Keywords
The noninvasive assessment of left ventricular contractile reserve is relevant to the clinical management of patients with ischemic heart disease and systolic dysfunction. Conventional imaging techniques that assess contractile reserve include echocardiography,1-9 gated-SPECT,6-18 magnetic resonance imaging19,20 and, less frequently, cardiac computerized tomography21 and cardiac catheterization22 with low-dose dobutamine (LDD) infusion. At low doses, dobutamine can increase contractility without inducing ischemia. In clinical practice, the results of these tests provide relevant data that can influence decisions regarding treatment.
The analysis of left ventricular contractile reserve normally focuses on assessing improvements in myocardial wall thickening or contractility using LDD infusion or a biphasic response during echocardiography as indicators of myocardial viability. In general, less attention is paid to the segments in which contractility decreases with LDD (negative contractile response [NCR]). The aim of this study was to analyze, using gated-SPECT myocardial perfusion with LDD, the decrease in left ventricle (LV) wall segment thickening in patients with ischemic cardiomyopathy (IC) and its relationship to overall left ventricular systolic function, with evidence of viability provided by scintigraphy and with normal coronary anatomy.
METHODS
Patients
A total of 68 consecutive patients <75 years of age with a diagnosis of IC were assessed using gated-SPECT myocardial perfusion at rest and during LDD infusion. The patients were recruited from 8 hospitals and, at the discretion of their clinical cardiologist, underwent gated-SPECT at rest for the myocardial viability study. The images were sent to a Centralized Imaging Unit for analysis. Ischemic cardiomyopathy was defined as confirmed coronary artery disease using contrast-enhanced coronary angiography, with LVEF ≤40% during gated-SPECT myocardial perfusion at rest, and in the absence of other heart disease.23 Exclusion criteria were previous coronary revascularization, cardiac pacemakers, and the presence of any other disease with poor short-term prognosis.
Design
The patients who had been assessed using gated-SPECT myocardial perfusion and fulfilled the selection criteria were given a new appointment and, after obtaining signed informed consent in each center within 10 days of the previous test, underwent gated-SPECT at rest using LDD and under uniform image acquisition protocols at each center. Image interpretation and statistical tests were conducted in the imaging unit of the coordinating center whose ethical committee had approved the study.
Gated-SPECT Using Low-Dose Dobutamine
First, a dose of 740 MBq to 925 MBq 99Tc-tetrofosmin was injected at rest, and images acquired at rest 30 min later. Next, 5 µg/kg/min dobutamine was infused over 3 min. The dobutamine dose was increased to 7.5 µg/kg/min at the same time as a second gated-SPECT24 acquisition procedure was conducted over 11 min, with continuous ECG monitoring and blood pressure checked every 3 min. Images were acquired using gamma cameras equipped with a high-resolution collimator, following a semi-circular orbit starting in the 30o right anterior oblique view with image capture every 3o until a 180o turn was completed in the left posterior oblique view. A 5th-order Butterworth filter at a cutoff frequency of 0.4 was used for image reconstruction. The images were obtained in short axis, horizontal long axis, and vertical long axis.
The LV was divided into 17 segments,25 and a score was assigned to each one according to its degree of perfusion (0 = normal perfusion; 1 = mild hypoperfusion; 2 = moderate hypoperfusion; 3 = severe hypoperfusion; and 4 = no perfusion).23 Two blinded observers made a semiquantitative analysis of each segment, assigning scores for both contractility and wall thickening (0 = normal; 1 = mild reduction; 2 = moderate reduction; 3 = severe reduction; and 4 = none).23,24
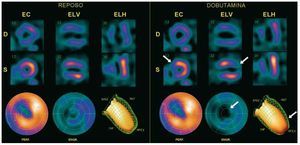
Segments were considered as viable on scintigraphy when they had a grade 3-4 contractility score and a grade 0, 1, or 2 perfusion score or when they had some baseline wall thickening or grades 0, 1, and 2 with LDD. A segment was considered contractile-reserve negative when the wall thickening score increased by ≥1 unit (Figure 1) during LDD infusion. The anterior, septal and apical segments (1, 2, 7, 8, 13, 14, 17) were assigned to the left anterior descending coronary artery (LAD); the lower segments (3, 4, 9, 10, and 15) to the right coronary artery (RCA); and the lateral segments (5, 6, 11, 12, 16) to the left circumflex artery.25
Figure 1. Gated-SPECT myocardial perfusion. Example of negative contractile reserve in the antero-septo-apical region during low-dose dobutamine (LDD) infusion. A decrease can be seen between rest (R) and LDD infusion in thickening and contractility of the antero-apical region (arrows), together with a decreased ejection fraction of 4%. ANT indicates anterior; D, diastole; EC, short axis; ELH, horizontal long axis; ELV, vertical long axis; ENGR, polar map of thickening; INF, inferior; PERF, polar map of perfusion; S, systole.
