The results from the IMPROVE-IT trial and data from Mendelian randomization studies reinforce the causal role of low-density lipoprotein (LDL) cholesterol in atheromatous cardiovascular disease.1,2 The “lower is best” concept has robust evidence-based support, and high-intensity cholesterol-lowering strategies ought to be implemented instead of high-intensity statin therapy.3
A clinically relevant question is “What is the maximum LDL-lowering capacity that will be achieved by combination therapy after the introduction of the new proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors?”
Statins have accumulated the most scientific evidence in cardiovascular prevention. Their average cholesterol-lowering effect ranges from 30% to 50%. By adding ezetimibe, their LDL-lowering capacity increased by 20% (22% in the IMPROVE-IT trial).1 New PCSK9 inhibitors add an LDL reduction capacity of approximately 60%.4,5 It must be taken into account that these reduction percentages are average values that may vary due to individual response. In addition, these percentages are achieved from the starting LDL values. Therefore, when calculating the overall impact of drug combinations, the effect of previous drugs must be taken into account. The absolute effect of adding drugs is lower than the addition of their relative effects.
For example, in a patient with LDL levels of 200mg/dL, a high potency statin will decrease LDL cholesterol by 50% to 100mg/dL. By adding ezetimibe, we expect a 20% incremental LDL reduction; therefore, LDL concentrations of 100mg/dL will decrease to 80mg/dL (20% less). Thus, this patient will have a final reduction of 120mg/dL, which is a 60% reduction from the starting point (200mg/dL). Therefore, by adding a drug that reduces LDL by 50% and another that reduces it by 20%, we will have a final absolute reduction of 60% instead of 70%. The same principle can be applied to PCSK9 inhibitors. In this patient, we can expect an incremental LDL reduction of 60%, so the LDL cholesterol level of 80mg/dL will decrease to 32mg/dL. This is exactly an 84% reduction, 24% more from the baseline value. This is indeed the maximum LDL-lowering capacity according to available drugs.
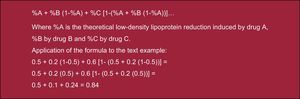
The efficacy of different drug combinations can be calculated by the formula in the Figure.
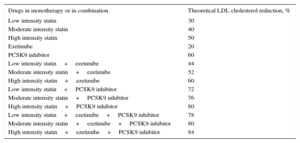
Several points should be stressed. The maximum LDL-lowering capacity obtained with a statin plus ezetimibe was 60%. The maximum LDL-lowering capacity when combining the more potent statin plus a PCSK9 inhibitor was 80%. The maximum LDL-lowering capacity using the 3 drugs in combination was 84% (Table).
Theoretical Low-density Lipoprotein Reduction in Percentage Induced by Drugs in Monotherapy or in Combination
| Drugs in monotherapy or in combination | Theoretical LDL cholesterol reduction, % |
|---|---|
| Low intensity statin | 30 |
| Moderate intensity statin | 40 |
| High intensity statin | 50 |
| Ezetimibe | 20 |
| PCSK9 inhibitor | 60 |
| Low intensity statin+ezetimibe | 44 |
| Moderate intensity statin+ezetimibe | 52 |
| High intensity statin+ezetimibe | 60 |
| Low intensity statin+PCSK9 inhibitor | 72 |
| Moderate intensity statin+PCSK9 inhibitor | 76 |
| High intensity statin+PCSK9 inhibitor | 80 |
| Low intensity statin+ezetimibe+PCSK9 inhibitor | 78 |
| Moderate intensity statin+ezetimibe+PCSK9 inhibitor | 80 |
| High intensity statin+ezetimibe+PCSK9 inhibitor | 84 |
Low, moderate and high intensity statins are defined according to Stone et al.6
LDL, low-density lipoprotein.
This theoretical exercise has implications for clinical decision-making and should also be taken into account in clinical guidelines.
For example, when statins are used as monotherapy (a maximum LDL lowering effect of 50%), only patients with LDL levels below 140mg/dL will reach secondary prevention targets (LDL<70mg/dL). With a statin plus ezetimibe (maximum LDL lowering capacity of 60%), only patients with LDL below 175mg/dL will reach secondary prevention targets.
With triple therapy (LDL lowering capacity of 84%), almost anyone with LDL levels up to 437mg/dL could achieve secondary prevention LDL targets.
It seems reasonable to adapt clinical guidelines and recommendations to clinical feasibility.
CONFLICTS OF INTERESTL. Masana receives lecture or advisory fees from Amgen, Sanofi, MSD, Kowa, Recordati, Esteve, Danone, Chiesi; Praxis. N. Plana receives lecture fees from MSD Esteve, and D. Ibarretxe receives lecture fees from MSD.