Percutaneous coronary intervention (PCI) of chronic total occlusion (CTO) is a demanding situation. This condition causes abnormalities in the vascular bed distal to the lesion and in the related microvasculature. Percutaneous treatment of CTO improves the patient's quality of life and reduces angina.1 Positron emission tomography scans have shown an improvement in myocardial blood flow and coronary flow reserve (CFR) after CTO PCI.2 However, improvement is not immediate and can take weeks or months.3
The Microvascular Coronary Resistance and Absolute Coronary Flow in Patients With Percutaneous Intervention of a Chronic Total Occlusion study (FLOW-CTO; NCT05197361) was designed to evaluate the trend over time of microvascular resistance and absolute coronary flow after CTO PCI. The study was conducted at 4 Spanish sites with consecutive patients who underwent a functional study immediately after the procedure and at 6 months and measured the fractional flow reserve (FFR), CFR, and index of microvascular resistance (IMR). Absolute coronary flow and microvascular resistance were determined by continuous thermodilution during maximum hyperemia induced by serum infusion, as previously described.4 The procedure was performed using the PressureWire X guidewire (Abbott, United States) and the Coroventis program (CoroFlow Cardiovascular System, Sweden). Microvascular dysfunction was defined as IMR ≥ 25 or CFR <2.0 in the presence of FFR> 0.80. The protocol was approved by the Research Ethics Committee for medications at the coordinating site, and all patients provided written informed consent. The data obtained from the baseline study immediately after CTO PCI are presented for the first 49 patients.
Table 1 lists the clinical, angiographic, and procedure characteristics. Most patients were men, and the mean age was 60 to 69 years. The prevalence of hypertension, dyslipidemia, and diabetes was 71%, 67%, and 41%, respectively. More than half the patients had a history of ischemic heart disease, and 55% had required PCI. The median left ventricular ejection fraction was 55% [interquartile range, 45-60]. A total of 86% of patients had exertional angina, and 14% had a history of heart failure.
Baseline, angiographic, and functional study characteristics
| Patients, n | 49 | P |
|---|---|---|
| Age, y | 62 [56-69] | |
| Men | 44 (90) | |
| Hypertension | 35 (71) | |
| Dyslipidemia | 33 (67) | |
| Diabetes mellitus | 20 (41) | |
| Insulin-dependent DM | 6 (12) | |
| History of smoking | 24 (49) | |
| Chronic kidney failure (eGFR <60 mL/min) | 5 (10) | |
| History of ischemic heart disease | 29 (59) | |
| History of AMI | 18 (37) | |
| History of PCI | 27 (55) | |
| History of CABG | 2 (4) | |
| LVEF, % | 55 [45-60] | |
| Exertional angina | 42 (86) | |
| History of heart failure | 7 (14) | |
| Positive ischemia/viability study | 29 (59) | |
| Stress echocardiography | 6 (12) | |
| SPECT | 10 (20) | |
| Cardiac magnetic resonance | 13 (27) | |
| Normal regional contractility + symptoms of myocardial ischemia | 20 (41) | |
| Vessels with CTO | ||
| Anterior descending artery | 15 (31) | |
| Circumflex artery | 7 (14) | |
| Right coronary artery | 27 (55) | |
| Main collateral vessel | ||
| Anterior descending artery | 29 (59) | |
| Circumflex artery | 6 (12) | |
| Right coronary artery | 14 (29) | |
| J-CTO score | 2 [1-2] | |
| PCI-CTO technique | ||
| Antegrade guidewire upgrade | 36 (74) | |
| Retrograde guidewire upgrade | 8 (16) | |
| Antegrade dissection and re-entry | 4 (8) | |
| Retrograde dissection and re-entry | 1 (2) | |
| Number of stents | 2 [1-3] | |
| Total length of stents, mm | 59±25 | |
| Residual stenosis, % | 8±4 | |
| Scope time, min | 37 [29-45] | |
| Contrast administered, mL | 280 [220-350] | |
| Collateral persistence after PCI | ||
| Absent | 29 (59) | |
| Present | 13 (27) | |
| Not evaluated | 7 (14) | |
| FFR | 0.91 [0.83-0.3] | |
| FFR ≤ 0.80 | 10 (20) | |
| IMR | 12 [8-19] | |
| IMR ≥ 25 (only if FFR> 0.80) | 5/37 (14) | |
| CFR | 2 [1.1-2.5] | |
| CFR <2.0 (only if FFR> 0.80) | 19/37 (51) | |
| Microvascular dysfunction | 20/37 (54) | |
| Invasive absolute coronary flow, mL/min | 170 [124-239] | .9119 |
| CTO in anterior descending artery | 168 [127-263] | |
| CTO in circumflex artery | 169 [112-257] | |
| CTO in right coronary artery | 205 [116-239] | |
| Microvascular resistance, mmHg/L/min | 453 [322-642] | .7605 |
| CTO in anterior descending artery | 460 [246-704] | |
| CTO in circumflex artery | 366 [255-642] | |
| CTO in right coronary artery | 433 [326-625] | |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft; CFR, coronary flow reserve; CTO, chronic total occlusion; eGFR, estimated glomerular filtration rate; FFR, fractional flow reserve; IMR, index of microvascular resistance; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention; SPECT, single-photon emission computed tomography.
