Surgical aortic valve replacement (SAVR) can modify the natural history of severe aortic stenosis (SAS). However, compared with the general population, these patients have a loss of life expectancy. The life expectancy of patients who undergo SAVR due to low-gradient SAS with preserved left ventricular ejection fraction (LVEF) is unknown.
MethodsWe included all patients between 50 and 65 years who underwent isolated SAVR in 27 Spanish centers during an 18-year period. We analyzed observed and expected survival at 18 years in patients with low-gradient SAS with preserved LVEF and all other types of SAS. We used propensity score matching to compare the life expectancy of patients with low-gradient SAS with preserved LVEF vs those with high-gradient SAS with preserved LVEF.
ResultsWe analyzed 5084 patients, of whom 413 had low-gradient SAS with preserved LVEF. For these patients, observed survival at 10, 15 and 18 years was 86.6% (95%CI, 85.3-87.8), 75% (95%CI, 72.7-77.2), and 63.5% (95%CI, 58.8-67.8). Expected survival at 10, 15 and 18 years was 90.2%, 82.1%, and 75.7%. In the matched sample, survival of patients with low-gradient SAS with preserved LVEF was similar to that of patients with high-gradient with preserved LVEF, log-rank test, P=.95; HR=1 (95%CI, 0.7–1.4; P=.95).
ConclusionsThere is a loss of life expectancy in patients with all types of SAS undergoing SAVR. This loss is higher in patients with left ventricular dysfunction and lower in patients with low-gradient or high-gradient aortic stenosis with preserved LVEF. The benefit of surgery is similar between these last 2 groups.
Keywords
Surgical aortic valve replacement (SAVR) has been shown to modify the natural history of symptomatic severe aortic stenosis (SAS). Nevertheless, compared with the general population of the same age and sex, some recent studies have shown that patients undergoing this intervention have a loss of life expectancy.1–3 This loss seems small in elderly individuals but high in young patients.
Low-gradient SAS with preserved left ventricular ejection fraction (LVEF) is an infrequent type of SAS (5-20% of all SAS).4 The reason underlying this low-gradient despite preserved LVEF is a decline in left ventricular filling secondary to concentric hypertrophy with restrictive diastolic pattern, atrial fibrillation or mitral regurgitation.4 This entity is increasingly important due to the observed poor prognosis after its diagnosis. Some small studies have reported that patients with this type of SAS have, compared with those with high-gradient SAS and preserved LVEF, almost twice the risk of dying in the year after diagnosis.5,6 Nevertheless, studies based on life expectancy after surgery are single-center analyses, based on small sample sizes, with relatively short follow-up periods and highly heterogeneous samples with concomitant coronary disease or other valvulopathies.5–9 In addition, any survival data, not compared with the survival data of the general population, provides little information.
We used a national registry to determine the observed and expected survival of young patients undergoing isolated SAVR due to low-gradient SAS with preserved LVEF. We also calculated the observed and expected survival of other types of SAS. Finally, we compared the prognosis of patients with low-gradient SAS with preserved LVEF with that of patients who had high-gradient SAS with preserved LVEF.
METHODSThis work was prepared in compliance with international recommendations on clinical research (Declaration of Helsinki of the World Medical Association revised in October 2013). It was approved by the Independent Ethics Committee of Malaga (Spain). Due to its retrospective nature, informed consent was waived.
Sample selection of the sampleWe used a national multicenter registry including all patients aged 50 to 65 years who underwent isolated SAVR in 27 Spanish centers between January 2000 and September 2018. We excluded endocarditis, nonelective operations and surgery due to isolated aortic regurgitation. We also excluded patients with concomitant mitral or tricuspid intervention or surgery for ascending aortic aneurysm. Each center had 2 researchers responsible for collecting pre-, intra- and postoperative data and for follow-up of all patients. Information on follow-up was collected based on medical reports, telephone contacts with the patient/family and contacts with their physicians. Only 3 patients were lost to follow-up. For these patients we considered the last date they were known to be alive.
