High-sensitivity troponin assays have improved the diagnosis of acute coronary syndrome in patients presenting with chest pain and normal troponin levels as measured by conventional assays. Our aim was to investigate whether N-terminal pro-brain natriuretic peptide provides additional information to troponin determination in these patients.
MethodsA total of 398 patients, included in the PITAGORAS study, presenting to the emergency department with chest pain and normal troponin levels as measured by conventional assay in 2 serial samples (on arrival and 6 h to 8h later) were studied. The samples were also analyzed in a central laboratory for high-sensitivity troponin T (both samples) and for N-terminal pro-brain natriuretic peptide (second sample). The endpoints were diagnosis of acute coronary syndrome and the composite endpoint of in-hospital revascularization or a 30-day cardiac event.
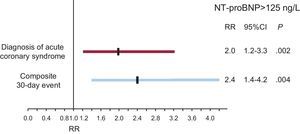
ResultsAcute coronary syndrome was adjudicated to 79 patients (20%) and the composite endpoint to 59 (15%). When the N-terminal pro-brain natriuretic peptide quartile increased, the diagnosis of acute coronary syndrome also increased (12%, 16%, 23% and 29%; P=.01), as did the risk of the composite endpoint (6%, 13%, 16% and 24%; P=.004). N-terminal pro-brain natriuretic peptide elevation (>125ng/L) was associated with both endpoints (relative risk= 2.0; 95% confidence interval, 1.2-3.3; P=.02; relative risk=2.4; 95% confidence interval, 1.4-4.2; P=.004). However, in the multivariable models adjusted by clinical and electrocardiographic data, a predictive value was found for high-sensitivity T troponin but not for N-terminal pro-brain natriuretic peptide.
ConclusionsIn low-risk patients with chest pain of uncertain etiology evaluated using high-sensitivity T troponin, N-terminal pro-brain natriuretic peptide does not contribute additional predictive value to diagnosis or the prediction of short-term outcomes.
Keywords
In patients attending the emergency service for chest pain who have normal troponin levels, decision making requires careful evaluation of the medical history,1,2 electrocardiogram (ECG),3 exercise test,4 imaging stress test5 or coronary computed tomographic angiography.6 In a considerable proportion of patients with normal troponin levels, chest pain is due to acute coronary syndrome (ACS). In this complex scenario, a biomarker that would be readily available 24h per day/7 days per week and that could add to the information provided by troponin would be extremely useful.
Among the various biomarkers studied, those that have most consistently been shown to have prognostic value in the entire spectrum of ACS, including the subgroup of patients with normal troponin levels,7–16 are natriuretic peptides. Nevertheless, most studies of these peptides were performed before the introduction of high-sensitivity troponin assays and consequently the utility of these peptides as a possible addition to risk stratification using high-sensitivity troponins is unknown.
The PITAGORAS (troPonIna ulTrAsensible en pacientes atendidos en urGencias por dOlor toRácico in hospitales espAñoleS [in English: High-Sensitivity Troponin in Patients With Chest Pain Presenting To Spanish Emergency Departments]) is a multicenter study performed in Spain that evaluated the Elecsys® high-sensitivity troponin T (hs-TnT) assay (Roche Diagnostics; Basil, Switzerland) in patients with chest pain and normal troponin levels measured by conventional assays. The principal results of this study indicated that the main instruments for the diagnosis of ACS in these patients are the clinical history and ECG, although undetectable hs-TnT levels had a high negative predictive value that could be clinically useful.17 The aim of the present study was to analyze whether the N-terminal pro-brain natriuretic peptide (NT-proBNP) provides additional information to hs-TnT determination in establishing the diagnosis and prognosis of these patients.
MATERIAL AND METHODSPITAGORAS is a Spanish prospective multicenter study designed by the Section for Ischemic Heart Disease and Coronary Care Units of the Spanish Society of Cardiology. The main objective of this study was to evaluate the role of hs-TnT in the diagnosis of ACS in patients presenting to the emergency department with chest pain and who have normal troponin levels as measured by the reagents used in the routine clinical practice of each hospital. The participating hospitals are listed in the Appendix.
