ACS also influence the increase in CRP level,21 and b) the contrasting clinical data regarding the prognostic value of CRP levels probably derive from differences in the moment when they were determined and variations in the results obtained.2-4,11
Since the maximum CRP level occurs at around 48 h after the onset of symptoms, and given that the good correlation between this maximum and the value determined within 48 h (r=0.960, P<.001), there is no need continue monitoring CRP levels after this time. The higher the maximum CRP recorded, the more serious the infarction suffered, the greater the likelihood of ventricular remodeling, the lower the ejection fraction, and the greater the risk of heart failure, heart rupture, and death.22,23 Nevertheless, given the correlation between peak CRP level and the degree of necrosis, the maximum CRP probably provides no additional information over that provided by the maximum values of troponin, CK or CK-MB in AMI. In patients with unstable angina and no evidence of myocardial damage, however, determining the CRP level might be of prognostic value, and would help in the selection of the best medical treatment, when taking the decision of whether to follow an invasive or conservative strategy, and when deciding whether or not to attempt revascularization.
Initial physiological data are available that identify the failure of fibrinolytic treatment in patients with STEMI to be related to inflammatory status.24 High CRP values at admission allow the identification of patients in whom fibrinolytic treatment is likely to fail. In the present work, the CRP level at admission was slightly higher in patients with no ECG signs of reperfusion, although no significant association was seen. However, those who showed signs of having achieved reperfusion also showed a tendency to reach the CRP peak earlier and to have a smaller area under the serum CRP time curve. A detailed analysis of the relationship between inflammation and the failure of fibrinolytic treatment might require a larger sample size.
Finally, at the time of discharge only 19% of the patients as a whole had CRP values equal to or below those recorded at admission. A recent report indicates that a high CRP level at discharge can independently predict future cardiovascular complications,25 although the type of ACS suffered by the patient needs to be taken into account.
In conclusion, the CRP concentration ranges over a spectrum of vawes according to the type of ACS suffered. This should be taken into account when designing new studies with the aim of evaluating the prognostic value of the CRP concentration in such patients.
This work was partly financed by the Red Temática de Enfermedades Cardiovasculares (RECAVA).
Correspondence:
Dr. P.L. Sánchez.
Instituto de Ciencias del Corazón (ICICOR). Hospital Clínico de Valladolid.
Ramón y Cajal, 3. 47005 Valladolid. España.
E-mail: pedrolsanchez@secardiologia.es
Received May 24, 2005.
Accepted for publication January 31, 2006.