Heart transplant (HT) is the treatment of choice for patients with advanced heart failure, with outcomes of significantly improved life expectancy and quality of life. The main limitation is the lack of donors, which justifies the adoption of exceptional measures to make greater use of the organs available.
The first recipient was a 58-year-old man with a diagnosis of idiopathic dilated cardiomyopathy with refractory cardiogenic shock, who had received a Levitronix CentriMag left ventricular assist device as a bridge to transplant. The patient subsequently woke up and was extubated; HT was performed at 26 days postimplant and with a national priority status. The original donor was a 34-year-old man with no cardiovascular history, who died from a subarachnoid hemorrhage secondary to a ruptured cerebral aneurism. The patient had been in intensive care for 48hours, was hemodynamically stable, requiring noradrenaline infusion at 0.5 μg/kg/min, and had a normal echocardiogram.
There were no complications of note during the HT. The ischemia time of the organ was 205minutes. At 48hours, the patient did not wake up, and brain computed tomography showed a massive ischemic stroke that led to brain death at 6 days post-HT. The patient maintained an excellent hemodynamic status, with no arrhythmias, and was able to be weaned off isoproterenol on the third day with normal graft function on echocardiogram.
The second recipient was a 62-year-old man, who had been on the HT waiting list for 14 months due to ischemic dilated cardiomyopathy. He had undergone previous surgical revascularization and was inotrope-dependent (INTERMACS 3) on home treatment with intravenous milrinone. Echocardiography showed severe biventricular dysfunction and an apical mural thrombus.
A second transplant of the same organ was proposed after confirmation of the brain death of the first recipient on 2 consecutive electroencephalograms at 6 days post-transplant. The recipient was informed of the unusual origin of the donor organ and gave his consent. The hospital ethics committee approved the procedure. The implantation technique used was biatrial anastomosis, which is the standard practice in our hospital. The ischemia time was 50minutes, and the extracorporeal circulation time was 75minutes. Epicardial biopsy of the graft ruled out significant acute cellular rejection.
The recipient was treated with intravenous methylprednisolone intraoperatively, basiliximab as induction immunosuppression, and cyclosporine, mycophenolate mofetil, and prednisone as maintenance immunosuppression.
The patient progressed favorably in the immediate postoperative period, with early extubation and a 48-hour stay in the surgical intensive care unit. Subsequent complications of note consisted of prolonged symptomatic sinus node dysfunction for more than 2 weeks, requiring implantation of a dual chamber pacemaker, and symptomatic infection with cytomegalovirus, treated with valganciclovir.
Endomyocardial biopsies taken at 14, 30, 60, and 90 days after transplant ruled out significant acute cellular rejection, and the patient remained asymptomatic at 4 months post-HT.
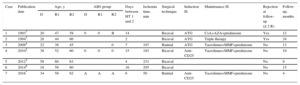
The case described is the first published case in Spain, and the seventh in the world, of reuse of a transplanted heart in a second recipient. The lack of donors, both in Spain and worldwide, has contributed to the progressive expansion of donor criteria, and nowadays transplantation frequently involves organs that would traditionally have been considered “suboptimal”, such as those coming from older donors.1
Ischemic or hemorrhagic stroke is a rare complication in the postoperative period in HT recipients, but, exceptionally, it can cause brain death, making the recipient a potential donor.
The potential disadvantages of reusing a transplanted heart include ethical, immunological, and technical aspects (for example less tissue available for anastomosis), as well as factors inherent to the cumulative ischemia time and a second reperfusion injury. Some authors postulate that the immune response of the second recipient is greater when the graft has been exposed to 2 different donors. In contrast, other authors believe that organ pretreatment with immunosuppressive drugs may reduce its immunogenicity, decrease the incidence of cellular rejection, and even prolong survival.2
To date, there have been 6 published cases of reusing a transplanted heart (Table), with favorable outcomes in all cases at mid-term follow-up (10 months to 2 years).2–7 One patient died at 10 months from leukemia. Obviously, we cannot exclude the possibility of bias toward the publication of successful cases. The maximum time between the first and second transplant in all cases was less than 16 days. The reuse of an older transplanted organ could have negative implications due to greater tissue adherence and the probability of the graft having some degree of rejection.
Published Cases of Reuse of a Transplanted Heart
| Case | Publication date | Age, y | AB0 group | Days between HT 1 and 2 | Ischemia time, min | Surgical technique | Induction IS | Maintenance IS | Rejection at follow-up (≥ 2 R) | Follow-up, months | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D | R1 | R2 | D | R1 | R2 | |||||||||
| 1 | 19937 | 20 | 47 | 58 | 0 | 0 | B | 14 | Bicaval | ATG | CsA+AZA+prednisone | Yes | 12 | |
| 2 | 19943 | 28 | 44 | 66 | 2 | Bicaval | ATG | Triple therapy | Yes | 24 | ||||
| 3 | 20084 | 22 | 38 | 45 | 0 | 7 | 197 | Biatrial | ATG | Tacrolimus+MMF+prednisone | No | 13 | ||
| 4 | 20102 | 38 | 52 | 60 | 0 | 0 | 0 | 15 | 193 | Bicaval | Anti-CD25 | Tacrolimus+MMF+prednisone | No | 10 |
| 5 | 20125 | 58 | 60 | 63 | 4 | 231 | Bicaval | No | 9 | |||||
| 6 | 20146 | 18 | 59 | 60 | 16 | 295 | Bicaval | No | 15 | |||||
| 7 | 2016* | 34 | 58 | 62 | A | A | A | 6 | 50 | Biatrial | Anti-CD25 | Tacrolimus+MMF+prednisone | No | 4 |
ATG, antithymocyte globulin; AZA, azathioprine; CsA, cyclosporine; D, donor; HT, heart transplant; IS, immunosuppression; MMF, mycophenolate mofetil; R, recipient.
Ischemia time appears to be a crucial aspect in the reuse of transplanted organs. In our case, given that the donor and the second recipient belonged to the same hospital, the ischemia time was exceptionally short and probably positively influenced the patient's good progress.
The experience from this and other published cases indicates that the reuse of a transplanted heart from a first recipient with early brain death can be an effective alternative to increase the number of organs available for HT in selected cases.