The methodology of the PITAGORAS study and its principal results concerning hs-TnT have previously been described.17 Briefly, the study included patients presenting to the emergency department for chest pains of uncertain etiology with onset in the previous 24h and who were suspected of having ACS in the opinion of the duty cardiologist. The exclusion criteria were as follows: a) persistent ST-segment elevation on the emergency ECG; b) elevated troponin levels in 1 of 2 serial determinations (at arrival at the emergency department and 6 h to 8h later) as determined by the method routinely used in each hospital; c) a prior diagnosis of myocardial ischemia established by a finding of significant coronary stenosis in a previous coronary angiogram or prior documented myocardial infarction; d) left bundle branch block or other ventricular repolarization alterations that could make the result of an exercise test impossible to interpret, or physical inability to perform exercise; e) known structural heart disease other than myocardial ischemia, and f) significant concomitant heart failure, or bradyarrhythmia (<55 bpm), or tachyarrhythmia (>110 bpm).
The total population included in the PITAGORAS study consisted of 446 patients. Due to logistic difficulties in the referring hospitals or in the central laboratory where the hs-TnT and NT-proBNP determinations were performed, data on NT-proBNP were unavailable in 48 patients due to the lack of to blood sample. Consequently, the present subanalysis was performed in a population of 398 patients.
Determination of High-sensitivity Troponin T and N-terminal Pro-brain Natriuretic PeptideTwo blood samples were obtained for troponin determination with the method routinely used in each hospital. These samples were also used to determine hs-TnT in a single central laboratory. In the second sample (taken 6 h to 8h after arrival at the emergency department) NT-proBNP was also obtained. To do this, all the blood samples were centrifuged after extraction and were then frozen at −80°C and transferred to the central laboratory for biomarker measurement. Both hs-TnT and NT-proBNP determinations were performed using their respective assays in an automatic immunochemical analyzer Cobas e601 (Roche Diagnostics; Basil, Switzerland). The limit of detection for hs-TnT is 3ng/L and the 99th percentile of the reference limit of a healthy population is 14ng/L. The upper reference limit recommended by the manufacturer for NT-proBNP is 125ng/L.
Diagnostic ProtocolClinical variables were gathered in all patients (Table 1). The approach adopted was guided by the findings of the ECG performed in the emergency department. Patients with an ECG suggestive of ischemia (ST-segment depression≥0.5mm or negative T wave≥2mm in 2 adjacent leads) were admitted for coronary angiography. The remaining patients were assigned to a noninvasive test for ischemia (preferentially to a conventional exercise text or stress cardiac imaging according to the routine practice in each hospital). If the results of the test were positive, coronary angiography was indicated; if the results were negative, the patient was discharged, and if the results were inconclusive, coronary angiography or an alternative test for ischemia was performed (although coronary angiography was recommended by the protocol).
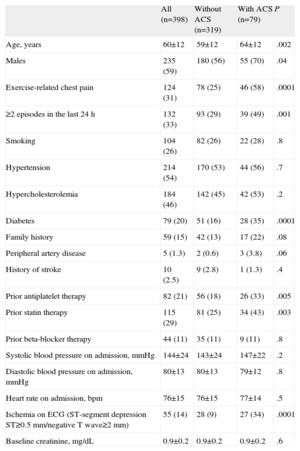
Characteristics of the Total Population and the Subgroups With and Without a Final Diagnosis of Acute Coronary Syndrome.
