Obesity is a vascular risk factor implicated in the pathogenesis of type 2 diabetes mellitus (DM2). There has been some debate about whether obesity in patients with DM2 is associated with greater1 or less2 mortality with respect to patients of normal weight with DM2 (the obesity paradox in DM2). In principle, the association between body mass index (BMI) and mortality could be mediated by vascular risk factors, target organ lesions, and vascular events, although we are not aware of studies that have investigated these variables in patients with DM2 and different BMIs. We compared the frequency of vascular events and their associated factors in obese patients with DM2 and those of normal weight with DM2.
This was an observational study conducted in the outpatient clinic of the Metabolic-Vascular Unit of La Paz University Hospital, Madrid, Spain in 2013. We selected all patients with DM2 (according to the American Diabetes Association criteria) attended at least once in the calendar year with a full clinical work-up. Patients had to have a BMI of 30 kg/m2 or more (obesity) or less than 25kg/m2 (normal weight). Weight and height were measured during the first appointment of the year using a height rod and digital scales, calibrated every 6 months (AENOR quality control, UNE-EN ISO 9001 standard). Height was measured to the nearest centimeter and weight was measured in kilograms to 1 decimal place, with the patient wearing no coat, jacket, or shoes. We recorded demographic variables, vascular risk factors, target organ lesions, cardiovascular events, laboratory data, and DM-related treatments, according to the criteria defined in the REACH study,3 which included patients from Spain. Glomerular filtration rate was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
For qualitative variables, the 2 groups, obese and normal-weight patients, were compared with the Pearson chi-square test using a continuity correction or the Fisher exact test when the number of measurements in the sample was small. The Student t test for independent samples was used for quantitative variables. The relationship between events in the 2 BMI groups, adjusted for age, sex, smoking, and blood pressure, was studied with binomial logistic regression. P < .05 was considered statistically significant.
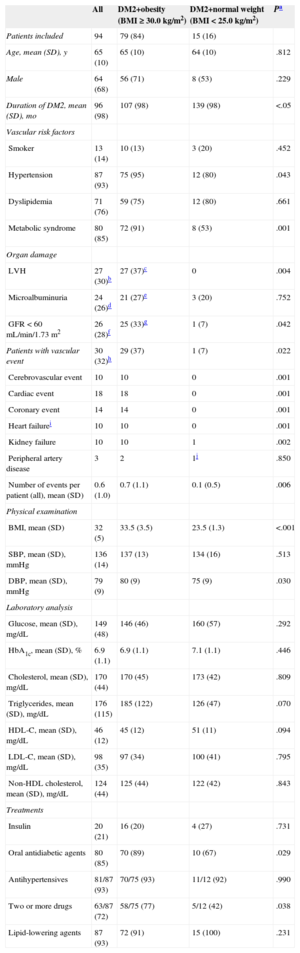
Overall, 94 patients with DM2 were included: 79 with BMI of 30kg/m2 or more and 15 with BMI less than 25kg/m2 (Table). The number of patients with at least 1 vascular event was significantly higher among obese patients (n = 29 [37%]) compared with normal-weight patients (n = 1 [7%], P = .032). Most of the vascular events affected the heart (ischemic heart disease or heart failure, 18/30 patients [60%]). On multivariate analysis, the association between obesity and vascular events remained significant (P = .035). Despite a shorter duration of diabetes (P < .05), a greater proportion of obese patients had hypertension (P = .043) than normal-weight patients. A greater proportion of obese patients had left ventricular hypertrophy (P = .004), metabolic syndrome, and chronic stage III renal failure (glomerular filtration rate of 30-60mL/min/1.73 m2; P = .042).
