Keywords
INTRODUCTION
Diabetes mellitus (DM) is among the diseases with the greatest public health impact in Spain. It's high prevalence and the cardiovascular complications with which it is associated make it a problem of great concern.1,2
Over the last 20 years there has been a spectacular increase in the number of overweight people with DM in Western countries, a phenomenon that has been largely attributed to changes in lifestyle. It is now estimated that some 10%-15% of the Spanish population is diabetic. More than 90% of those afflicted have type 2 DM (DM2), the incidence of which has now reached 10 cases per year per 1000 people. These figures suggest that the number of diabetics in Spain will double over the next 25 years.3,4
The risk of cardiovascular disease (CVD) in adult diabetics is 4 times higher than in the general population of the same age,5 and together, ischemic heart disease and cerebrovascular disease account for more than 70% of mortality in such patients.
The influence of sex on cardiovascular disease is of great interest. Many studies have shown there to be sex-related differences in the prevalence, symptomatic presentation, and management of cardiovascular disease, as well as in patient prognosis.6 Indeed, in Spain there is worrying data that suggests that mortality is greater among women hospitalized for their first acute myocardial infarction.7 Certainly, one of the most controversial medical topics of the last decade has been the influence of sex on morbidity/ mortality in diabetic patients. At the end of the 1990s an analysis of the NHANES I (First National Health and Nutrition Examination Survey)8 registry led to a report suggesting that coronary death was becoming more common among women diabetics but less common in their male counterparts. Findings such as this led to several meta-analyses being performed, some of which confirmed the poorer prognosis of women both in terms of morbidity and mortality.9 Others, however, contradicted this.10,11
Clinical information on the influence of sex on the prognosis of Spanish diabetic patients is practically non-existent, a situation that justifies the undertaking of prospective studies designed to determine what this influence might be. The present study focuses on a single population from Galicia (NW Spain).
The prospective Barbanza Diabetes12,13 study was designed to determine the characteristics, cardiovascular risk factors and the clinical course of patients with DM treated by primary care physicians, as well as the adherence to clinical practice guidelines. The aim of this subanalysis was to determine the influence of sex on the appearance of cardiovascular complications (death and/or hospitalization due to cardiovascular causes) during the follow-up period.
METHODS
Study Protocol
The characteristics of the patients in this multi-center, prospective cohort study have been described elsewhere.12,13 The researchers involved were 31 primary care physicians belonging to 10 health centers in the southeast of the Province of A Coruña (Galicia, NW Spain). A total of 1423 consecutive patients who came for consultation over a period of 2 months in 2002 were recruited. All met the inclusion criteria of: age over 18 years, having a previous diagnosis of DM,14 and providing consent to be included. No rejection of inclusion was recorded. A prospective follow-up period of 4 years was programmed, with 3 intermediate visits for the monitoring of risk factors and treatment. During this period 109 patients were lost to follow-up, 26 because of a change of address, and 83 because of a change of workplace by 2 of the physicians involved.
After the recording of data an internal audit was undertaken to guarantee its quality. This involved the random selection of 10 of the participating physicians (one per health center), and the review of the clinical histories produced. All data were found to be perfectly recorded.
Variables Analyzed
All patients were subjected to anamnesis, physical exploration and biochemical tests and electrocardiographic monitoring. Their main demographic, anthropometric and clinical details were recorded, along with the treatment they received.
Patients with a body mass index (BMI) of ≥30 were considered obese. The recorded blood pressure was measured on the day of inclusion, using a tested and calibrated sphygmomanometer; readings were taken after a resting period of 5 min, and then again after another 5 min had elapsed. The mean was then calculated and recorded. A well controlled blood pressure was regarded as a value of <130/80 mm Hg. Acceptable values for baseline fasting glycemia and glycohemoglobin were considered to be <126 mg/dL and <7%, respectively. A triglyceride concentration of <150 mg/dL, a total cholesterol level of <180 mg/ dL, a low density lipoprotein cholesterol (LDL-C) level of <100 mg/dL, and a high density lipoprotein cholesterol (HDL-C) level of >40 mg/dL in men and >50 mg/dL in women15 were considered well controlled. Albuminuria was considered above values of 30 mg/dL/24 h.