| All (n=398) | Without ACS (n=319) | With ACS (n=79) | P | |
| Age, years | 60±12 | 59±12 | 64±12 | .002 |
| Males | 235 (59) | 180 (56) | 55 (70) | .04 |
| Exercise-related chest pain | 124 (31) | 78 (25) | 46 (58) | .0001 |
| ≥2 episodes in the last 24 h | 132 (33) | 93 (29) | 39 (49) | .001 |
| Smoking | 104 (26) | 82 (26) | 22 (28) | .8 |
| Hypertension | 214 (54) | 170 (53) | 44 (56) | .7 |
| Hypercholesterolemia | 184 (46) | 142 (45) | 42 (53) | .2 |
| Diabetes | 79 (20) | 51 (16) | 28 (35) | .0001 |
| Family history | 59 (15) | 42 (13) | 17 (22) | .08 |
| Peripheral artery disease | 5 (1.3) | 2 (0.6) | 3 (3.8) | .06 |
| History of stroke | 10 (2.5) | 9 (2.8) | 1 (1.3) | .4 |
| Prior antiplatelet therapy | 82 (21) | 56 (18) | 26 (33) | .005 |
| Prior statin therapy | 115 (29) | 81 (25) | 34 (43) | .003 |
| Prior beta-blocker therapy | 44 (11) | 35 (11) | 9 (11) | .8 |
| Systolic blood pressure on admission, mmHg | 144±24 | 143±24 | 147±22 | .2 |
| Diastolic blood pressure on admission, mmHg | 80±13 | 80±13 | 79±12 | .8 |
| Heart rate on admission, bpm | 76±15 | 76±15 | 77±14 | .5 |
| Ischemia on ECG (ST-segment depression ST≥0.5 mm/negative T wave≥2 mm) | 55 (14) | 28 (9) | 27 (34) | .0001 |
| Baseline creatinine, mg/dL | 0.9±0.2 | 0.9±0.2 | 0.9±0.2 | .6 |
ACS, acute coronary syndrome; ECG, electrocardiogram.
Values are expressed as no. (%) or mean±standard deviation.
The primary endpoint was diagnosis of ACS as the cause of chest pain, with consensus on this diagnosis being reached by 3 cardiologists who were blind to the results of hs-TnT testing. The criterion for the diagnosis of ACS was angiographic evidence of significant coronary stenosis or, if angiography had not been performed, a positive result of a noninvasive test for ischemia, or the occurrence of a 30-day cardiac event. To ensure the robustness of the diagnosis, the protocol recommended the performance of angiography after an ECG result suggesting ischemia or after a positive or inconclusive result of a noninvasive test for ischemia. Likewise, the study's exclusion criteria included evidence of coronary stenosis in a prior coronary angiogram, because, in these patients, a current coronary angiogram would always lead to a diagnosis of ACS.
The secondary endpoint was the composite endpoint of revascularization or a 30-day cardiac event, including death or acute myocardial infarction (a new episode of chest pain with elevated troponin levels). An acute myocardial infarction was also deemed to have occurred when the creatine-kinase-MB mass increased to ≥3 times the upper limit of normality after coronary angioplasty, or to ≥5 times this limit after coronary surgery, evaluated at 8 h and 24h after the revascularization procedure.
Statistical AnalysisContinuous variables are presented as the mean (standard deviation), and qualitative variables as absolute values and percentages. Hs-TnT was used in such to way that the results of the PITAGORAS study showed their best discriminative ability: the highest of the 2 hs-TnT determinations was taken and the population was divided into 3 categories: <3ng/L (undetectable levels), ≥3 ng/L but <14 ng/L (levels were detectable but below the 99th percentile), and ≥14ng/L (levels above the 99th percentile).17
Because the distribution of NT-proBNP followed a non-normal pattern, values for this variable are presented as median and interquartile ranges. In the univariable analysis to compare values among groups with and without the primary and secondary endpoints, a nonparametric test was used (Mann-Whitney test). The population was distributed among the NT-proBNP quartiles and the groups were compared by using the chi-square test. Likewise, the population was dichotomized by taking the cut-off point for the upper limit of normality recommended by the manufacturer (>125ng/L) and estimating relative risks (RR) with their 95% confidence intervals (95%CI). The sensitivity, specificity, positive predictive value, negative predictive value, and 95%CI were calculated for NT-proBNP>125ng/L and for hs-TnT≥14ng/L (the cut-point corresponding to the 99th percentile of the reference population). For the multivariable analysis, a binary logistic regression was used (backward conditional method with an exit criteria; P=.1) in which the clinical and ECG variables related to the endpoints in the univariable analysis, hs-TnT and NT-proBNP, were introduced. Odd ratio (OR), 95%CI and the C statistic were calculated.
The statistical analysis was performed using the SPSS 18.0 statistical package (SPSS Inc.; Chicago, Illinois, United States).