Characteristics of Obese and Normal-Weight Patients With Type 2 Diabetes Mellitus
| All | DM2+obesity (BMI ≥ 30.0 kg/m2) | DM2+normal weight (BMI < 25.0 kg/m2) | Pa | |
|---|---|---|---|---|
| Patients included | 94 | 79 (84) | 15 (16) | |
| Age, mean (SD), y | 65 (10) | 65 (10) | 64 (10) | .812 |
| Male | 64 (68) | 56 (71) | 8 (53) | .229 |
| Duration of DM2, mean (SD), mo | 96 (98) | 107 (98) | 139 (98) | <.05 |
| Vascular risk factors | ||||
| Smoker | 13 (14) | 10 (13) | 3 (20) | .452 |
| Hypertension | 87 (93) | 75 (95) | 12 (80) | .043 |
| Dyslipidemia | 71 (76) | 59 (75) | 12 (80) | .661 |
| Metabolic syndrome | 80 (85) | 72 (91) | 8 (53) | .001 |
| Organ damage | ||||
| LVH | 27 (30)b | 27 (37)c | 0 | .004 |
| Microalbuminuria | 24 (26)d | 21 (27)e | 3 (20) | .752 |
| GFR < 60 mL/min/1.73 m2 | 26 (28)f | 25 (33)g | 1 (7) | .042 |
| Patients with vascular event | 30 (32)h | 29 (37) | 1 (7) | .022 |
| Cerebrovascular event | 10 | 10 | 0 | .001 |
| Cardiac event | 18 | 18 | 0 | .001 |
| Coronary event | 14 | 14 | 0 | .001 |
| Heart failurei | 10 | 10 | 0 | .001 |
| Kidney failure | 10 | 10 | 1 | .002 |
| Peripheral artery disease | 3 | 2 | 1j | .850 |
| Number of events per patient (all), mean (SD) | 0.6 (1.0) | 0.7 (1.1) | 0.1 (0.5) | .006 |
| Physical examination | ||||
| BMI, mean (SD) | 32 (5) | 33.5 (3.5) | 23.5 (1.3) | <.001 |
| SBP, mean (SD), mmHg | 136 (14) | 137 (13) | 134 (16) | .513 |
| DBP, mean (SD), mmHg | 79 (9) | 80 (9) | 75 (9) | .030 |
| Laboratory analysis | ||||
| Glucose, mean (SD), mg/dL | 149 (48) | 146 (46) | 160 (57) | .292 |
| HbA1c, mean (SD), % | 6.9 (1.1) | 6.9 (1.1) | 7.1 (1.1) | .446 |
| Cholesterol, mean (SD), mg/dL | 170 (44) | 170 (45) | 173 (42) | .809 |
| Triglycerides, mean (SD), mg/dL | 176 (115) | 185 (122) | 126 (47) | .070 |
| HDL-C, mean (SD), mg/dL | 46 (12) | 45 (12) | 51 (11) | .094 |
| LDL-C, mean (SD), mg/dL | 98 (35) | 97 (34) | 100 (41) | .795 |
| Non-HDL cholesterol, mean (SD), mg/dL | 124 (44) | 125 (44) | 122 (42) | .843 |
| Treatments | ||||
| Insulin | 20 (21) | 16 (20) | 4 (27) | .731 |
| Oral antidiabetic agents | 80 (85) | 70 (89) | 10 (67) | .029 |
| Antihypertensives | 81/87 (93) | 70/75 (93) | 11/12 (92) | .990 |
| Two or more drugs | 63/87 (72) | 58/75 (77) | 5/12 (42) | .038 |
| Lipid-lowering agents | 87 (93) | 72 (91) | 15 (100) | .231 |
BMI, body mass index; DBP, diastolic blood pressure; DM2, type 2 diabetes mellitus; GFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LVH, left ventricular hypertrophy; SBP, systolic blood pressure.
In the study, obese patients with DM2 had a higher frequency of vascular events than normal-weight patients with DM2, as well as a higher frequency of hypertension and target organ lesions. In more than half the patients with a vascular event, the heart was affected (60%) and all these patients were obese. The association between obesity and vascular events was maintained in the multivariate analysis. This finding does not support the concept of the obesity paradox in DM21,2 (apparent benefit of obesity). The study was designed to verify whether the worse prognosis of obese patients with DM2 compared with patients with normal weight1 was associated with a greater frequency of risk factors, organ damage, and vascular events. As such, the results cannot be extrapolated to all patients with DM2, given that this was not a population-based sample.
Among the study strengths, we highlight that the diagnosis of DM2 and target organ involvement, as well as assessment of the vascular events, were assessed by the same team, based on written medical records according to accepted criteria.3 Moreover, the characteristics of our series are very similar to those of other populations from different autonomous regions of Spain (mean age, 67 years; frequency of vascular events, 32%).4–6 Among the study limitations, we should highlight that we analyzed a case series, with all patients available in the clinic during 1 year. Despite the small sample size, the results help to stress that obesity in patients with diabetes is associated with vascular events and that these may be associated with hypertension and its complications, especially in the case of cardiac events.
FUNDINGHealth Research Grant from the Instituto de Salud Carlos III (FIS, 08/0009 and 11/0598), and the Spanish Primary Care Network (2009/70) and RECAVA (RD/12/0042/0024).