In the registry, there were 4 different types of SAS: a) low-gradient (mean gradient<40mmHg) with preserved LVEF (LVEF ≥ 50%); this is paradoxical SAS, b) high-gradient with preserved LVEF, c) high-gradient with low LVEF, and d) low-gradient with low LVEF. Because reduced LVEF is a well-known risk factor for short- and long-term mortality, we decided that patients with high-gradient SAS and preserved LVEF and those with high-gradient SAS and reduced LVEF should be analyzed separately.10
We calculated the long-term observed survival of these patients who underwent isolated SAVR with the expected survival of the general population from Spain matched by age, sex and year of surgery. To match for these factors, we used the data freely available and provided by the National Institute of Statistics.11 This method has been previously used.1,2
Primary endpointsThere were 2 primary endpoints: a) observed and expected survival of patients who underwent SAVR due to low-gradient SAS and preserved LVEF; and b) to compare survival in patients who underwent SAVR due to low-gradient SAS and preserved LVEF with that in patients with high-gradient SAS and preserved LVEF.
Secondary endpointsSecondary endpoints consisted of observed and expected survival of the other types of SAS.
Statistical analysisContinuous variables are expressed as the mean value±standard deviation and were compared using the t-test for equal or unequal variances. The robust Levene test was used for equality of variance. Categorical variables are expressed as number (percentage) and were compared using the Fisher exact test.
We compared observed survival, calculated by the usual actuarial estimate (intervals of 0.5 years), with expected survival, calculated by the Ederer II method. This method, considered the best for this purpose,12 can estimate the expected survival of the sample under the theoretical assumption that they did not have the disease. This methodology was previously used in other works.1,2 If the 95% confidence interval (95%CI) of the observed survival included the expected survival, no difference can be shown. We also calculated the probability of death due to the disease based on a competing risk framework, by using the method proposed by Cronin and Feuer et al.13 For the calculations, we used the data provided by the National Institute of Statistics.11
Finally, we aimed to compare the prognosis of patients who underwent surgery due to low-gradient SAS with preserved LVEF and those that had high-gradient SAS with preserved LVEF. To control for selection and confounding factors we controlled for all baseline variables using the propensity score matching technique. We used the nearest neighbor 1:1 with no replacement, greedy matching, and a caliper of 0.05.14 Because the P value depends on sample size, baseline variables after the matching were compared using standardized mean differences. Absolute values over 0.1 (10%) in the standardized mean differences indicate substantial differences between both groups.15,16 Balance diagnostics were performed comparing standardized mean differences and evaluating graphics. The hazard ratio was calculated to estimate the risk of death and 95%CI were calculated using 1000 bootstrap replications.17 As a sensitivity analysis, we created a Cox-regression model with a frailty factor (allowing for unobserved heterogeneity among centers) in the propensity-score matched sample. The high-gradient group was the reference for the estimates.
A bilateral P value ≤ .05 was considered statistically significant for all estimates. All analyses were performed with STATA v.16 (StataCorp, United States).
RESULTSA total of 5084 patienbts underwent isolated SAVR during the study period. Mean age was 59.3±4.3 years and 1618 (31.8%) were women. Baseline characteristics are described in table 1. In all, 152 (2.99%) patients died during the postoperative period with a logistic EuroSCORE of 3.1±7.5. Mean follow-up of the censored observations was 105.2±54.3 months. No patient was lost to follow-up.
Unmatched baseline characteristics of patients undergoing surgery due to high-gradient SAS with preserved LVEF and low-gradient SAS with preserved LVEF
| Variable | High gradient with preserved LVEFn=3984 | Low gradient with preserved LVEFn=413 | P | Standardized difference |
|---|---|---|---|---|
| Age, y | 59.4±4.3 | 59.2±4.5 | .44 | −0.04 |
| Women | 1343 (33.7) | 169 (40.9) | .004 | 0.15 |
| Hypertension | 2404 (60.3) | 272 (65.9) | .03 | 0.11 |
| Dyslipidemia | 1983 (49.8) | 224 (54.2) | .08 | 0.09 |
| Body mass index, kg/m2 | 29.1±6.8 | 29.2±11.3 | .92 | 0 |
| Diabetes | 963 (24.2) | 80 (19.4) | .03 | −0.11 |
| Extracardiac arteriopathy | 204 (5.1) | 42 (10.2) | <.001 | 0.19 |
| Chronic pulmonary disease | 460 (11.6) | 52 (12.6) | .52 | 0.03 |
| Previous stroke | 172 (4.3) | 22 (5.3) | .32 | 0.05 |
| Previous myocardial infarction | 196 (4.9) | 26 (6.3) | .24 | 0.06 |
| Renal impairment (creatinine clearance <85mL/min) | 304 (7.6) | 23 (5.6) | .14 | −0.08 |
| History of smoking | 646 (16.2) | 68 (16.5) | .89 | 0.01 |
| History of alcoholism | 240 (6) | 20 (4.8) | .38 | −0.05 |
| Previous atrial fibrillation | 277 (7) | 36 (8.7) | .19 | 0.07 |
| Left ventricular ejection fraction, % | 62.4±7.1 | 61.8±7.3 | .06 | −0.1 |
| Biological prosthesis | 733 (18.4) | 80 (19.4) | .64 | 0.02 |
LVEF, left ventricular ejection fraction; SAS, severe aortic stenosis.