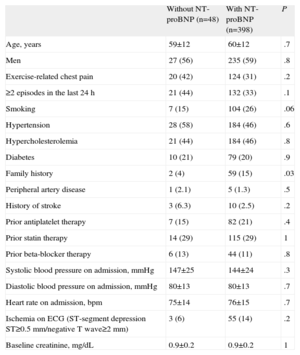
RESULTSCharacteristics of the PopulationTable 1 shows the characteristics of the study population. Table 2 shows the differences with the population in the PITAGORAS study who were excluded (n=48) due to lack of a blood sample for NT-proBNP determination. There were no differences between the 2 groups, except that the frequency of smoking and a family history of myocardial ischemia was higher in patients included in the NT-proBNP substudy.
Comparison of Population Characteristics Between Patients Included in the N-terminal Pro-brain Natriuretic Peptide Substudy and Those not Included due to the Lack of a Blood Sample for N-terminal Pro-brain Natriuretic Peptide Determination.
| Without NT-proBNP (n=48) | With NT-proBNP (n=398) | P | |
| Age, years | 59±12 | 60±12 | .7 |
| Men | 27 (56) | 235 (59) | .8 |
| Exercise-related chest pain | 20 (42) | 124 (31) | .2 |
| ≥2 episodes in the last 24 h | 21 (44) | 132 (33) | .1 |
| Smoking | 7 (15) | 104 (26) | .06 |
| Hypertension | 28 (58) | 184 (46) | .6 |
| Hypercholesterolemia | 21 (44) | 184 (46) | .8 |
| Diabetes | 10 (21) | 79 (20) | .9 |
| Family history | 2 (4) | 59 (15) | .03 |
| Peripheral artery disease | 1 (2.1) | 5 (1.3) | .5 |
| History of stroke | 3 (6.3) | 10 (2.5) | .2 |
| Prior antiplatelet therapy | 7 (15) | 82 (21) | .4 |
| Prior statin therapy | 14 (29) | 115 (29) | 1 |
| Prior beta-blocker therapy | 6 (13) | 44 (11) | .8 |
| Systolic blood pressure on admission, mmHg | 147±25 | 144±24 | .3 |
| Diastolic blood pressure on admission, mmHg | 80±13 | 80±13 | .7 |
| Heart rate on admission, bpm | 75±14 | 76±15 | .7 |
| Ischemia on ECG (ST-segment depression ST≥0.5mm/negative T wave≥2 mm) | 3 (6) | 55 (14) | .2 |
| Baseline creatinine, mg/dL | 0.9±0.2 | 0.9±0.2 | 1 |
ECG, electrocardiogram; NT-proBNP, N-terminal pro-brain natriuretic peptide.
Values are expressed as no. (%) or mean±standard deviation.
The median interval from the onset of chest pain to extraction of the first blood sample was 4h (interquartile range, 3 h to 6h). The median NT-proBNP value was 66ng/L (range, 5 ng/L to 2536ng/L; interquartile range, 35 ng/L to 154ng/L). Distribution of the patients by hs-TnT subgroups was as follows: <3ng/L, 134 (34%); ≥3 ng/L but <14 ng/L, 206 (52%), and ≥14ng/L, 58 (15%).
ACS was diagnosed in 79 patients (20%). The criterion for diagnosis was evidence of coronary stenosis on coronary angiography in 71 patients (90%), a positive test for ischemia in 7 patients who refused to undergo coronary angiography, and a 30-day event (readmission for unstable angina and revascularization) in 1 patient who had been discharged after a negative exercise test. Table 1 shows the differences in the baseline characteristics between the subgroups with and without ACS.
The composite endpoint occurred in 59 patients (15%). There were no deaths. Acute myocardial infarction occurred in 6 patients (of these, 4 were related to the revascularization procedure), and revascularization was performed in 58 patients.
Univariable AnalysisNT-proBNP levels were higher in patients with a final diagnosis of ACS or the 30-day composite event than in the remaining patients median [interquartile range]: 98 [51-260] vs 59 [33-122] ng/L, for the diagnosis of ACS (P=.001); 101 [53-261] vs 62 [33-122] ng/L, for the composite event (P=.001).
