The role of high-density lipoproteins in the context of acute chest pain has not been well characterized. The objective of this study was to determine the relative contribution of lipid profile to the risk of acute coronary syndrome in patients admitted to a cardiology ward for chest pain.
MethodsWe included all consecutive admissions in a single cardiology department over a period of 10 months and 1-year follow-up was performed.
ResultsIn total, 959 patients were included: 457 (47.7%) were diagnosed with non-ischemic chest pain, 355 (37%) with non-ST-elevation acute coronary syndrome, and 147 (15.3%) with ST-elevation acute coronary syndrome. Prevalence of high-density lipoproteins <40mg/dL was 54.6%, and was higher in patients with acute coronary syndrome (69.4% vs 30.6%; P<.01). The prevalence of acute coronary syndrome increased with reductions in mean high-density lipoproteins. Age, active smoking, diabetes, fasting glucose >100mg/dL, and high-density lipoproteins <40mg/dL were independently associated with acute coronary syndrome, and low high-density lipoproteins was the main associated factor (odds ratio, 4.11; 95% confidence interval, 2.87-5.96). Survival analysis determined that, compared with non-ischemic chest pain, the presence of acute coronary syndrome was associated with significantly greater risk of all-cause and cardiovascular mortality.
ConclusionsLow levels of high-density lipoproteins cholesterol (≤40mg/dL) were independently associated with a diagnosis of acute coronary syndrome in patients hospitalized for chest pain, with an inverse relationship between lower levels of high-density lipoproteins and prevalence of acute coronary syndrome.
Keywords
.
IntroductionIn clinical registries of ischemic heart disease, dyslipidemia is considered to be one of the most prevalent risk factors, affecting 30% to 50% of patients.1, 2, 3, 4 Spain has one of the lowest incidences of coronary artery disease and coronary death in Europe.5, 6 Consequently, the factors that promote and protect against coronary artery disease in the Spanish population are an important topic of research. Chest pain is the characteristic symptom of ischemic heart disease and one of the most common presenting complaints in the emergency department; a series of tests are usually required to diagnose or rule out coronary artery disease and stratify subsequent risk.2, 7, 8 Furthermore, ruling out the presence of acute myocardial ischemia has clear implications, since patients with nonischemic chest pain (NICP) have a much better cardiovascular prognosis.1, 2, 9
The close relationship between dyslipidemia and ischemic heart disease has been demonstrated in studies of both the pathophysiology of the disease and its epidemiology.10, 11, 12 Plasma concentrations of low-density lipoprotein (LDL) and high-density lipoprotein (HDL) have opposing effects on the initiation, progression, and destabilization of atherosclerotic plaques, such that an imbalance in favor of LDL promotes the development of atherosclerosis, whereas HDL acts as a protective factor.13, 14 Prospective randomized studies with statins and observational registries have demonstrated a direct relationship between the concentrations of LDL and the risk of coronary artery disease, as well as a relationship between the concentrations achieved with treatment and the recurrence of coronary events.15, 16 However, some studies have revealed that the concentrations of HDL can modify the effect of LDL on the incidence of cardiovascular disease even at low LDL concentrations; thus, the absence of protective factors such as HDL, even in the absence of risk factors, can play a fundamental role in acute coronary syndrome (ACS),10, 16 and this has increased interest in the prognostic value of HDL and also in HDL as a potential therapeutic target.
Recent observational studies have found a high prevalence of low concentrations of HDL cholesterol (HDL-C) in populations with a different lipid profile, such as in the Mediterranean,17 and subanalyses of some registries have revealed a prognostic role for the different lipoproteins.18, 19, 20 Nevertheless, the association with acute ischemia in the context of chest pain, comparing patients with ACS with patients who were finally diagnosed with NICP, has not been extensively analyzed, and studies undertaken in emergency departments have not succeeded in demonstrating the usefulness of apolipoproteins for the discrimination of ischemia.21
The aim of this study was to assess the relative contribution of lipid profile to the risk of ACS in patients admitted to a cardiology ward for chest pain.
Methods Study DesignA prospective observational study was undertaken of patients admitted to a single cardiology ward with suspected coronary chest pain after visiting the emergency department. All unscheduled admissions were consecutively enrolled in the study over a 10-month period (December 1, 2008 to April 30, 2010). The emergency department of our hospital has neither a specific care program for patients with chest pain nor an on-call cardiologist, and the decision to admit patients to the cardiology ward was therefore made by the emergency department. The 1-year follow-up involved review of patient histories, including electronic records held by emergency departments and by primary care services (via the ABUCASIS program), and also telephone contact to ensure adequate follow-up of all patients for at least 1 year. The study included 2 analyses: a cross-sectional analysis of the role of lipid profile, specifically HDL-C, in patients admitted to the cardiology ward for chest pain and a second, prospective analysis involving follow-up of those patients to confirm the diagnosis and prognosis after 1 year.