The data are expressed as No. (%) or mean±standard deviation.
Of the 5084 patients, 413 (8.1%) patients underwent SAVR due to low-gradient SAS with preserved LVEF during the study period. Mean age was 59.2±4.5 years and 169 (40.9%) were women. Baseline characteristics are presented in table 1. Ten (2.4%) patients died during the postoperative period.
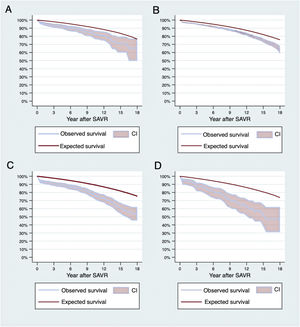
Observed survival at 1, 5, 10, 15 and 18 years was 96.4% (95%CI, 94-97.8), 91.4% (95%CI, 88.1-93.8), 83.6% (95%CI, 78.3-87.7), 71% (95%CI, 60.1-79.5), and 65.3% (95%CI, 49.7-77.3). Expected survival at 1, 5, 10, 15 and 18 years was 99.3%, 96.2%, 90.9%, 83.6%, and 76.5%. Figure 1A shows observed and expected survival curves. At 18 years, the cumulative incidence of death due to the disease was 13.6%.
Observed and expected survival curves. Expected survival was calculated by matching by age, sex and year. A: group with low-gradient SAS with preserved LVEF. B: group with high-gradient SAS with preserved LVEF. C: groups with high-gradient SAS with reduced LVEF. D: patients with low-gradient SAS with reduced LVEF. CI, cumulative incidence; LVEF, left ventricular ejection fraction; SAS, severe aortic stenosis; SAVR, surgical aortic valve replacement.
Of the 5084 patients, 3984 (78.4%) were patients who underwent surgery due to high-gradient SAS with preserved LVEF. Mean age was 59.4 years±4.3 and 1343 (33.7%) were women. A total of 102 (2.6%) patients died during the postoperative period. Table 1 shows baseline characteristics. Observed survival at 1, 5, 10, 15 and 18 years was 96.8% (95%CI, 96.2-97.3), 93% (95%CI, 92.1-93.8), 86.6% (95%CI, 85.3-87.8), 75% (95%CI, 72.7- 77,2), and 63.5% (95%CI, 58.8-67.8). Expected survival at 1, 5, 10, 15 and 18 years was 99.2%, 95.9%, 90.2%, 82.1%, and 75.7%. Figure 1B shows observed and expected survival curves for this group. At 18 years, the cumulative incidence of death due to the disease was 13.8%.
A total of 528 (10.4%) patients underwent surgery due to high-gradient aortic stenosis with low LVEF. Mean age was 58.8 years±4.4 and 83 (15.7%) were women. Thirty (5.7%) patients died during the postoperative period. Observed survival at 1, 5, 10, 15 and 18 years was 93.6% (95%CI, 91.9-95.4), 89% (95%CI, 86-91.4), 78.3% (95%CI, 73.6-82.2), 60.9% (95%CI, 53.7-67.3), and 54.2% (95%CI, 45.5-62.1). Expected survival at 1, 5, 10, 15 and 18 years was 99.3%, 95.7%, 89.8%, 81.8%, and 75.4%. Figure 1C shows observed and expected survival curves in this group. At 18 years, the cumulative incidence of death due to the disease was 25.4%.
A total of 159 (3.1%) patients underwent SAVR due to low-gradient SAS with low LVEF. Mean age was 59.6 years±3.8 and 23 (14.5%) were women. Ten (6.3%) patients died during the postoperative period. Observed survival at 1, 5, 10, 15 and 18 years was 94.3% (95%CI 89.4-97), 83.8% (95%CI, 76.8-88.9), 69.5% (95%CI, 59.5-77.5), 52.6% (95%CI, 38.1-65), and 47.4% (95%CI, 31.1-62). Expected survival at 1, 5, 10, 15 and 18 years was 99.2%, 95.4%, 89.2%, 80.7%, and 73.7%). Figure 1D shows observed and expected survival curves. At 18 years, the cumulative incidence of death due to the disease was 32.8%.