The patients were grouped depending on whether or not they suffered CVD before their inclusion in the study. Cardiovascular disease was deemed present in those previously diagnosed with angina, myocardial infarction, ictus, intermittent claudication or aneurysm of the abdominal aorta, and in those who had suffered a transitory ischemic attack. Those who had undergone a percutaneous and/or surgical arterial revascularization (coronary, carotid, or of the peripheral arteries of the leg), and those who had been subjected to surgery on the abdominal aorta were also deemed to suffer CVD.
After 4 years of follow-up, the mortality (and the corresponding causes of death) and morbidity (hospitalizations and their causes during the study period) data were examined. The cause of death was obtained from death certificates; reasons for hospitalization were obtained from discharge documents. Both types of document were available in the clinical histories of the patients at the corresponding health centers.
Statistical Analysis
Qualitative variables were expressed in terms of absolute frequencies and percentages, while qualitative variables were expressed as means (standard deviation) or medians and the interquartile range, depending upon whether their distribution was normal. Differences between the means of parametric variables were analyzed using the Student t test for independent samples. The Mann Whitney U test was used to compare the means of non-parametric variables. A descriptive statistical study of the categorical variables was made using frequency tables; the Pearson c2 test was used to determine the significance of associations between qualtitative variables.
The probability of survival during follow-up was determined using the Kaplan-Meier test. The logarithmic rank test was used to compare the curves of different subgroups. Cardiovascular events (death or hospitalization) were subjected to univariate analysis and the variables found to be significant were included in a Cox multivariate analysis using the conditional forward stepwise method. The variables that remained significant (age, high blood pressure [HBP], BMI, albuminuria, prior CVD, and treatment with diuretics, angiotensin converting enzyme inhibitors [ACE inhibitors] or angiotensin II receptor antagonists [ARA-II]) were those used to adjust the Cox model; the results are expressed as hazard ratios (HR) plus 95% confidence intervals (95% CI).
All calculations were performed using SPSS v.14.0 software for Windows. Differences with a type 1 probability error of <5% were considered significant. It was estimated that to detect differences of >5% in the mortality of men and women, and for a power of 90%, a minimum of 621 patients would be required in each group.
RESULTS
Characteristics of the Study Population
A total of 1423 diabetic patients were recruited, of whom 7.9% had type 1 diabetes (DM1) (5.1% of the men and 10.6% of the women). Table 1 shows the characteristics of the patients by sex. The sample was well balanced, with 49.7% men (n=707) and 50.3% women (n=716). The mean age was 66 years (range, 18-97 years); the women, however, were significantly older. Some 64% of patients had HBP, 70% had dyslipidemia, and more than half had some form of CVD or target organ damage.
Except for smoking, all risk factors for CVD were more common among the women patients. Table 1, however, shows the distribution of CVD and albuminuria according to sex; CVD (especially ischemic heart disease) was more common among the men. In addition, men more often had target organ damage.
Table 1 shows that a greater percentage of women received ACE inhibitors and/or ARA-II and diuretics than men, and more were treated with insulin.
No differences were seen in the number of medications used for the control of diabetes between the men and women: only 1 diabetes medication in 72.7% of men and 72.4% of women, and 3 or more in just 2.7% of men and 4.5% of women. A strong correlation was seen between HBP and treatment with diuretics (supplied to 29.1% of hypertensive patients but only 4.8% of non-hypertensive patients; P<.001). This relationship was even stronger among the women patients; diuretics were supplied to 34.9% of hypertensive and to 6.3% of normotensive female patients.
