To the Editor:
Essential thrombocythaemia (ET) is a myeloproliferative disease characterised by megakaryocytic hyperplasia in the bone marrow,1 with an overproduction of dysfunctional platelets in the peripheral blood. It develops with complications, both haemorrhagic and thrombotic (more frequently arterial),2 and an incidence of coronary thrombosis of up to 9.4% has been described.3
We present the case of a 54-year-old male, ex-smoker, who arrives at the hospital with a piercing pain in the left hemithorax, of continual development over the previous 3 days. The pain worsens with deep inspiration and improves on bending forward. He had been experiencing cold symptoms and fever from the previous week.
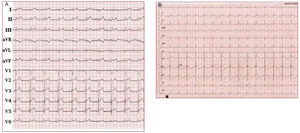
He had a fever of 38.5ºC in the emergency unit. His blood pressure was 95/60 mm Hg and heart rate 95 beats/min. No murmurs or friction rubs were found on auscultation. An electrocardiogram was performed (Figure 1A), in which general repolarization changes were noted, with ST segment elevation, concave morphology on inferior and lateral leads, J point elevation of V2 to V5 and slight PR depression in leads II, III, and aVF.
Figure 1. A: electrocardiogram on admission, compatible with acute pericarditis. B: second electrocardiogram, concordant with a previous myocardial infarction.
Based on the clinical results and the electrocardiogram, he was diagnosed with acute pericarditis. An emergency full blood count was performed, showing leukocyte numbers at 16 000/ μL, C-reactive protein (CRP) at 14 mg/dL, and troponin I at 19.3 ng/mL. The platelet count was alarming (1 420 000/μL, checked several times). All other parameters were normal.
After administering anti-inflammatory medicines, the patient experienced an important improvement from the pain, although he still had slight but continuous discomfort on his left side, localised to the touch. However, a routine ECG performed in the next hours (Figure 1B) showed convex elevation of the ST segment of up to 4 mm in the precordium, more pronounced from V3 to V5 and of less magnitude in the area below and V6.
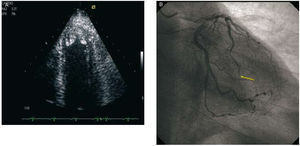
Given the discordance between the symptoms and the ECG, an echocardiogram was carried out, which showed a left ventricle with severe apical hypokinesia. Two rounded images of moderate echogenicity, hyperechogenic edge, and low mobility, were visualised adhered to the apical endocardium, which indicated possible mural thrombi (Figure 2A). The ejection fraction of the left ventricle was of 60% and there was no pericardial effusion.
Figure 2. A: apical thrombi viewed through echocardiography. B: angiographic image showing thrombotic occlusion in the anterior descending distal artery.
In view of the findings, a cardiac catheterization was requested. This evidenced a subtotal stenosis in the distal 1/3 radius of the anterior descending artery (Figure 2B), with an elongated intraluminal image compatible with thrombus (indicated with an arrow). The circumflex and the right coronary presented no lesions.
Taking into account the marked thrombocytosis and the presence of thrombotic disease, the possibility of an ET was considered,4 and a haematology evaluation was requested. The tests performed in this sense (abdominal ultrasound, granulocytic alkaline phosphatase, peripheral blood smear, and studies of genes JAK2 and BCR-ABL) were normal. Furthermore, there was a progressive and spontaneous platelet count decline, which reached normal values (311 000/μL) within 3 weeks. All of the above excluded the possibility of ET and the final diagnosis was of reactive thrombocytosis (RT).
RT is the most frequent thrombocytosis (80%-90%).5 The most frequent causes are infections, chronic inflammatory diseases, and neoplasia, and its origin is related with the presence of proinflammatory cytokines (thrombopoietin, interleukin 6, PCR).6 The diagnosis is usually incidental and the absolute platelet values are not directly related with the aetiology of the thrombocytosis, although there is data which differentiates the RT from the ET7: thrombotic or haemorrhagic phenomena are infrequent in the RT, since the platelets are normal with regard to morphology and functionality. In addition, there is no splenomegaly, present in 40% of ET patients. Finally, as illustrated in the case presented, the platelet count tends to normalise once the trigger process has been corrected.
We conclude by emphasizing how unusual this case is. The pericarditis suffered by the patient not only caused the coronary thrombosis mediated by a reactive thrombocytosis, but it also masked the ischaemic symptoms and led the thrombocytosis study towards a clonal origin.