Keywords
INTRODUCTION
Prosthetic valves represent a potential problem when attempting to access the ventricles and may limit the use of radiofrequency ablation. This problem becomes especially relevant in patients with a mechanical aortic valve replacement (MAVR) and left ventricular tachycardia (VT), particularly if these episodes are highly recurrent or incessant.
We present a case in which the left ventricle (LV) was accessed by optimized atrial transseptal puncture for left VT ablation in a patient with an MAVR.
CASE STUDY
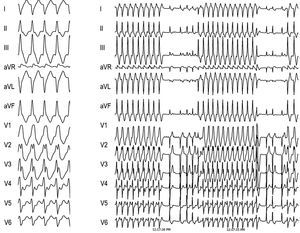
A 61-year-old man with a history of aortic stenosis, implantation of a disc MAVR at age 45, and chronic atrial fibrillation was seen for chest pain, in which incessant VT was observed (Figure 1). The coronary angiography was normal, although an echocardiogram revealed concentric hypertrophy of the left ventricle with normal systolic function and a disc MAVR that was functioning normally.
Figure 1. Left: electrocardiogram at 25 mm/s showing monomorphic ventricular tachycardia, with a cycle of 320 ms and image of right bundle-branch block and right lower axis. Right: electrocardiogram at 10 mm/s showing incessant nature.
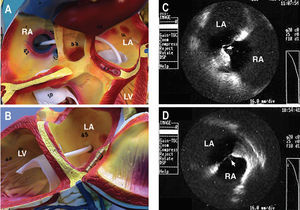
Ventricular tachycardia ablation by the atrial transseptal approach was decided, and a protocol was designed for programmed ventricular stimulation, with negative results. Isoproterenol was then administered, inducing incessant sustained monomorphic ventricular tachycardia equivalent to that observed clinically and with good hemodynamic tolerance. In order to facilitate LV access using a transseptal approach, a preformed guiding introducer designed for the right atrium was chosen (Fast-Cath SR3®, St. Jude Medical) and the transseptal puncture was guided toward the anterior region of the ovale foramen by intracardiac echocardiography (ICE®, Boston Scientific) (Figure 2).
Figure 2. A and B: the distal segment of the transseptal introducer chosen to access the left ventricle transseptally is shown. C: image obtained with intracardiac echocardiography at the transseptal puncture. Observe (arrow) the protrusion produced by the Brockenbrough needle in the anterior region of the foramen ovale, unlike in D, where the ICE® catheter is seen at the posterior limit of the foramen ovale.
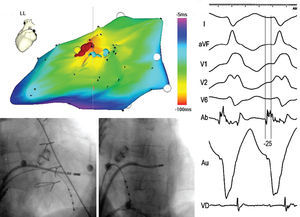
An irrigated catheter with electroanatomic navigation (CARTO®, Biosense-Webster) was used for the mapping and ablation. An LV activation map was obtained during VT, showing a pattern of focal activation originating in the middle segment of the anterolateral wall of the LV (Figure 3). No mid-diastolic potentials or low-voltage areas were observed.
Figure 3. Location of the point of ventricular tachycardia (VT) ablation. A: electroanatomic mapping of the left ventricle (left lateral view) during VT. The orange area indicates the area of earliest activation. Programmed electrical stimulation of the VT was obtained at the yellow point. The radiofrequency application points are shown in red. Fast presystolic potentials were recorded at these points, as well as in neighboring areas of less early activation (blue points), which could express activation of the local Purkinje network. B and C: fluoroscopic images of the ablation catheter in the successful position (right and left anterior oblique view, respectively). D: bipolar (Ab) and unipolar (Au) electrograms obtained at the successful position.
Ablation was done at the earliest point, using increasing power up to 50 W while maintaining a maximum temperature of 38°C at all times. The VT was interrupted 6 s after application, with no subsequent recurrence.
DISCUSSION
The retroaortic route is the conventional approach for left VT ablation.1 In the case of severe aortic stenosis, mechanical aortic valve replacement, intracavitary thrombi, or severe arteriopathy, however, this approach may be contraindicated.
In our case we decided to use an optimized transseptal approach with intracardiac echocardiography to safely perform puncture in the anterior region of the septum and thus facilitate access to the LV.2 In this case, we also chose a preformed transseptal introducer which, although commercially recommended for other anatomical regions, appeared to be morphologically appropriate for this purpose; this fact was later confirmed. The use of this introducer allowed easy access to the entire LV, particularly the area of interest, providing the ablation catheter with extraordinary stability.
The use of navigating systems in electrophysiology has facilitated ablation in "difficult cases."3,4 In this patient, the CARTO® system allowed us to establish the focal origin of the VT, as well as to rule out the presence of scar regions and mid-diastolic potentials. Apart from these data, other factors, such as the inducibility of VT with isoproterenol but not with programmed stimulation, make a reentrant origin unlikely.
Correspondence: Dr. N. Pérez-Castellano.
Unidad de Arritmias, Instituto Cardiovascular. Hospital Clínico San Carlos.
Prof. Martín Lagos, s/n. 28040 Madrid. España.
E-mail: nperez.hcsc@salud.madrid.org