Table 2 shows that blood pressure was well controlled in only 14% of the hypertensive patients. Baseline glycemia was adequate in only 22% of the entire cohort. The women patients showed poorer glycemic control (expressed in terms of the glycohemoglobin concentration), higher total cholesterol levels, and lower HDL-C levels than the men.
Morbidity and Mortality
After a mean follow-up time of 44.6 (10.2) months (median, 48.1 months), total mortality was 6.2%. Some 49% of all deaths had a cardiovascular cause. The general rate of hospitalization was 30%. Table 3 shows the mortality and hospitalization rates and their causes for the patients as a whole and by sex.
No difference was seen between the men and women patients in terms of mortality, either in general or by its cause. The actuarial probability of survival at 4 years was 93.8% for the patients as a whole.
In multivariate analysis, age, CVD, albuminuria, and treatment with diuretics were all independent predictors of morbidity/mortality; these variables remained independent predictors after adjustment for sex.
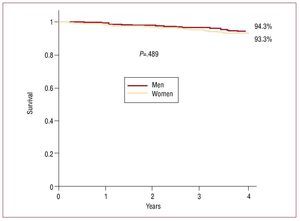
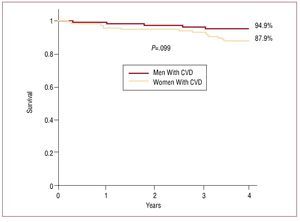
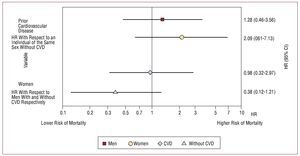
The Kaplan-Meier curves of Figure 1 showed there to be no difference between the sexes with respect to the probability of survival (log-rank test, P=.489). Among the women patients, greater mortality was seen when CVD was present (log rank test, P=.009), but this was not maintained when adjustments were made for other variables (Figures 3 and 4). Neither were any differences seen between men and women patients when cardiovascular death and hospitalizations were combined (Tables 5 and 6).
Figure 1. Probability of survival of the patients in the Barbanza Diabetes study; distribution by sex. Univariate analysis.
Figure 2. Probability of survival of the women in the Barbanza Diabetes study, depending on the presence of prior cardiovascular disease. Univariate analysis. CVD indicates cardiovascular disease.
Figure 3. Risk of cardiovascular events (death and/or hospitalization) of patients adjusted for age, high blood pressure, body mass index, albuminuria, and the use of diuretics, beta-blockers, angiotensin II receptor antagonists, and angiotensin converting enzyme inhibitors. CI indicates confidence interval; CVD, cardiovascular disease; HR, hazard ratio.
Figure 4. Risk of death due to cardiovascular causes, adjusted for age, high blood pressure, body mass index, albuminuria, and the use of diuretics, beta-blockers, angiotensin II receptor antagonists, and angiotensin converting enzyme inhibitors. CI indicates confidence interval; CVD, cardiovascular disease; HR, hazard ratio.
DISCUSSION
The present work, which involved a large, non-selected cohort of diabetic patients whose members were followed prospectively by primary care physicians, showed that, during the study period, the risk of suffering a cardiovascular complication (death and/or hospitalization owing to a cardiovascular cause) was not influenced by sex.
This large group of patients reflected the expected characteristics of a coastal population from the Galicia region of Spain, ie, a high prevalence of HBP, high salt consumption, and a greater incidence of ictus than that seen in other Spanish regions.16 According to Galician Health Service data, the annual rate of death due to acute myocardial infarction among the present patients was higher than among the general population (152.2 vs 47.3 per 100 000 people). They were, however, similar for death owing to ictus (76.1 vs 78.4 per 100 000 people).