Figure 1 shows the distribution of the study's endpoints according to NT-proBNP quartiles (<35, 35-66, 66-154, >154ng/L). The frequency of both diagnosis of ACS (n=12, 12%; n=15, 16%; n=23, 23%; and n=29, 29%; P=.01) and the composite event (n=6, 6%; n=13, 13%; n=16, 16%; and n=24, 24%; P=.004) progressively increased with increasing NT-proBNP quartiles.
Elevated NT-proBNP levels (>125ng/L) were found in 110 patients (28%). NT-proBNP elevation was associated with a diagnosis of ACS (28% vs 17%; RR=2.0; 95%CI, 1.2 to 3.3; P=.02) and with the composite event (24% vs 12%; RR=2.4; 95% CI, 1.4 to 4.2; P=.004) (Fig. 2).
Table 3 shows the agreement/disagreement between NT-proBNP>125ng/L and hs-TnT≥14ng/L for the diagnosis of ACS and the composite event. The sensitivity, specificity and positive and negative predictive values (with 95%CI) of NT-proBNP for the 2 endpoints, respectively, were as follows: sensitivity: 39% (29% to 50%) and 44% (32% to 57%); specificity: 75% (70% to 80%) and 75% (70% to 80%); positive predictive value: 28% (21% to 37%) and 24% (17% to 33%); negative predictive value: 83% (79% to 87%) and 89% (84% to 92%). The corresponding values for hs-TnT≥14ng/L were as follows: sensitivity 30% (21% to 41%) and 34% (23% to 47%); specificity: 89% (85% to 92%) and 89% (85% to 92%); positive predictive value: 41% (30% to 54%) and 35% (24% to 48%); and negative predictive value: 84% (80% to 87%) and 89% (85% to 91%).
Number of Patients With and Without Elevation of High-sensitivity Troponin T and N-terminal Pro-brain Natriuretic Peptide in the Subgroups With and Without a Diagnosis of Acute Coronary Syndrome and With and Without Events.
| NT-proBNP, ng/L | With ACS (n=79) | Without ACS (n=319) | ||
| Hs-TnT<14 ng/L | Hs-TnT≥14 ng/L | Hs-TnT<14 ng/L | Hs-TnT≥14 ng/L | |
| <125 | 40 (73) | 8 (33) | 225 (79) | 15 (44) |
| >125 | 15 (27) | 16 (67) | 60 (21) | 19 (56) |
| With events (n=59) | Without events (n=339) | |||
| <125 | 27 (69) | 6 (30) | 238 (79) | 17 (45) |
| >125 | 12 (31) | 14 (70) | 63 (21) | 21 (55) |
ACS, acute coronary syndrome; hs-TnT, high-sensitivity troponin T; NT-proBNP, N-terminal pro-brain natriuretic peptide.
The percentages refer to those within each hs-TnT category.
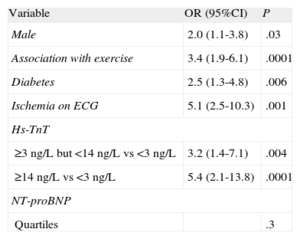
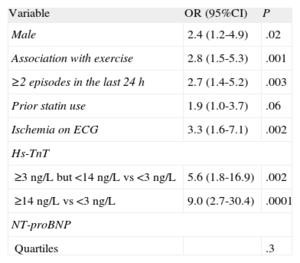
Tables 4 and 5 show the multivariable models for the endpoints of the study, including clinical variables, ECG data, hs-TnT, and NT-proBNP. The variables related to a diagnosis of ACS or the composite event were male sex, association of chest pain with exercise, 2 or more episodes of chest pain in the last 24h, diabetes, prior statin therapy, and a finding of ischemia on the el ECG.
Multivariable Model with Clinical Variables N-terminal Pro-brain Natriuretic Peptide and High-sensitivity Troponin T for the Diagnosis of Acute Coronary Syndrome.
| Variable | OR (95%CI) | P |
| Male | 2.0 (1.1-3.8) | .03 |
| Association with exercise | 3.4 (1.9-6.1) | .0001 |
| Diabetes | 2.5 (1.3-4.8) | .006 |
| Ischemia on ECG | 5.1 (2.5-10.3) | .001 |
| Hs-TnT | ||
| ≥3 ng/L but <14 ng/L vs <3 ng/L | 3.2 (1.4-7.1) | .004 |
| ≥14 ng/L vs <3 ng/L | 5.4 (2.1-13.8) | .0001 |
| NT-proBNP | ||
| Quartiles | .3 | |
95%CI, 95% confidence interval; ECG, electrocardiogram; hs-TnT, high-sensitivity troponin T; NT-proBNP, N-terminal pro-brain natriuretic peptide; OR, odds ratio.
