Several classifications have been proposed to define the baseline characteristics of bifurcation lesions, but the most widely accepted is the Medina classification. This classification was first adopted in 2005 during the first congress held by the European Bifurcation Club in Bordeaux, France. Its success is based on its simplicity and the fact that it does not require memorization. Today, it remains the preferred reference, with new and interesting considerations added since its publication in 2006.1
THE MEDINA CLASSIFICATION IS FLEXIBLEThe original description included 7 types of bifurcations. Bifurcations are divided into 3 segments: proximal, distal main vessel (MV), and side branch (SB). Each segment is assigned a value of 0 (in the absence of significant stenosis) or 1 (in the presence of > 50% stenosis). Some authors have modified the original format by using the letter X (as an equivalent of 0 or 1) to group some types of bifurcation. Thus (excluding 0,0,1 lesions), true and nontrue bifurcation lesions can be defined as (X,X,1) or (X,X,0), respectively; lesions with any proximal or distal involvement of the MV as (1,X,X) or (X,1,X), bifurcations with proximal MV, and SB stenosis as 1,X,1 and so on.
THE MEDINA CLASSIFICATION IS VERSATILEAlthough the Medina classification was originally described for bifurcation lesions, it has recently been adapted for left main (LM) trifurcations.2 Thus, maintaining the same philosophy (1,0) for the presence or absence of> 50% stenosis, a fourth number is added to describe the trifurcation. The first number thus corresponds to the proximal segment (LM) and the remaining 3 numbers must be ordered according to the diameters of the distal segments. The second number thereby corresponds to the distal MV (left anterior descending artery [LAD]), the third to the largest SB and, finally, the last number to the smallest SB. Consequently, 15 different types of trifurcation lesions are possible. The modification described above can be also used for groups.
THE MEDINA CLASSIFICATION HAS PROGNOSTIC SIGNIFICANCEThe Medina classification can provide valuable information on the prognosis of patients with bifurcation lesions.3,4 In addition to the percentage of stenosis in each segment, bifurcation severity may also be graded according to the Medina type. Thus, the ranking from highest to lowest severity according to the Bif-Arc/EBC consensus2 would be as follows: (1,1,1)> (1,1,0)> (1,0,1)> (0,1,1)> (1,0,0)> (0,1,0)> (0,0,1). In the COBIS II registry,3 the patients with Medina class (1,0,1), (1,1,1), or (0,1,1), ie, true bifurcation lesions, had a significantly higher risk of major adverse cardiac events than those with nontrue bifurcation lesions. Among true bifurcation lesions, Medina (1,1,1) and (0,1,1) were associated with a higher risk of cardiac death or myocardial infarction than Medina (1,0,1). Similarly, Perl et al.4 found that in patients undergoing bifurcation percutaneous coronary intervention with second-generation drug-eluting stents, true bifurcation lesions were associated with a significantly higher rate of major adverse cardiac events at 1 and 3 years. A recent article5 showed that, in addition to Medina class (1,1,1), bifurcation type (0,0,1) was independently associated with an increased hazard of target lesion failure.
THE MEDINA CLASSIFICATION HAS ACCEPTABLE INTEROBSERVER VARIABILITYZlotnick et al.6 evaluated the interobserver variability of the Medina classification to characterize bifurcation lesions. A standardized set of freeze frame coronary angiograms was provided to interventional cardiologists from the United States and Europe, who sent their answers through an online survey. The authors found that, for most of the angiograms evaluated, there was minimal variability in lesion classification using the Medina system.
IS THE MEDINA CLASSIFICATION USEFUL TO SELECT THE TREATMENT STRATEGY?Provisional philosophy vs an upfront 2-stent technique for the treatment of bifurcation lesions is a common discussion that started many years ago and it is still a matter of debate.7 In general, it is accepted that Medina class bifurcations (1,0,0) (1,1,0) and (0,1,0) should be treated by provisional stenting.8 In contrast, in Medina class (1,1,1), (1,0,1) and (0,1,1), this treatment is more controversial. While the EBC TWO9 and the EBC MAIN10 studies supported provisional strategies in these types of bifurcations, the DKCRUSH-V study11 obtained better results in patients treated with the DK crush technique than in those treated by provisional stenting. According to an additional randomized study12 and a recent meta-analysis,13 in patients with complex bifurcation lesions, the systematic 2-stent approach significantly improved clinical outcomes compared with the provisional stenting strategy. If provisional stenting does not result in positive outcomes in complex lesions, the rule of complex techniques for complex bifurcation lesions seems to be a wise recommendation.14 The key is to identify this type of unfavorable bifurcation lesion. The DEFINITION (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts) study15 proposes a score based on 2 major and 6 minor criteria to differentiate between simple and complex lesions. However, the above-mentioned meta-analysis13 identifies candidates for an upfront 2-stent technique in a simpler way: patients with SB lesion length> 10mm.
