To the Editor:
Ventricular arrhythmia is normally secondary to organic heart disease or ion disorders. On rare occasions, it may also be caused by extracardiac diseases, such as hyperthyroidism.
We describe a 46-year-old woman who consulted for dyspnea, cough, and edema that had lasted three weeks. She reported no other symptoms and had not lost weight. Soon after her arrival, she presented cardiorespiratory arrest caused by ventricular fibrillation, but recovered with electric defibrillation.
The subsequent physical examination showed a patient with anxiety and slight fine tremor in both hands. She presented dyspnea at rest, crepitant rales in both bases, jugular vein enlargement, and edema in the legs. Blood pressure was 155/64 mm Hg. Auscultation revealed a systolic murmur in the mitral area and gallop rhythm in the third sound. The electrocardiogram basically showed sinus rhythm of 100 bpm, normal QRS complex, and QTC interval of 0.44 s. The chest x-ray disclosed cardiomegaly and bilateral interstitial pattern indicative of edema. The general blood tests were normal (potassium, 3.8 mmol/L; magnesium, 1.8 mg/dL). The echocardiogram showed left ventricle neither dilated nor hypertrophied, with global hypokinesia (ejection fraction, 35%), and mild to moderate mitral insufficiency.
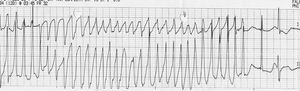
In the first 7 hours of hospitalization, she presented repeated runs of polymorphic ventricular tachycardia in torsade de pointes (Figure 1) that partially remitted with magnesium sulfate and virtually disappeared after initiating atenolol therapy at 72 h post-admission. Cardiac catheterization did not show any coronary lesions or vasospasm. The thyroid hormone study revealed the following: T3 of 733.1 ng/dL (normal value, 60-181 ng/dL), T4 of 20.2 µmg/dL (normal value, 4.5-10.9 µg/dL), free T4 of 5.3 ng/dL (normal value, 0.8-1.8 ng/dL), thyroid-stimulating hormone (TSH) <0.01 mU/L (normal value, 0.3-5.5 mU/L), antithyroglobulin antibodies <20.0 U/mL (normal value <40 U/mL), and antimicrosomal antibodies 2,704 U/mL (normal value <35 U/mL). Thyroid scintigraphy showed hyperfunctioning diffuse goiter. Therefore, Graves-Basedow disease was diagnosed, and carbimazole therapy was started, maintaining the atenolol therapy. The QTC interval was 0.42 s. An echocardiogram at 14 days showed an improvement in systolic function (ejection fraction, 53%) and reduced mitral regurgitation. At the end of follow-up (8 March 8, 2006), the patient was well and presented no signs of heart failure or arrhythmias.
Figure 1. Polymorphic ventricular tachycardia in torsade de pointes.
The most common clinical manifestations of thyrotoxic heart disease are heart rate disorders, in particular, sinus tachycardia and atrial fibrillation, which presents in 5%-15% of patients.1 Malignant ventricular arrhythmias, which are potentially fatal, are much more unusual.2 The onset of tachycardia or ventricular fibrillation has been reported within a thyrotoxic storm.3 The presentation of these arrhythmias in the initial phase of the disease is much less common, and only a few isolated cases are described in the scientific literature. The majority4,5 occur in the context of thyrotoxic periodic paralysis with severe hypopotassemia. There has been an occasional patient in whom the ventricular arrhythmia were related to coronary spasm.6 An interesting observation is the finding of QT interval prolongation, in both experimental work and in patients with hyperthyroidism,7 which could play an important role in the pathophysiological mechanism of ventricular tachycardia in torsade de pointes.
In short, the patient we describe is an illustration of a rare arrhythmic complication of hyperthyroidism. Ventricular dysfunction attributable to the hyperthyroidism8 and mild hypopotassemia have probably contributed to the genesis of the ventricular arrhythmia. Although exceptionally rare, hyperthyroidism should be investigated and ruled out in patients who present ventricular arrhythmia of uncertain etiology.