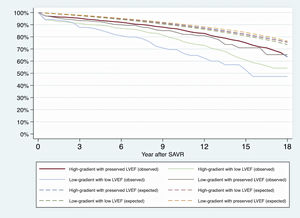
Figure 2 shows observed and expected survival curves for all types of SAS.
Survival of low-gradient SAS with preserved LVEF vs high gradient with preserved LVEFBefore matching, the group with low-gradient and preserved LVEF had a higher percentage of women, hypertension and peripheral artery disease. However, this group had less LVEF and diabetes (table 1).
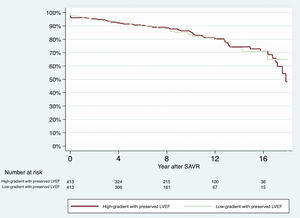
After matching, both groups were well balanced in all baseline characteristics (table 2 and ). Survival curves were similar with a log-rank test P=.95 and a HR=1 (95%CI, 0.7–1.4; P=.95) (figure 3).
Matched baseline characteristics of patients who underwent surgery due to high-gradient SAS with preserved LVEF and low-gradient SAS with preserved LVEF
| Variable | High gradient with preserved LVEFn=413 | Low gradient with preserved LVEFn=413 | P | Standardized difference |
|---|---|---|---|---|
| Age, y | 59.2±4.4 | 59.2±4.5 | .83 | 0.01 |
| Women | 165 (39.9) | 169 (40.9) | .83 | 0.02 |
| Hypertension | 262 (63.4) | 272 (65.9) | .51 | 0.05 |
| Dyslipidemia | 220 (53.3) | 224 (54.2) | .83 | 0.02 |
| Body mass index, kg/m2 | 29.2±4.5 | 29.2±11.3 | .8 | 0.02 |
| Diabetes | 76 (18.4) | 80 (19.4) | .79 | 0.02 |
| Extracardiac arteriopathy | 39 (9.4) | 42 (10.2) | .82 | 0.03 |
| Chronic pulmonary disease | 48 (11.6) | 52 (12.6) | .75 | 0.03 |
| Previous stroke | 20 (4.8) | 22 (5.3) | .87 | 0.02 |
| Previous myocardial infarction | 25 (6.1) | 26 (6.3) | 1 | 0.01 |
| Renal impairment (creatinine clearance <85mL/min) | 14 (3.4) | 23 (5.6) | .18 | 0.09 |
| History of smoking | 646 (16.2) | 68 (16.5) | .89 | 0.03 |
| History of alcoholism | 240 (6) | 20 (4.8) | .38 | −0.04 |
| Previous atrial fibrillation | 38 (9.2) | 36 (8.7) | .9 | −0.02 |
| Left ventricular ejection fraction, | 61.8±6.6 | 61.8±7.3 | .98 | 0 |
| Biological prosthesis | 89 (21.6) | 80 (19.4) | .49 | −0.05 |
LVEF, left ventricular ejection fraction; SAS, severe aortic stenosis.
The data are expressed as No. () or mean±standard deviation.
Survival curves of patients with low-gradient SAS with preserved LVEF and those with high-gradient SAS with preserved LVEF after the PSM. LVEF, left ventricular ejection fraction; PSM, propensity score matching; SAS, severe aortic stenosis; SAVR, surgical aortic valve replacement.
Data cannot be freely available. The authors are responsible for guaranteeing the anonymity of the data. They could be shared for the editors to test the analysis under reasonable request.
The sensitivity analysis controlling for the heterogeneity of centers showed a HR=0.88 (95%CI, 0.61-1.28), P=.50.
DISCUSSIONIn this study, based on a real-world setting, we found that patients who underwent surgery due to low-gradient SAS with preserved LVEF had the same life expectancy as those with high-gradient SAS with preserved LVEF. Compared with the general population of the same age, sex and year, patients with all types of SAS who underwent surgery had a loss of life expectancy. However, the loss was higher in patients with reduced LVEF and lower in patients with preserved LVEF, regardless of transvalvular gradients.
