A 40-year-old woman was admitted to the intensive care unit due to pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and subsequently experienced a stroke in the left middle cerebral artery. Cranial computed tomography (CT) showed focal occlusion of the M1 segment and, therefore, mechanical thrombectomy was performed. Lower limb ultrasound ruled out thrombosis. However, contrast-enhanced transthoracic echocardiography (TTE) with agitated saline solution, performed from the peripherally inserted central catheter (PICC) in the left cephalic vein, revealed a massive shunt to the left atrium (LA), with no obvious foramen ovale or interatrial defect. TTE showed direct passage of bubbles from the PICC to the LA, without passing through the right atrium (RA), indicating extracardiac shunt. There was no evidence of cardiac chamber or coronary sinus dilatation, interatrial defect, or ostium secundum in any of the venae cavae. Once the left-sided PICC line was removed, a contralateral PICC was inserted and the TTE was repeated. This time, the agitated saline serum remained only in the right chambers (figure 1, figure 2).
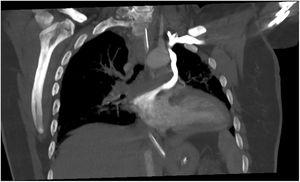
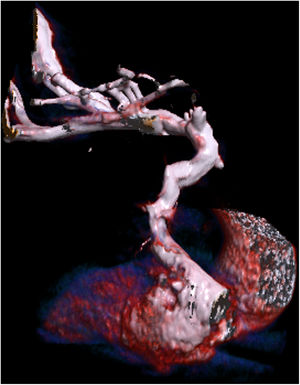
Stroke due to paradoxical embolism was suspected because of abnormal drainage of the venous system of the left arm to the LA. Hence, thoracic CT angiography was performed, revealing the presence of a vein originating in the left subclavian vein, draining a segmental pulmonary vein of the left upper lobe and the LA. Additionally, the innominate vein was severely stenotic, the coronary sinus was normal, and there were no defects between the latter and the LA. Consequently, the differential diagnosis included persistent left superior vena cava (PLSVC) and levoatriocardinal vein.
Diagnostic workup was completed with 72hours of cardiac telemetry, which found no potentially emboligenic arrhythmia. Therefore, the etiology was considered to be paradoxical embolism, facilitated by the left-sided PICC line.
Paradoxical embolism can occur when a thrombus passes from venous to arterial circulation through a vascular or intracardiac defect.1 Approximately 2% of acute arterial ischemia episodes are due to paradoxical embolisms (a rare cause of stroke). The intracardiac defect most often associated with this condition is patent foramen ovale.2 Paradoxical embolism can also arise due to other conditions, such as systemic venous drainage abnormalities that produce right-to-left extracardiac shunting: pulmonary arteriovenous fistulae (Rendu-Osler disease), PLSVC drainage into the LA or a levoatriocardinal vein connecting pulmonary venous circulation (usually the left superior pulmonary vein), and systemic venous circulation (generally the left innominate vein).
The most common abnormality of systemic venous drainage is PLSVC, observed in 0.3% to 0.5% of the total population and 12% of congenital heart diseases. Cases in adults are primarily diagnosed after placement of central venous catheters (CVCs).3 The PLSVC usually drains to the RA through the coronary sinus in 80% to 92% of cases and to the LA in 10% to 20% (directly or through a partial defect of the coronary sinus roof), leading to a right-to-left shunt, with stronger predisposition toward paradoxical embolisms.4 The most characteristic echocardiographic marker, not always present, is coronary sinus dilatation.3
Conversely, a levoatriocardinal vein is a persistent abnormal connection between the pulmonary and systemic venous systems through the celiac plexus that is commonly associated with congenital heart diseases with left chamber obstruction (hypoplastic left ventricle).5 Due to the current availability of advanced radiologic techniques (CT angiography), this rare malformation is diagnosed more often. It can be an isolated asymptomatic abnormality, diagnosed incidentally, that produces extracardiac shunting between the pulmonary and systemic venous circuits.
In our patient, venous-phase CT angiography visualized contrast opacification through the left subclavian vein and toward an irregular venous structure, which drained into the segmental vein of the left upper lobe and then into the LA. Likewise, another venous structure of smaller diameter and scant contrast flow was observed in the course of the left innominate vein, and a component of fibrosis or chronic thrombosis could not be ruled out. The right superior vena cava was of normal diameter, and both the right subclavian vein and the jugular vein appeared to be normal.
Because echocardiography showed no coronary sinus dilation (a characteristic marker of PLSVC) and no significant right-to-left shunting was observed, the radiologic findings could indicate a levoatriocardinal venous malformation (which would connect the left superior pulmonary vein with the left innominate vein) even though no obstructive left-sided heart abnormalities were observed. Plain TTE from the suprasternal (or high parasternal) position can show the left vertical vein, and color Doppler ultrasound can visualize intravascular flow in the ascending or descending direction. In our patient, however, TTE was unable to confirm its presence due to endotracheal intubation and poor suprasternal access.
Although venous drainage abnormalities are often associated with birth defects in children, they are sometimes detected during adulthood. Other cases reported in the literature are usually diagnosed after CVC placement. Consequently, in the case of paradoxical embolism after CVC placement, possible anatomic variants of the venous drainage system should be studied as the possible cause.