Obviously, the Medina classification poses a limitation with regards to the identification of complex bifurcations lesions, as well as to the selection of the subsequent therapeutic strategy. Although modifying the simplicity of the classification carries a risk of losing the spirit of the original description, a slight modification by adding a final letter S (short: SB lesion length <10 mm) or L (long: SB lesion length> 10 mm) may be useful. Thus, (1,1,0), (0,1,0), (1,0,0), (1,1,1,S), (1,0,1,S) and (0,1,1,S) Medina classes should be considered candidates for provisional stenting. In contrast, (1,1,1,L), (1,0,1,L) and (0,1,1,L) would be considered complex bifurcation lesions that could be better treated by an upfront 2-stent technique.
THE MEDINA CLASSIFICATION BY QUANTITATIVE CORONARY ANGIOGRAPHYVisual estimation to assess the severity of angiographic coronary stenosis is an inaccurate method with well-known limitations. The Medina classification is based on visual estimation, and therefore, this limitation affects the precision of the classification. These drawbacks could be overcome by quantitative coronary angiography. However, angiographic analysis of bifurcation lesions poses certain difficulties since software packages for straight vessel analysis are not designed for the complexities of this type of lesion. Therefore, some dedicated 2-dimensional bifurcation quantitative coronary angiography algorithms have been designed. These algorithms incorporate the principles of fractal geometry to address the “step-down” reduction in the diameter of the bifurcation branches: CAAS bifurcation software (Pie Medical Imaging, The Netherlands) and QAngio XA bifurcation software (Medis Medical Imaging Systems, The Netherlands). The EBC consensus in quantitative angiographic methods for bifurcation lesions16 and the Bif-ARC2 both recommend the use of these dedicated software packages according to Medina philosophy. Thus, the minimal lumen diameter, as well as the percentage of stenosis can be calculated in each segment of the bifurcation (proximal, distal, and SB) and a Medina class can be reported based on adapted quantitative coronary angiography.
MEDINA RESTENOSISThe same segmental analysis of the bifurcation used at baseline conditions and postintervention should be also used for follow-up assessment. This analysis will provide details of the location of any residual stenosis postintervention and the precise location of restenosis at follow-up. Based on dedicated bifurcation quantitative coronary angiography, Bif-ARC2 proposes a new nomenclature, according to which any target bifurcation revascularization should be accompanied by the identification of the diseased bifurcation segments using the Medina classification (MEDINA restenosis).
MEDINA COMPUTED TOMOGRAPHY CORONARY ANGIOGRAPHY CLASSIFICATIONPapadopoulou et al.17 have proposed a novel computed tomography (CT)-based Medina classification scheme for bifurcation lesions, combining lumen stenosis and plaque severity. The authors have added an asterisk (*) as a superscript to the existing score of the segments if severe plaque burden (> 70%) is present. As plaque is widely present in all bifurcation segments, even in the absence of coronary lumen stenosis, each 0 of Medina classification may correspond to 0 or 0* in the new CT classification. The CT-Medina classification scheme combining lumen and plaque severity could be more informative than the angiographic classification for the description of atherosclerosis at the bifurcation sites.
A more recent article18 compared coronary CT and conventional angiography for evaluation of the Medina classification. In this setting, the agreement between CT and angiography was poor, resulting in less frequent identification of obstructive SB lesions on noninvasive CT. However, the Medina classification was more reproducible with CT than with angiography.
In summary, although CT has some limitations in the assessment of the severity of coronary stenosis in some bifurcation segments, it definitely provides valuable information on plaque distribution along the bifurcation, like intravascular ultrasound (IVUS) or optical coherence tomography (OCT), but in a noninvasive way.