Data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The vessel most commonly involved was the right coronary artery (55%), followed by the anterior descending artery (31%). The median Japanese Multicenter CTO Registry (J-CTO) score was 2 points. The most frequently used technique (74%) for PCI was antegrade guidewire upgrade, and the median number of stents implanted was 2 (1-3), with a total length of the devices of 59±25mm. Angiographic outcome was good, with a mean residual stenosis of 8%±4%.
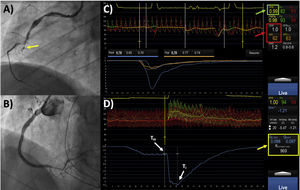
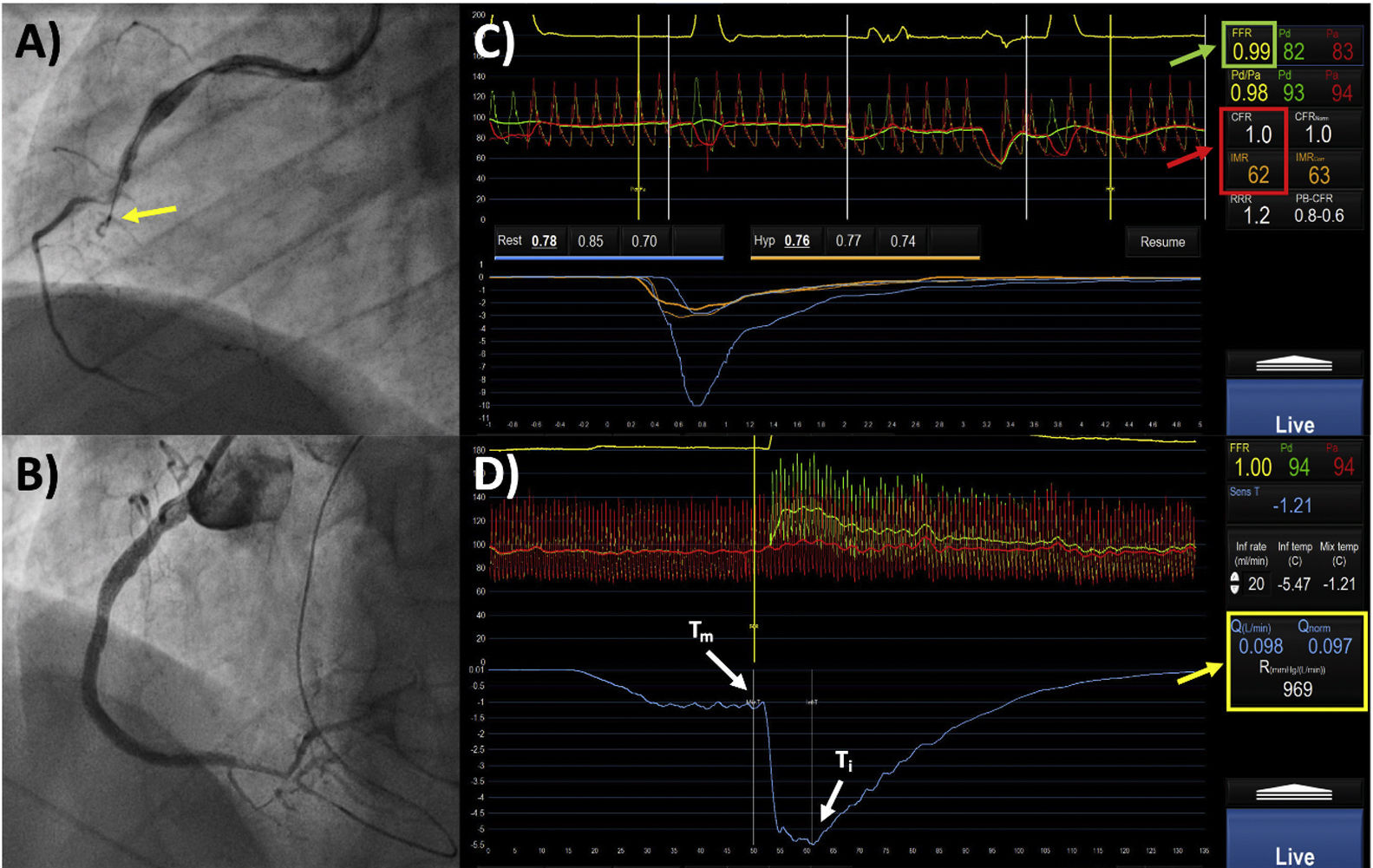
Despite good angiographic outcome, the post-PCI functional study revealed 20% of lesions with FFR ≤0.80. Among patients with an insignificant FFR value (> 0.80), 54% had signs of microvascular dysfunction. Compared with patients with normal IMR, patients with high IMR (≥ 25) showed an insignificant tendency to lower absolute coronary flow (143±79 vs 192±59mL/min; P=.1043), with significantly more elevated microvascular resistance (694±206 vs 471±166mmHg/L/min; P=.0328). However, compared with patients with normal CFR, patients with reduced CFR (< 2.0) had lower absolute coronary flow (166±57 vs 207±64mL/min; P=.0460) and an insignificant tendency toward higher microvascular resistance (535±240 vs 466±195mmHg/L/min; P=.3419). Diabetes mellitus was the only predictor found to be related to high IMR (odds ratio [OR]=6.3; 95% confidence interval [95%CI], 1.1-13; P=.046) or reduced CFR (OR=5.7; 95%CI, 1.4-22; P=.013) immediately after CTO PCI. Figure 1 provides an example of the study protocol.
