Early, high-quality cardiopulmonary resuscitation (CPR) improves survival and neurological prognosis in out-of-hospital cardiac arrest. Mechanical compression systems have been developed with the aim of achieving uninterrupted CPR, without rescuer fatigue, or for use in places where manual resuscitation is impractical.
The most widely-used at the moment are the piston system (LUCAS, Jolife; Sweden) and the distributing band system (AutoPulse, Zoll; USA). The benefit of these systems is debated,1 and there are few data on their safety. Our objective was to analyze the introduction of these mechanical systems to the medical emergency services network in our province, describing their use and associated complications.
We prospectively included all patients admitted to a cardiological intensive care unit with the diagnosis of recovered out-of-hospital cardiac arrest from January 2016, which was when mechanical compression devices were introduced.
We analyzed resuscitation times, neurological status at discharge according to the Glasgow-Pittsburgh Cerebral Performance Category (CPC) and the complications in patients who received mechanical compressions compared with those who received manual compressions.
Complications were defined as any new traumatic thoracic or abdominal lesion that could be explained as a consequence of resuscitation (bone fracture, pneumothorax, hemothorax, pneumomediastinum, pulmonary contusion, or organ laceration).
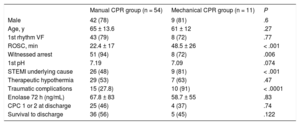
Between January 2016 and August 2017, 65 consecutive patients were identified with a diagnosis of out-of-hospital cardiac arrest; 11 (17%) received predominantly mechanical compressions when a device was available (1 with AutoPulse and 10 with LUCAS) and 54 (83%) received only manual compressions. The baseline patient characteristics and the cardiac arrest details are described in Table 1.
Patient Characteristics and Cardiac Arrest Details
| Manual CPR group (n = 54) | Mechanical CPR group (n = 11) | P | |
|---|---|---|---|
| Male | 42 (78) | 9 (81) | .6 |
| Age, y | 65 ± 13.6 | 61 ± 12 | .27 |
| 1st rhythm VF | 43 (79) | 8 (72) | .77 |
| ROSC, min | 22.4 ± 17 | 48.5 ± 26 | < .001 |
| Witnessed arrest | 51 (94) | 8 (72) | .006 |
| 1st pH | 7.19 | 7.09 | .074 |
| STEMI underlying cause | 26 (48) | 9 (81) | < .001 |
| Therapeutic hypothermia | 29 (53) | 7 (63) | .47 |
| Traumatic complications | 15 (27.8) | 10 (91) | < .0001 |
| Enolase 72 h (ng/mL) | 67.8 ± 83 | 58.7 ± 55 | .83 |
| CPC 1 or 2 at discharge | 25 (46) | 4 (37) | .74 |
| Survival to discharge | 36 (56) | 5 (45) | .122 |
CPC, Glasgow-Pittsburgh Cerebral Performance Category; CPR, cardiopulmonary resuscitation; ROSC: return of spontaneous circulation; STEMI, ST-elevation myocardial infarction; VF, ventricular fibrillation.
Values are expressed as No. (%) or mean ± standard deviation.
The time to return of return of spontaneous circulation (ROSC) in the group with mechanical compressions was significantly longer (48.3 ± 26min) than in the group with manual compressions 22.4 ± 17min; P < .001). The mechanical compression group also had a higher proportion of ST-elevation acute myocardial infarction as the cause of arrest.
The proportion of witnessed arrests was higher in the manual compression group than in the mechanical compression group.
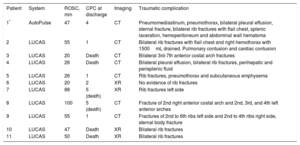
All patients had a chest X-ray and/or computed tomography of the chest and abdomen within the first few hours of admission. Traumatic lesions were significantly more common in the mechanical compression group (91% vs 27.8%; P < .001) and their complications are listed in Table 2.