Some recent studies have shown a loss of life expectancy in patients with SAS undergoing SAVR, especially in young individuals.1,2 In our study, we confirm this finding for all types of SAS, but the cumulative incidence of death due to the disease was almost 3 times higher in patients with low-gradient and low LVEF than in those classified as low-gradient SAS and preserved LVEF. Reduced LVEF is a well-known risk factor for short- and long-term mortality after cardiac surgery10 and thus we decided to separate those patients with high-gradient and preserved LVEF from those with high-gradient and reduced LVEF. The survival curves show that, in those patients in whom the left ventricle, despite being dysfunctional, can raise gradients, the loss of life expectancy was lower than in those in whom it is no longer able to raise them.
The most important finding of our work is that patients classified as having low-gradient SAS with preserved LVEF (paradoxical SAS) by the referral cardiologists who underwent surgery had the same life expectancy as those with high-gradient SAS with preserved LVEF (figure 4). These findings are consistent with a recent meta-analysis revealing a substantial survival benefit in patients with low-gradient SAS and preserved LVEF (with low flow and with normal flow) who underwent surgery.4 This meta-analysis, however, showed high levels of heterogeneity and the authors encouraged other researchers to conduct a large observational study to obtain clearer results.
Central illustration. All aortic valve replacements in 27 Spanish centers during an 18-year period were included. The life expectancy of patients with paradoxical aortic stenosis was compared with that of patients with other types of aortic stenosis. The benefit was similar to those with high-gradient aortic stenosis. LVEF, left ventricular ejection fraction; PSM, propensity score matching; SAS, severe aortic stenosis; SAVR, surgical aortic valve replacement.
Our findings are also consistent with other small studies (around 180 patients with paradoxical SAS) showing that SAVR has a benefit on both low-gradient SAS with preserved LVEF and high-gradient SAS with preserved LVEF.5,6 However, other even smaller studies have observed that, compared with conservative treatment, SAVR had no benefit on survival in patients with paradoxical SAS.7–9 With 8% of more than 5000 patients, we report the study with the largest sample size (n=413) and the longest follow-up (more than 100 months) of patients with paradoxical SAS undergoing SAVR. In our sample, the paradoxical group had more women and hypertension than the group with high-gradient SAS, which is consistent with the pathophysiology of the low-gradient SAS with preserved LVEF.18 Our results support the finding that SAVR in these patients has the same benefit as in patients with high-gradient SAS with preserved LVEF. Clavel et al.5 showed that patients with paradoxical SAS have, compared with those with high-gradient and preserved LVEF, almost twice the risk of dying in the first year after diagnosis. Therefore, SAVR should be indicated and performed as soon as possible in these patients.
LimitationsThe main limitation of this study is that the valve area and stroke volume index were not collected in the database. Therefore, some patients with moderate aortic stenosis could have been included in the group with low-gradient SAS and preserved LVEF. These are real-world data based on a registry. Therefore, echocardiographic errors cannot be ruled out. Our sample was composed of patients aged between 50 and 65 years. The rate of biscuspid aortic valve is unknown since this variable was not registered in the database. This could be important when trying to extrapolate these results.
CONCLUSIONSYoung patients with all types of SAS undergoing SAVR have a loss of life expectancy. This loss is higher in patients with low-gradient and reduced LVEF. Patients diagnosed as having low-gradient SAS but preserved LVEF and high-gradient with preserved LVEF have a lower loss of life expectancy. The benefit of surgery is similar between these last 2 groups.
FUNDINGThere was no source of funding.
AUTHORS’ CONTRIBUTIONSAll authors meet the following 4 requirements: a) contributed substantially to the conception and design, acquisition of data, or its analysis and interpretation; b) wrote the article or critically reviewed its intellectual content; c) gave final approval to the version to be published; d) agreed to take responsibility for all aspects of the article and to investigate and resolve any issues related to the accuracy and veracity of any part of the work.
D. Hernández-Vaquero and E. Rodríguez-Caulo contributed equally to this study.
CONFLICTS OF INTERESTThere is no conflict of interest.
- -
Compared with the general population, there is a loss of life expectancy among young patients undergoing aortic valve replacement due to severe stenosis. Paradoxical aortic stenosis is a rare indication for valve replacement and its prognosis is unknown.
- -
There is a loss of life expectancy in patients with all types of aortic stenosis undergoing valve replacement. This loss is higher in patients with left ventricular dysfunction and lower in patients classified as low-gradient (paradoxical) or high-gradient aortic stenosis with preserved left ventricular ejection fraction. The benefit of surgery is similar between these last 2 groups.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2022.05.009