THE MEDINA CLASSIFICATION BY INTRAVASCULAR IMAGING TECHNIQUESIntravascular imaging techniques (IVUS/OCT) provide a detailed baseline study of the anatomy of the bifurcation. An important point to consider is the composition and distribution of plaque along the bifurcation, which can be precisely analyzed with IVUS/OCT. This can imply a modification of the angiographic Medina classification when the disease is not angiographically significant in any bifurcation segment, but is clearly seen by using these techniques. In this regard, Oviedo et al.19 proposed a modification of the Medina classification according to plaque distribution for the LM bifurcation. In this modification, the LM is classified as 0/0 (no disease), 1/0 (continuous plaque from the LM to the proximal LAD), 0/1 (the plaque spreads from the LM to the left circumflex (LCx), and 1/1 (continuous plaque from the LM into both the proximal LAD and LCx arteries). As in the angiographic classification, the LAD and LCx arteries are classified as diseased (1) or without disease (0).
Bifurcation severity can also be assessed using the minimal lumen area (MLA) at each bifurcation segment. Thus, an IVUS-Medina classification2 can be defined according to an MLA <6mm2 for LM and <4mm2 for ostial LAD and circumflex artery. Although a single cutoff measurement has limitations due to variations in vessel caliber and subtended myocardium, these cutoff points of severity are validated when IVUS is performed at the LM. However, for non-LM bifurcation lesions, MLA measurement is not recommended for the assessment of lesion significance. Additionally, the MLA values established for IVUS evaluation of the LM cannot be directly translated to OCT.20 In these situations, the percentage of stenosis with respect to the reference diameter can be a useful relative value to analyze lesion severity.
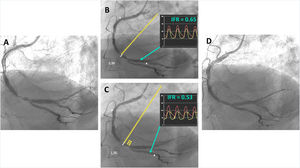
THE MEDINA CLASSIFICATION BY PHYSIOLOGICAL ASSESSMENTPhysiological assessment of coronary lesions is a useful strategy that has several advantages over angiography, IVUS or OCT in the evaluation of intermediate stenosis. However, it is well known that sequential stenosis is difficult to evaluate “individually” with the classic physiological index (fractional flow reserve) since it is determined by the sum of all proximal stenosis. Thus, individual bifurcation segment evaluation can be precisely performed in Medina class (1,0,0), (0,1,0), (0,1,1) and (0,0,1) lesions by placing the pressure wire distally to the MV and SB. In contrast, in class (1,1,1), (1,0,1), (1,1,0) lesions, it would be difficult to establish the individual contribution of each stenosis at the 3 different segments. To overcome these difficulties in sequential lesions, a coregistration between a nonhyperemic index, the instantaneous wave-free ratio (IFR), and angiography has been developed (Syncvision-iFR pullback software, Philips Volcano, Belgium). This approach provides a global distal IFR and, at the same time, a “lesion-level” discrimination of functional significance by superimposed points onto the coronary angiogram (figure 1). A distal IFR less than 0.9 is considered positive and each integrated point onto the vessel represents −0.01 of IFR units. The concentration of these points provides information on the location of the most significant stenosis. Although this novel technology still needs to be validated by new prospective trials, it could potentially be applied to bifurcation lesions, allowing definition of a new Medina-physiological classification (figure 1).
A: bifurcation lesion at the right coronary artery, {1,1,1} on angiography. B: distal IFR and pull back from the PLA: all superimposed points of IFR units are located in the proximal bifurcation segment. C: distal IFR and pull back from the PDA. Apart from points of IFR units in the proximal segment, a second concentration of points appears at the PDA origin. Thus, according to physiological assessment, this bifurcation lesion would be {1,1,0}. D: final result after 1 stent across the bifurcation and POT. IFR, instantaneous wave-free ratio; PDA, posterior descending artery; PLA, posterolateral artery; POT, proximal optimization technique.
Although the Medina classification has succeeded because of its simplicity, this characteristic entails a lack of information that constitutes a limitation per se. Thus, other extensive and complex classifications that provide more detailed information on the characteristics of bifurcations have been proposed, but none of them are as intuitive and easy to use. Additionally, the Medina classification has become a universal common language that can be adapted and modified according to different diagnostic methods or additional anatomic characteristics of the bifurcation. This versatility has also contributed to a wide acceptance that, many years after its first description, still remains.
FUNDINGNone declared.
CONFLICTS OF INTERSESTNone.