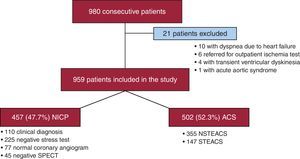
In total, 980 consecutive patients were initially included in the study. We excluded 21 patients for clearly different clinical presentations (10 reported dyspnea and were diagnosed with heart failure; 4 patients were diagnosed with transient ventricular dyskinesia; 6 patients were discharged with an outpatient referral for an ischemia test; and 1 patient had acute aortic syndrome). The final sample therefore comprised 959 patients.
The following criteria defined ACS: elevated serum levels of enzymes that act as markers of myocardial damage above the lower limits for our laboratory (troponin I, ≥0.04 ng/dL) and/or abnormalities in the electrocardiogram (ECG) indicative of a lesion or myocardial ischemia accompanied by chest pain and/or positive results in the ischemia test (stress test or cardiac single-photon emission tomography [SPECT]). Diagnosis of ACS included acute myocardial infarction with or without ST-segment elevation and unstable angina. Patients without enzyme and ECG abnormalities and who had a negative ischemia test were discharged with a diagnosis of NICP. Data were recorded on primary diagnosis, prior history, cardiovascular risk factors, treatments, additional tests performed, and thrombotic or hemorrhagic complications during the period of admission. The registry was approved by the institutional review board of our hospital.
Definition of VariablesAnalysis of the lipid profile was carried out using a sample of blood obtained under fasting conditions during the first 24 to 72h of hospital admission for each patient. The HDL-C concentrations were classified according to the cutoff of ≤40mg/dL indicated in the National Cholesterol Education Program III criteria22; likewise, LDL cholesterol (LDL-C) concentrations were considered elevated if they were greater than 130mg/dL.22 Glomerular filtration rate (GFR) was estimated from the serum concentrations of creatinine according to the Modification of Diet in Renal Disease Study equation.23 Patients were considered to have a history of diabetes mellitus, dyslipidemia, or hypertension when they were receiving specific treatment for the condition or reported prior diagnosis.
Statistical AnalysisQualitative variables were evaluated using the χ2 test and the Fisher exact test when necessary; quantitative variables were compared by t test and analysis of variance. Multivariate analysis of the characteristics associated with ACS versus NICP was carried out by binary logistic regression, with ACS as the dependent variable and variables that were statistically significant in the univariate analysis and that could have plausible clinical and/or etiological relevance introduced as independent variables. Regression models and their analysis were carried out according to current guidelines24; possible first-level interactions among the variables included in the model were analyzed, and those for which statistical significance was observed were included in the logistic regression model. The calibration of the logistic regression model was carried out using the Hosmer-Lemeshow statistic. Survival during follow-up was assessed by Cox proportional hazard regression analysis, using a backward stepwise inclusion method in which age, sex, all risk factors, any prior cardiovascular disease, treatment at discharge, and coronary revascularization were included. Statistical analysis was carried out using SPSS 15.0 (SPSS Inc., Chicago, Illinois, United States). Values of P<.05 were considered to be statistically significant.
ResultsOf the 959 patients included in the study, 457 (47.7%) were diagnosed with NICP and 502 (52.3%) with ACS, which corresponded to ACS with ST-segment elevation in 29.3% (Figure 1); patients diagnosed with unstable angina were included in the group with ACS (10.2%). In the group diagnosed with NICP, ischemia was ruled out based on the clinical judgement of the attending physician in 100 cases, by stress test in 225 cases, by coronary angiography showing normal coronary arteries in 77 cases, and by SPECT in 45 cases. Compared with patients who had a diagnosis of ACS, patients with NICP were younger and had a lower prevalence of male sex, smoking, diabetes mellitus, and history of ischemic heart disease; in contrast, patients with NICP had a higher body mass index and more frequent history of atrial fibrillation (Table 1). Patients with NICP were also more frequently treated with fibrates, but there were no differences in the frequency of treatment with statins or antiplatelet drugs. The results of biochemical analyses are shown in Table 2. Patients with NICP had lower fasting glucose levels, creatinine, and GFR but higher concentrations of total cholesterol, HDL-C, and hemoglobin.