Multivariable Model With Clinical Variables, N-terminal Pro-brain Natriuretic Peptide and High-sensitivity Troponin T for the 30-day Composite Event.
| Variable | OR (95%CI) | P |
| Male | 2.4 (1.2-4.9) | .02 |
| Association with exercise | 2.8 (1.5-5.3) | .001 |
| ≥2 episodes in the last 24 h | 2.7 (1.4-5.2) | .003 |
| Prior statin use | 1.9 (1.0-3.7) | .06 |
| Ischemia on ECG | 3.3 (1.6-7.1) | .002 |
| Hs-TnT | ||
| ≥3 ng/L but <14 ng/L vs <3 ng/L | 5.6 (1.8-16.9) | .002 |
| ≥14 ng/L vs <3 ng/L | 9.0 (2.7-30.4) | .0001 |
| NT-proBNP | ||
| Quartiles | .3 | |
95%CI, 95% confidence interval; ECG, electrocardiogram; hs-TnT, high-sensitivity troponin T; NT-proBNP, N-terminal pro-brain natriuretic peptide; OR, odds ratio.
A strong association was found between hs-TnT and diagnosis of ACS (hs-TnT≥3 but <14ng/L vs <3ng/L; OR=3.2; 95%CI, 1.4 to 7.1; P=.004; hs-TnT ≥14ng/L vs <3ng/L; OR=5.4; 95%CI, 2.1 to 13.8; P=.0001) and with the composite event (hs-TnT≥3 but <14ng/L vs <3ng/L; OR=5.6; 95%CI, 1.8 to 16.9; P=.002; hs-TnT≥14ng/L vs <3ng/L; OR=9.0; 95%CI, 2.7 to 30.4; P=.0001). However, NT-proBNP lacked predictive value (P=.3 for both endpoints). No significant differences were found in the C statistic of the models with and without NT-propBNP for diagnosis of ACS (0.805 and 0.804) or for the composite event (0.836 and 0.842).
DISCUSSIONThe results of the present study show that, in patients presenting to the emergency department for chest pain without myocardial injury, or with only minimal damage, not detected by conventional troponin assays, hs-TnT provides information on diagnosis and prognosis and can therefore help in decision making. In contrast, NT-proBNP does not add to the information provided by hs-TnT and should not be routinely used.
N-terminal Pro-brain Natriuretic Peptide and Chest PainMyocardial ischemia provokes changes in the ventricular contractility and relaxation, which releases natriuretic peptides. Moreover, ischemia per se also facilitates the release of these substances.18 Consequently, there is a rational basis for considering that natriuretic peptides might be of value in risk stratification in ACS in addition to their value in heart failure.