To our knowledge, an earlier paper arising from the Barbanza Diabetes study was the first to describe the mid-term prognosis of a homogenous cohort of diabetic patients with and without clinical CVD in Spain.16 Other reports have referred to the incidence of CVD in diabetic patients, such as that of Tomás et al17 in the Manresa study, which involved a 28-year follow-up period - but this only included men (n=1050). The work of Rius et al18 is also available, but this involved only a small number of patients and provided few data on mortality. Cañón-Barroso et al19 retrospectively identified (in a general medicine clinic) a larger cohort of patients with DM2 who initially did not suffer CVD (n=190); these authors observed a cumulative incidence of coronary heart disease (angina, mortal or non-mortal acute myocardial infarction) at 10 years of 14.7% (13.3% in men and 16% in women). However, the present work is one of the first to be performed in Spain that shows a similar prognosis for diabetic men and women in terms of mortality and cardiovascular events.
A number of studies have examined the cardiovascular risk faced by diabetics according to their sex, but have returned very heterogeneous results. The majority of these studies focused on the relationship between DM and ischemic heart disease. Although the follow-up times and sample sizes of these studies were very different, some report the relationship to be stronger in women than in men.9,10,20-22 This would appear to indicate that suffering diabetes reduces the sex-related difference in the normally expected probability of developing coronary heart disease and associated mortality. However, many of these studies also varied with respect to the adjustment for important confounding factors, and, in fact, some of the meta-analyses among them included many reports in which no data for women were available. Further, the influence of already established CVD was often not taken into account in the analysis of the risk of future ischemic events. A less favorable cardiovascular risk profile in diabetic women9,23 plus less effective strategies for this group9 have been put forward as explanations for sex-related differences in the influence of diabetes on coronary mortality.23
It should also be remembered that the above meta-analyses have returned variable results, reporting opposite effects for the influence of sex.2,9-10 One analysis2 even affirms that patients without DM who had suffered a myocardial infarction, and those with DM in isolation, were just as likely to suffer a cardiovascular event in the future (as reported earlier by Haffner et al24) and indeed that this correlation was stronger in women. A recent epidemiological study of three million Danish citizens25 confirmed the affirmation of Haffner et al in similar patients (those with DM treated pharmacologically) over 30 years of age. However, no sex-related differences were seen among the diabetic patients with respect to prognosis. This same study confirmed the additive effect on prognosis of a prior infarction and DM. This was also highlighted in other studies such as that of Dale et al.26 The latter authors indicated patients with DM who had suffered a prior infarction have a poorer prognosis, although they reported no differences with respect to sex. This lack of a sex difference is controversial since other works7,11,20,27 report DM plus associated prior coronary heart disease to have a major impact on prognosis in women.
In the present study, one of the reasons why sex appeared to have no effect is very likely because the percentage of diabetic women with prior coronary heart disease was lower than in the men (9.8% vs 16.4%; P=.002). In addition, the survival of the women with prior ischemic heart disease and those with no such history was similar (89.36 vs 93.67%; P=.2639).
Also, the extent of treatment and monitoring might influence prognosis among the female population. The under-use of medications recommended by clinical guidelines was greater in women than men. Further, the reduced efficacy of their active agents in women that has been described by some authors,6,28,29 meaning the degree of control required to achieve an improvement in mortality, may not have been reached. These sex-related differences in treatment are reflected in the national-scale ESPERANZA30 study, which showed a lower percentage of diabetic women than men were prescribed antiaggregation and lipid lowering medication; no differences were seen with respect to other pharmacological agents. In the present study, antiaggregants were also less often prescribed to women, although there were fewer women than men with coronary heart disease. In contrast, lipid lowering drugs were prescribed equally to both sexes. It is curious that, in the present patients, the control achieved over serum lipids (total cholesterol and HDL-C) in the women was not as good as in the men. Women also had higher glycohemoglobin levels than the men (although this did not influence prognosis).
As reported in other studies,11,26,27 the present diabetic women showed a greater accumulation of risk factors and were older than the male patients. This finding can be used to try to explain the poorer prognosis of the women. However, more of the present men were smokers (an important risk factor for ischemic heart disease), and more had CVD with the involvement of a target organ, which may have compensated for the women's greater accumulation of risk factors. It should be noted that, in the present work, greater age, having CVD, the presence for albuminuria and treatment with diuretics were independent determinants of morbidity/mortality. The first three are factors that are identified in nearly all registries of patients with CVD; the fourth probably reflects the influence of heart failure and the need for a greater number of medications to control more serious problems of HBP.