Figure 1. Flow diagram of patient inclusion in the study. ACS, acute coronary syndrome; NICP, nonischemic chest pain; NSTEACS, non-ST-elevation ACS; SPECT, single photon emission computed tomography; STEACS, ST-elevation ACS.
Table 1. Patient Characteristics According to Diagnosis.
| Total | Nonischemic pain | ACS | P | |
| Patients, n (%) | 959 | 457 (47.7) | 502 (52.3) | |
| Men, % | 65 | 57.1 | 72.3 | <.01 |
| Age, y | 67.7±13.1 | 65.5±13.3 | 69.7±12.5 | <.01 |
| BMI | 27.9±4.6 | 28.8±4.2 | 27.4±4.8 | .02 |
| Diabetes mellitus, % | 33.2 | 23.6 | 41.8 | <.01 |
| Hypertension, % | 68.5 | 65.9 | 70.9 | .09 |
| Dyslipidemia, % | 49.8 | 45.3 | 54 | .01 |
| Smokers, % | 23.8 | 19.7 | 27.5 | .01 |
| Prior ischemic heart disease, % | 32.6 | 27.8 | 37.1 | .01 |
| Prior heart failure, % | 4.2 | 4.2 | 4.2 | .98 |
| Prior CVA, % | 6.2 | 5.7 | 6.6 | .57 |
| Atrial fibrillation, % | 10.5 | 12.7 | 8.6 | .02 |
| Intermittent claudication, % | 4.9 | 1.5 | 8 | <.01 |
| COPD, % | 9.5 | 9.6 | 9.4 | 0.89 |
| Family history of IHD, % | 8.2 | 7.2 | 9.2 | 0.27 |
| Treatment with statins, % | 28.3 | 28.6 | 28.1 | .86 |
| Treatment with aspirin, % | 27.2 | 27.9 | 26.5 | .62 |
| Treatment with fibrates, % | 2.9 | 4.4 | 1.6 | .01 |
ACS, acute coronary syndrome; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; IHD, ischemic heart disease.
Continuous variables are shown as mean±standard deviation and discrete variables as percentages.
Table 2. Results of Biochemical Analyses According to Diagnosis.
| Total | Nonischemic pain | ACS | P | |
| Fasting glucose, mg/dL | 111.6±38.5 | 105.1±32.7 | 117.8±42.4 | <.01 |
| Total cholesterol, mg/dL | 170.7±102 | 179.9±118.2 | 162.2±83.6 | <.01 |
| HDL, mg/dL | 40.1±13.4 | 44.5±14.6 | 36.1±10.7 | <.01 |
| LDL, mg/dL | 98.5±50.2 | 100.3±35.6 | 96.8±60.4 | .29 |
| Triglycerides, mg/dL | 125 [95-167] | 124 [92-167.5] | 126 [97-166] | .61 |
| Creatinine, mg/dL | 1±0.4 | 0.9±0.3 | 1.1±0.5 | <.01 |
| GFR, mL/min/1.73 cm2 | 76.8±25.4 | 80±25.7 | 74±24.9 | <.01 |
| Hemoglobin, mg/dL | 13.2±1.9 | 13.4±1.8 | 13±2 | <.01 |
| HbA1c, % (in diabetics) | 7.7±1.4 | 7.5±1.4 | 7.9±1.4 | .07 |
ACS, acute coronary syndrome; GFR, glomerular filtration rate; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Results are shown as mean±standard deviation, except for triglycerides, which are shown as median [interquartile range] as the values did not obey a normal distribution.
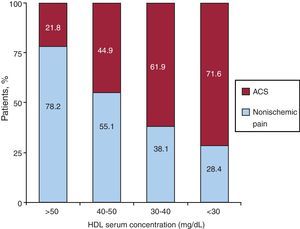
Overall, HDL-C concentrations of less than 40mg/dL were found in 54.6% of patients, and the prevalence of low HDL-C was higher in patients with ACS (69.4% vs 30.6%, P<.01). Furthermore, when HDL-C concentrations were stratified, the prevalence of ACS was much higher in patients with lower mean HDL concentrations (Figure 2). There was a positive relationship between HDL-C <40mg/dL and diabetes mellitus (P=.02), prior ischemic heart disease (P=.02), and treatment with fibrates (P<.01), which was taken into account when introducing variables into the logistic regression model used to identify variables independently associated with ACS vs NICP. This multivariate analysis was adjusted for age, sex, hypertension, diabetes mellitus, dyslipidemia, prior ischemic heart disease, and use of fibrates, and it was found that age, smoking, diabetes mellitus, fasting glucose >100mg/dL, and HDL-C <40mg/dL (which showed the strongest association) were independently associated with ACS (Table 3). The model was correctly calibrated (P=.25 in the Hosmer-Lemeshow test).