Studies performed in the entire spectrum of ACS, including those occurring in patients with normal troponin levels, have shown that elevated natriuretic peptide levels were associated with an increased risk of cardiovascular events.7–16 Moreover, in some of these studies, these substances provided additional prognostic value to that provided by troponin.15 Specifically, in patients with chest pain and normal troponin levels, evaluated in chest pain units, NT-proBNP elevations increased the 1-year risk of death or myocardial infarction.12 Low NT-proBNP levels in patients with chest pain and normal troponin levels could be used to identify low-risk patients who are candidates for discharge from the emergency service.13 Likewise, in primary prevention, natriuretic peptide elevation allowed identification of both silent heart disease19 and estimation of the 10-year risk of cardiovascular events independently of traditional risk factors and other biomarkers.20
In the present study, however, NT-proBNP was only marginally useful in the evaluation of chest pain or uncertain etiology when hs-TnT was also employed. This result could be explained by several factors: a) the greater sensitivity of the reagent used in the Elecsys® hs-TnT assay in detecting myocardial injury, which is superior to the sensitivity of that used in other studies21,22; b) in the PITAGORAS study, clinical data and risk factors were carefully gathered, allowing rigorous adjustment to the multivariable model. In particular, in the clinical history, the association between chest pain during exercise and recurrent pain was recorded, an association that previous studies have shown to be strongly associated with diagnosis of ACS and prognosis in patients with the same characteristics as those enrolled in the PITAGORAS study1,2,23; c) the most consistent association found for natriuretic peptides in previous studies has been with major cardiovascular events, particularly mortality, and in the long term. Due to its design, the PIGAGORAS study included low-risk patients in the population with normal troponin levels, who are those without a prior history of ischemic heart disease. Thus, the events registered were mainly revascularizations prompted by the results of noninvasive tests and coronary angiography. However, the follow-up period was only 30 days. Nevertheless, when decisions are taken in the emergency department, identifying the patients in this population who could require a revascularization procedure in the short term is a priority, even though the benefits of revascularization in some low-risk patients might be questionable24; d) in ACS, the peak NT-proBNP value appears between 16 h and 24h after arrival at the emergency department25; in the PITAGORAS study, this determination was made between 6 h and 8h after arrival at the emergency department. Determination at 24h might have increased the predictive value; and e) the sample size of the study may have been insufficient, although the number of patients included was sufficient to demonstrate the predictive value of hs-TnT.
High-sensitivity Troponin TThe introduction of hs-TnT assays has modified the evaluation of patients with chest pain because elevations occur earlier in hs-TnT than in conventional troponins; in addition, hs-TnT can identify patients with myocardial damage that was previously undetected by conventional troponin assays.26–29 Nevertheless, the PITAGORAS study showed that the clinical history and ECG are essential in the evaluation of patients without myocardial injury or with minimal damage. The higher the hs-TnT levels, the greater the probability of a diagnosis of ACS and the risk of events, although the most important datum was the high negative predictive value of the absence of detectable hs-TnT levels in 2 serial determinations. The results of the present substudy suggest that NT-proBNP does not provide significant additional information in this context and, in view of cost/effectiveness considerations, should not be routinely determined when hs-TnT is used.
LimitationsA total of 48 patients in the PITAGORAS study were not included in the present substudy of NT-proBNP due to lack of a blood sample. Nevertheless, no relevant differences were found in the characteristics of patients who were not included.
CONCLUSIONSIn low-risk patients with chest pain of uncertain etiology, such as those included in the PITAGORAS study, who were evaluated with hs-TnT, the use of NT-proBNP provides no additional information to diagnosis or estimation of short-term prognosis. These conclusions should not be extrapolated to patients at higher risk or to evaluation of major cardiovascular events, such as mortality or myocardial infarction, in the long term.
FUNDINGAn unrestricted grant from Roche Diagnostics (Basil, Switzerland). Instituto de Salud Carlos III (FEDER), Red HERACLES (Drs. Sanchis and Bosch) and Red RECAVA (Drs. Sánchez, Hernández and Barrabés).
CONFLICTS OF INTERESTNone declared.
Hospital Clínico Universitario, Valencia: Juan Sanchis, Arturo Carratalá, Lidia Abellán, Mauricio Pellicer and Cristina Gómez-Monsoliu; Hospital Universitari Vall de Hebrón, Barcelona: Jose A. Barrabés, Albert Alonso and Luzma Cruz; Hospital Universitari Joan XXIII, Tarragona: Alfredo Bardají and Angels Vilanova; Hospital Gregorio Marañón, Madrid: Pedro L. Sánchez, Mercedes García and Carolina Puerta; Hospital Meixoeiro, Vigo: Fran Calvo and Carmen Farreirós; Hospital Clínic, Barcelona: Xavier Bosch, Jose L. Bedini and Bernat González; Hospital Josep Trueta, Girona: Pablo Loma, Manel Ramírez, Marina Fontant and Francisco Campelo Parada; Hospital Clínico Universitario, Valladolid: Carolina Hernández, Alberto San Román, Encarna Lago and Inmaculada Vidriales; Hospital Virgen de la Arrixaca, Murcia: Francisco Marín, Ana Romero and Pedro Martínez; Hospital General de Asturias: Pablo Avanzas and Francisco Álvarez; Hospital Germans Trías i Pujol, Badalona: Silvia Serrano and Amparo Galán.