The value of albuminuria as a prognostic factor is known from a sub-study of the Heart Outcomes Prevention Evaluation (HOPE)31 trial, in which it was shown to be associated with an almost doubling of the mortality rate of that seen when the urine albumin level was normal. The literature contains multiple references that support this.32
Limitations of the Study
The loss to follow-up of over 7% of the study population may have had some influence on the results, although this loss rate is similar to that recorded in other population registries of patients with CVD. It should also be remembered that the present work was limited to a follow-up period of 4 years; further monitoring is needed to determine whether the findings reported here hold in the long term.
Changes in the therapeutic strategy followed during the study period were not recorded for the majority of patients. In addition to the initial treatment, any such changes may have had some influence on patient prognosis; this, however, is a limitation faced by nearly all registries.
It is possible that some patients may have suffered a cardiovascular complication during follow-up that did not require hospitalization; this may have led to an underestimation of the cardiovascular risk faced by the study population.
It is also possible that mortality was underestimated in the present study since some of the patients lost to follow-up may have died.
The study suffers from a methodological limitation regarding a lack of knowledge of the duration of the patients' DM. No data on this were recorded for the majority of patients, although it is likely that this was similar in both sexes. Had such data been available it may have influenced the results, since it is known that the effect of DM on cardiovascular mortality is greater with time. Some authors suggest this effect is more pronounced in women.33
Finally, this work involved a registry in which the different attending physicians made and recorded the diagnosis of DM, identified other risk factors, recorded the presence of concomitant CVD, and noted the treatment provided and the cardiovascular complications that occurred during follow-up. This might also be understood as a factor increasing the work's quality.
CONCLUSIONS
In the present study, no mid-term differences were observed with respect to cardiovascular morbidity or mortality in diabetic men and women from a single geographical area—despite their clinical differences and the different therapeutic strategies followed. This work reflects, for the first time in a group of Spanish diabetics, the influence of sex on prognosis and its determinants. The lack of difference in the prognosis of patients of either sex provides support for the therapeutic strategies currently followed in northwestern Spain—which are no different for men and women—aimed at reducing the risk of cardiovascular disease in diabetic patients.
RESEARCHERS OF THE BARBANZA GROUP
J.M. Fernández-Villaverde, G. Allut-Vidal, J. Domínguez-López, J.L. Gómez-Vázquez, P. de Blas-Abad, C. Pastor-Benavent, A. Fernández-Seoane, J. Maestro-Saavedra, M.J. Alvear-García, Pérez-Llamas, R. Besada-Gesto, J.A. Santos-Rodríguez, M. Lado-López, V. Turrado-Turrado, Vaamonde-Mosquera, A. Lado-Llerena, M.A. Juiz-Crespo, M. Sánchez-Loureiro, E. Rodríguez-Moldes, J. Dopico-Pita, G. Gutiérrez-Fernández, J. Torres-Colomer, R. Blanco-Rodríguez, and A. Nores-Lorenzo.
ABBREVIATIONS
ACE inhibitors: angiotensin converting enzyme inhibitors
ARA-II: angiotensin II receptor antagonists
CVD: cardiovascular disease
DM: diabetes mellitus
HBP: high blood pressure
HR: hazard ratio
A full list of the Barbanza Group researchers is included at the end of this article.
Correspondence: Dr. J.R. González-Juanatey.
Servicio de Cardiología. Hospital Clínico.
Travesía Choupana, s/n. 15706 Santiago de Compostela. A Coruña. Spain.
E-mail: jose.ramon.gonzalez.juanatey@sergas.es
Received December 12, 2008.
Accepted for publication October 19, 2009.