Figure 2. Relationship between high-density lipoprotein concentration and acute coronary syndrome. ACS, acute coronary syndrome; HDL, high-density lipoprotein.
Table 3. Variables Independently Associated With the Presence of Acute Coronary Syndrome in the Multivariate Model.
| Variables | OR | 95%CI | P |
| Female sex | 0.47 | 0.34-0.68 | <.01 |
| Atrial fibrillation | 0.50 | 0.30-0.84 | <.01 |
| Age | 1.05 | 1.03-1.06 | <.01 |
| Smoking | 2.50 | 1.62-3.84 | <.01 |
| Diabetes mellitus | 1.87 | 1.10-2.59 | .02 |
| Serum glucose >100 mg/dL | 3.35 | 1.74-6.77 | <.01 |
| HDL <40 mg/dL | 4.11 | 2.87-5.96 | <.01 |
95%CI, 95% confidence interval; HDL, high-density lipoprotein; OR, odds ratio.
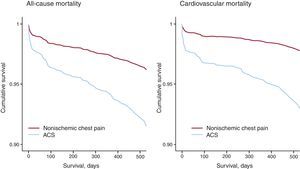
During the period of hospital admission, 21 patients died. All of those patients had ACS (4.6%), 8 with ST-segment elevation (5.4%), and 13 (3.7%) with non-ST-segment elevation (P=.37). To assess whether patients had been correctly classified as having NICP or ACS, the prognosis was assessed after 1 year. Of the 938 patients who were discharged from hospital, complete follow-up was obtained in 97.5% of cases, with a mean follow-up period of 415.3±107.5 days (median [interquartile range], 420 [361-461] days). All-cause mortality was greater in patients with ACS than in those with NICP (12.9% vs 3.8%; P<.01), as was cardiovascular mortality (10% vs 2%; P<.01). Assessment of survival by Cox proportional hazard regression analysis adjusted for age, sex, risk factors, and treatments at discharge showed that the presence of ACS was associated with a significantly higher risk of all-cause mortality (hazard ratio [HR], 2.26; 95% confidence interval [95%CI], 1.13-3.95; P<.01) and cardiovascular mortality (HR, 3.22; 95%CI, 1.55-6.71; P<.01) (Figure 3).
Figure 3. Cox regression curves for death during follow-up at 1 year. ACS, acute coronary syndrome.
DiscussionThe principal finding of this study is that patients with ACS have lower plasma concentrations of HDL-C; these low values are independently associated with the presence of ACS, and the frequency of ACS is greater at lower plasma concentrations of HDL-C. The results of our study showed that HDL-C concentrations of less than 40mg/dL are one of the principal factors associated with ACS in patients with chest pain. The characteristics of our study population were similar to those of other registries of ischemic heart disease and observational studies undertaken in chest pain units.1, 2, 3, 4, 7 We can therefore conclude that the sample is comparable and yields valid results that are applicable to similar populations. One of the strengths of our study is that it includes a control group of patients with NICP, in whom the presence of myocardial ischemia was ruled out and prognosis was subsequently verified at 1-year follow-up.
Clinical practice guidelines have defined a value below which plasma levels of HDL are considered low,22 but the relationship between these values and clinical events has not been extensively studied, particularly in the Spanish population, which has historically been associated with a different risk profile. Since cardiovascular risk usually displays an inverse linear relationship with HDL-C concentration, we analyzed the prevalence of ACS as a function of this variable and obtained a distribution that was highly indicative of an increased risk of ACS at lower concentrations of HDL-C. Control of plasma concentrations of LDL cholesterol (LDL-C) is considered to be the main objective of treatment for dyslipidemia, but definitive recommendations on the treatment and risk stratification of patients with low plasma HDL-C have not been provided in current guidelines.25, 26 Our study revealed that low HDL-C concentrations are strongly associated with the presence of acute ischemic heart disease, and this could have important implications for risk stratification in patients with chest pain, since those in whom acute myocardial ischemia is ruled out, as in our study, have a much better prognosis.