Details of the Traumatic Complications in Patients Resuscitated With Mechanical Compressions
| Patient | System | ROSC, min | CPC at discharge | Imaging | Traumatic complication |
|---|---|---|---|---|---|
| 1* | AutoPulse | 47 | 4 | CT | Pneumomediastinum, pneumothorax, bilateral pleural effusion, sternal fracture, bilateral rib fractures with flail chest, splenic laceration, hemoperitoneum and abdominal wall hematoma |
| 2 | LUCAS | 55 | 1 | CT | Bilateral rib fractures with flail chest and right hemothorax with 1500mL drained. Pulmonary contusion and cardiac contusion |
| 3 | LUCAS | 20 | Death | CT | Bilateral 3rd-7th anterior costal arch fractures |
| 4 | LUCAS | 26 | Death | CT | Bilateral pleural effusion, bilateral rib fractures, perihepatic and perisplenic fluid |
| 5 | LUCAS | 26 | 1 | CT | Rib fractures, pneumothorax and subcutaneous emphysema |
| 6 | LUCAS | 20 | 2 | XR | No evidence of rib fractures |
| 7 | LUCAS | 88 | 5 (death) | XR | Rib fractures left side |
| 8 | LUCAS | 100 | 5 (death) | CT | Fracture of 2nd right anterior costal arch and 2nd, 3rd, and 4th left anterior arches |
| 9 | LUCAS | 55 | 1 | CT | Fractures of 2nd to 6th ribs left side and 2nd to 4th ribs right side, sternal body fracture |
| 10 | LUCAS | 47 | Death | XR | Bilateral rib fractures |
| 11 | LUCAS | 50 | Death | XR | Bilateral rib fractures |
CPC, Glasgow-Pittsburgh Cerebral Performance Category; CT, computed tomography; ROSC, return of spontaneous circulation; XR, X-ray.
In the manual compression group, 13 X-rays were identified with isolated rib fractures and 2 computed tomography scans with traumatic lesions: 1 patient with bilateral rib fractures and flail chest and 1 patient with rib fractures and sternal fracture.
The main finding in our study was a significantly higher proportion of traumatic complications in the group of patients who received mechanical compressions. Although most randomized trials1 do not specifically include traumatic complications, the high percentage of complications in our study is in contrast to the CIRC study,2 which contained a detailed table with the traumatic complications in which there were similar results in both groups (11% in the manual CPR group vs 12% in the mechanical CPR group).
Among the reasons that could explain the high prevalence of traumatic lesions in our study is the significantly longer time to ROSC in the group of patients who received mechanical compressions than in the manual compression group (48.3 ± 26 vs 22.4 ± 17min; P < .001). However, in a randomized study3 in which information was available on time to ROSC–which was longer in the mechanical compression group—there were no differences between the 2 types of resuscitation, and the serious complication rate was 0.003%.
A multicenter study based on the autopsies of patients who died during resuscitation4 found a traumatic complication rate of 75% in the manual compression group and 91% in the mechanical compression group. Both groups had a mean CPR time of 35minutes, slightly lower than the mechanical compression group in our series, but still a high percentage of traumatic complications. It is worth mentioning here that in our series there were several patients treated with mechanical compressions and short ROSC times who had potentially serious complications (Table 2).
Despite the descriptive nature and small sample size of our study, there were no differences in terms of survival and good neurological status at discharge between the 2 groups. These results agree with the evidence published to date: in 4 of the randomized studies1 there was no demonstrated superiority of mechanical compression systems; equivalence was demonstrated in the CIRC study.2
The advanced life support algorithm in the 2015 ERC resuscitation guidelines5 recommends the use of mechanical devices as a reasonable alternative when high-quality manual compressions are impractical or compromise the safety of the provider (transport, coronary angiography) or when prolonged CPR is necessary. In these cases, we believe that a low threshold of clinical suspicion for traumatic lesions and the systematic use of imaging to exclude them could help in the early detection of potentially serious complications.
.