Left ventricle ejection fraction and ventricular volumes (end-systolic volume [ESV] and end-diastolic volume [EDV]) during gated-SPECT at rest and during LDD infusion were measured using quantitative gated-SPECT methodology.26 Inter-observer variability for LVEF assessed by gated-SPECT was 0.5 (2.6) points for LVEF as assessed in the imaging unit where these calculations were performed.27
Coronary Angiography
In total, 68 patients were evaluated using contrast-enhanced coronary angiography. This was performed using one of the 2 Philips systems, either the Optimus M200 (biplane) or Integris (monoplane). In all cases, a field of view of 17.8 cm was used. The observer visually assessed coronary stenosis and this assessment was confirmed by another interventional cardiologist. Significant coronary stenosis was considered present when this was >50% in any of the 3 main coronary vessels (LAD, CX, and RCA) and in the left main coronary artery. The coronary artery was considered open or non-occluded when stenosis was <100%.
Statistical Analysis
Discrete variables are expressed as percentages and continuous variables as means (standard deviation). The c2 test was used to compare 2 independent discrete variables; when the number of expected values in one or more boxes in the contingency table was <5, Fisher's exact test was used. The Student t test for independent samples was used to compare independent continuous variables; if the number of subjects was <30, the Mann-Whitney test was used. The cut-off value for the number of segments with NCR able to cause a decrease in LVEF >3% was determined by analysis of the receiver operating characteristic (ROC) curves. The association between the decrease in LVEF (dependent variable) and the number of segments with NCR (independent variable) in each coronary territory was assessed by linear regression analysis adjusted for LVEF and resting volumes, age, and sex (ENTER method). The following variables were introduced into the model: NCR of the region under study, LVEF at rest, EDV at rest, ESV at rest, age, and sex. All the variables were analyzed using the SPSS software package (SPSS, version 15, Chicago, IL, USA). A P value of <.05 was used as a cutoff for statistical significance.
RESULTS
The clinical characteristics of the 68 patients studied are shown in Table 1. No type of clinical, hemodynamic, or electrocardiographic complication was observed during LDD infusion. In total, 42.6% (29/68) of the patients presented one or more segments with NCR. The prevalence of segments with NCR during LDD infusion was 6.8% (79/1156 segments), corresponding to 6.9% (33/476) of the segments supplied by the LAD, 9.1% (31/340) of the segments supplied by the RCA, and 4.4% (15/340) of the segments supplied by the CX. All the segments with akinesia or severe hypokinesia (n=476) were segments with a grade 3-4 wall thickening score. The prevalence of NCR in these segments was 3.6% (17/476).
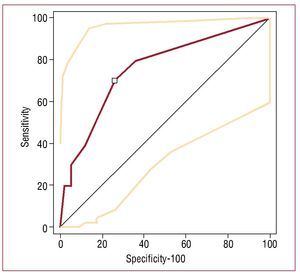
Negative Contractile Response and Overall Left Ventricular Systolic Function
The ROC curve analysis indicated a cutoff value of ≥2 segments with NCR for a 1-point decrease in LVEF ≥4% (sensitivity, 70%; confidence interval [CI], 34.8-93; specificity, 74,14% [61%-84.7%]; positive likelihood ratio = 2.71; negative likelihood ratio = 0.40) (Figure 2). During LDD infusion, 35.3% (n=24) of the patients presented an increase in LVEF <4%, and 14.7% (n=10) of the patients presented a decrease in LVEF ≥4%. No clinical differences were observed between the patients with and without a decrease in LVEF ≥4% (Table 2).
Figure 2. Determination of the cut-off value of the number of segments with negative contractile response (NCR) for a decrease in ejection fraction ≥4% by analysis of receiver operating characteristic curves.
A linear, negative and significant association (adjusted for LVEF and resting volume, age, and sex) was observed between the number of segments with NCR in the territory of the LAD (b=-1.98; 95% CI, -3.19 to -0.75; P=.002; ANOVA, F = 5.500; P<.001; r2=0.4) and the RCA (b=-1.98; 95% CI, -3.21 to -0.698; P=.003; ANOVA, F = 5.296; P<.001; r2=0.4) in relation to the decrease in LVEF.