We also identified a significant interaction between HDL-C concentrations greater than 40mg/dL and the presence of diabetes mellitus, ischemic heart disease, or treatment with fibrates for the association with final diagnosis of ACS. In addition to showing that the identified variables act as confounding factors, this observation is also consistent with current evidence, since it is well known that the insulin resistance associated with diabetes mellitus is one of the principal mechanisms implicated in lower HDL concentration27 and that patients with chronic ischemic heart disease tend to have significantly lower serum HDL-C concentrations.12, 28 In our opinion, the negative association observed between atrial fibrillation and ACS is consistent both with the overall study results and with day-to-day clinical practice. Chest pain due to rapid ventricular response (paroxysmal or associated with atrial fibrillation) can lead to hospital admission and can even be initially confused with ACS.
The most recent evidence has linked low plasma concentrations of HDL-C with accelerated progression of subclinical atherosclerotic lesions and the subsequent occurrence of clinical events. This process would be mediated by endothelial dysfunction, reduced reverse transport of cholesterol, increased oxidation of LDL, and inflammation of vessel walls.13, 14, 29, 30, 31 In addition to the evidence of a protective role for HDL obtained from epidemiological studies, the Framingham study found HDL-C to be a stronger risk factor than plasma LDL-C, total cholesterol, or triglycerides for coronary heart disease.32 Studies undertaken with vascular ultrasound have also demonstrated that regression of atheromatous plaques does not only depend on a maximal reduction of LDL-C concentrations but also on an increase in the HDL-C concentration, along with other factors such as the absence of diabetes or hypertension.10, 33 On the other hand, the concentrations of lipoproteins can change in the first 24h of ACS, and it is conceivable that the reduction in HDL-C could be a consequence of the condition; nevertheless, it has recently been shown that the magnitude of these changes in HDL-C concentrations would be extremely small.34 Whatever the case may be, HDL-C cholesterol remains strongly associated with ischemia.
In terms of the clinical importance of HDL-C for cardiovascular disease prevention and treatment of dyslipidemia, the strategies that are most effective in increasing HDL-C concentration are smoking cessation, weight reduction, and regular exercise.27, 35 On the other hand, statins, the most common lipid-lowering drugs in clinical practice, are very effective at reducing LDL concentrations but have little or no effect on plasma concentrations of this lipid fraction36 and could have a modulatory effect on the anti-inflammatory and proinflammatory properties of HDL.29, 37 Future perspectives for treatment include drugs that both increase HDL concentration and augment its functionality.35, 38
One of the limitations of our study is a possible selection bias, since it is an observational registry undertaken in a single hospital that included patients admitted to a single cardiology ward. As a result it does not include patients who visited the emergency department for chest pain and were discharged nor those patients who may have been admitted to other departments (internal medicine, respiratory medicine, etc.). Furthermore, the sample size included in this study is slightly lower than that in other studies of chest pain.7, 8, 31 Nevertheless, our study offers the advantages of a more accurate biochemical characterization of the patients and also follow-up data at 1 year.
In terms of the collection period for blood samples (24-72h), although it is true that variations in the concentrations of lipoproteins have been detected in the first few hours of ACS, those data come from studies involving small samples. The clinical relevance of this variability has been questioned on the basis of other studies with larger populations and samples extracted between the time of admission and up to 4 days after ACS.34 Although the variation is slightly significant, the demonstrated benefits of early initiation of statin treatment in these patients suggest that the lipid profile can and should be obtained reliably in the first available sample of blood, avoiding delay of up to 1 month after discharge for the selection of the most appropriate treatment for dyslipidemia.
Another possible limitation is linked to the analysis of plasma HDL-C concentrations and not of Apo-A particles, which have been postulated to be better predictors.11 Nevertheless, tests for ApoE particles are not as widely available as standard analysis of lipid fractions and the cut-off points have not been well defined.
ConclusionsIn an unselected group of patients admitted to a cardiology ward for chest pain, low HDL-C concentration (≤40mg/dL) was independently associated with a diagnosis of ACS. The concentrations of HDL-C are inversely associated with a diagnosis of acute ischemic heart disease in this subgroup of patients, such that lower levels of HDL are linked to higher frequencies of acute ischemic disease. The possible diagnostic and prognostic implications of this finding should be analyzed in future studies.
Conflicts of interestNone declared.
Received 24 February 2011
Accepted 26 July 2011
Corresponding author: Departamento de Cardiología, Hospital Universitario de San Juan, Carretera Valencia-Alicante s/n, 03550 San Juan de Alicante, Alicante, Spain. acorderofort@gmail.com