58-year-old man with diabetes mellitus. Exertional angina with inducible inferior ischemia. A, coronary angiography revealed chronic total occlusion (CTO) of the middle segment of the right coronary (yellow arrow). B, post-PCI angiographic follow-up, with excellent outcome. C, the pressure guidewire study showed an insignificant fractional flow reserve (FFR) (0.99) (green box); the microcirculation study revealed signs of microvascular dysfunction, with a reduced (< 2) coronary flow reserve (CFR) and high index of microvascular resistance (IMR> 25) (red box). D, calculation of absolute coronary flow (Q) and microvascular resistance (R) (yellow box). Ti, temperature at saline infusion site; Tm, temperature of homogeneous mixture of serum and blood.
This prospective study analyzed microcirculation parameters in patients after CTO PCI, finding that more than half the patients exhibited signs of microvascular dysfunction immediately after revascularization. Furthermore, despite an optimal angiographic outcome, a fifth of patients had a functional study showing significant abnormalities in parameters related to epicardial circulation, such as FFR. Microvascular dysfunction was seen more often in the invasive functional study when diabetes mellitus was present. Data analysis during follow-up of this patient cohort will allow us to evaluate whether or not these functional abnormalities improve after CTO PCI.
FUNDINGNo funding was received for this study.
AUTHORS’ CONTRIBUTIONSM. García-Guimarães, lead and corresponding author, designed the study, analyzed the data, and wrote the first version of the manuscript. M. García-Guimarães, A. Gutiérrez-Barrios, J. Gómez-Lara, N. Salvatella, and F. Rivero performed the coronary angiography studies. A. Aparisi participated in the data collection. All authors participated in the final version of the manuscript.
CONFLICTS OF INTERESTNo conflicts of interest related to this project.
We would especially like to thank Dr. Raúl Millán Segovia, who had the original idea that led to the project.