The patients with a decreased LVEF ≥4% had a significantly greater number of segments with NCR (2.8 [2.5] vs 0.87 [0.4]; P=.042). A significant increase in ESV was observed in the patients with a decreased LVEF ≥4% during LDD infusion, as well as a greater number of patients with ≥2 segments with NCR (Table 3).
Negative Contractile Response and Viability on Scintigraphy
During LDD infusion, greater NCR was observed in patients with baseline grade 0-2 wall thickening compared to the segments with grade 3 wall thickening (16.43% vs 3.5%, respectively; difference, 16.9%; 95% CI, 5.8-20.7; c2=11.286; P<.001).
A total of 40.9% (195/476) of the segments with severely decreased wall thickening (grade 3-4) in the baseline study corresponded to segments appearing viable on scintigraphy, since they presented grade 0-2 perfusion in the baseline images (Figure 3).
Figure 3. Flow chart of the 1156 segments associated with baseline perfusion, baseline thickening and negative contractile reserve (NCR). *All the segments had a baseline thickening score of 2.
Of the 79 segments with NCR, 17 (21.5%) corresponded to segments with akinesia or severe hypokinesia, in which viability had to be studied. In total, 70.6% (12/17) of these were viable according to a perfusion score ranging from 0 to 2. The remaining 62 segments with NCR were located in regions which did not undergo a myocardial viability assessment, since under baseline conditions they presented normal perfusion or thickening or a mild-to-moderate decrease. Thus, 93.7% (74/79) of the segments with NCR were associated with live myocardium (normal or viable), since only 6.3% (5/79) of the segments with NCR had scintigraphic signs of necrosis, defined as grade 4 perfusion plus grade 3-4 wall thickening (Figure 3).
Negative Contractile Response and Coronary Angiography
In total, 22.1% (15/68) of LAD presented ostial or proximal occlusion and 10.3% (7/68), medial or distal occlusion. Some 64.5% (21/33) of the anteroseptal segments with NCR were supplied by a patent LAD. Of the RCA segments, 10.3% (7/68) presented ostial or proximal occlusions and 10.3% (7/68) medial or distal occlusions. Some 87% (27/31) of the segments with NCR were supplied by a patent RCA, and 2.9% (2/68) of CX presented ostial or proximal occlusions and 5.9% (4/68) presented medial or distal occlusions. The CX was patent in 100% (15/15) of the segments with NCR in territories supplied by this artery.
Of the 12 viable segments with NCR, 83.3% (10/12) were associated with a patent coronary artery; 3 were in the territory of the LAD (all supplied by a patent artery), 7 in the territory of the RCA (5 with a patent artery), and 2 in the territory of the CX (both with a patent artery).
DISCUSSION
The segmental analysis of systolic thickening and left ventricular segmental contractility is complex. Generally, contractile reserve—segmentary or overall—is assessed during dobutamine infusion and it can be observed that some segments can respond with an increase, a decrease, or no change in wall thickening.24 To date, echocardiographic,1-9 nuclear cardiology,6-18 and magnetic resonance imaging studies19-20 have highlighted positive contractile reserve as a synonym of myocardial viability. On the other hand, the significance of a deterioration in segmental systolic function or NCR due to an inotropic stimulus, which can significantly influence the decrease in LVEF, has received little attention.
This study investigated NCR in a population of patients with IC using gated-SPECT at rest to assess myocardial viability for medical reasons. The first and striking finding was that the prevalence of patients with 1 or more segments with NCR was 42.6%. Overall, 6.8% of the segments presented this type of response, a similar percentage to that reported in an echocardiography study.17
In 14.7% of patients, LVEF decreased by ≥4%, a lower percentage than that found in other series (26%-31.2%), although these studies included patients with LVEF >50%.1,12 The patients with a decrease in LVEF of this magnitude were characterized by having more segments with NCR and a greater increase in end-systolic volume.
Another important finding to bear in mind is that the majority of the segments with NCR (93.6%) were in live myocardium (normal or viable on scintigraphy). On the other hand, most of the segments with akinesia or severe hypokinesia and NCR appeared viable on scintigraphy and were supplied by a patent coronary artery. The response of the cardiac muscle to an inotropic stimulus is due to a combination of different mechanisms; for example, parietal stress, the tethering effect,28 high-energy phosphate concentrations, the number of normal segments that surround the area with changes in contractility,29 and receptor response.30 However, the mechanisms with the greatest influence on the negative response are parietal stress, the tethering effect and intracellular high-energy phosphate concentrations.
The NCR mechanisms underlying the segments assessed via LDD-SPECT imaging in our series may not be the same as those which induce NCR using high-dose dobutamine (biphasic response) in echocardiographic studies, since the negative component of the biphasic contractile response may be caused by ischemia during high-dose dobutamine infusion.29 Despite this, both responses are negative and have an impact on ventricular function.
Positron emission tomography (PET) studies have shown that the contractile response is always lower in segments with severe perfusion abnormalities at baseline.31 Our results show that the prevalence of NCR is also slightly lower when there are severe perfusion abnormalities on baseline SPECT imaging. These observations may indicate that as myocardial damage increases, a contractile response, whether positive (improvement) or negative (deterioration), is less likely.
Another relevant finding of this study is the association between segments with NCR and the patency of their respective coronary artery. Although TIMI flow and collateral circulation grades were not assessed, the fact that the majority of the segments did not have severely compromised wall thickening at baseline plus the presence of a patent coronary artery could be an indirect indicator of persistent coronary flow and myocardial viability.
Limitations
The number of patients included in this series was low, but it should be borne in mind that the number of patients with IC who undergo LDD gated-SPECT at rest for medical reasons in a single center is limited. For this reason, 8 hospitals participated and followed the same methodology. To keep inter-observer variation in interpreting the results to the minimum, all images were analyzed in a centralized imaging unit.
The criterion for a decrease in LVEF ≥4% may seem arbitrary, but was this was agreed on after analyzing the best cutoff point on ROC curves, as described. This cutoff point appears to be clinically relevant and is similar to the one used in other series.12,27
The lack of data on the collateral circulation, distal bed and TIMI flow grade is a limitation of the present study, since this data could have contributed additional information to the complex interpretation of the effect of LDD infusion. In any case, Barilla et al32 found that the recovery of contractility of dysfunctional viable myocardium supplied by occluded arteries during inotropic stimulation with LDD does not depend on increased coronary blood flow, and even occurs in the absence of collateral circulation.
This study does not provide data on exercise SPECT, which would have provided information on the possible presence of ischemia using LDD in the segments with NCR. However, Melon et al33 have already demonstrated that the infusion of 10 µg/ kg/min dobutamine can cause ischemia in regions irrigated by severely stenotic arteries.
It should also be highlighted that the low number of patients (n=10) in one of the groups could have led to extreme and nonrobust results, and so they should be verified with a larger number of patients.
CONCLUSIONS
A negative contractile reserve on gated-SPECT at rest using LDD was not uncommon in patients with IC and was associated with a decrease in overall LV systolic function. It was mainly observed in segments meeting scintigraphic criteria of viability and that were supplied by a patent coronary artery. The majority of the segments with severe contractile dysfunction and NCR appeared viable on scintigraphy and were supplied by patent coronary arteries.
RECAVA RESEARCHERS (RED TEMáTICA DE ENFERMEDADES CARDIOVASCULARES)
Gustavo de León,a Joan Castell-Conesa.b Hospital Universitari Vall d'Hebron, Barcelona, Spain.
Martín de la Fuente,a Juan José Martínez Sampere.b Hospital Clínico Universitario San Cecilio, Granada, Spain.
Maximiliano Diego Domínguez,a Ricardo Ruano.b Hospital Universitario, Salamanca, Spain.
José Alfonso Jurado López,a María Jesús Pérez Castejón.b Instituto de Cardiología, Madrid, Spain.
Jordi Magriñá Ballará,a M. África Muxí Pradas.b Hospital Clínic, Barcelona, Spain.
Carlos Peña Gil,a Virginia Pubul Núñez.b Complejo Universitario Hospitalario, Santiago de Compostela. A Coruña, Spain.
José Antonio Ferrero Cabedo,a Irene Casáns Tormo.b Hospital Clínico, Valencia, Spain.
Miguel Hartáiz Urdaci,a María José García Velloso.b Clínica Universitaria de Navarra, Pamplona, Navarra, Spain.
aServicio de Cardiología.
bServicio de Medicina Nuclear.
ABBREVIATIONS
CX: left circumflex artery
EF: ejection fraction
IC: ischemic cardiomyopathy
LAD: left anterior descending artery
LDD: low-dose dobutamine
LV: left ventricle
NCR: negative contractile response
RCA: right coronary artery
SPECT: single-photon emission computed tomography
This study was partially financed by the Redes temáticas de enfermedades Cardiovasculares, Instituto Carlos III (Red C03/01, RECAVA).
Correspondence: Dr. J. Candell-Riera.
Servicio de Cardiología. Hospital Universitari Vall d'Hebron. Universitat Autònoma de Barcelona.
Pg. Vall d'Hebron, 119-129. 08035 Barcelona. Spain.
E-mail: jcandell@vhebron.net
Received December 18, 2008.
Accepted for publication November 11, 2009.