To the Editor,
High rates of unknown diabetes mellitus (DM) have been described in coronary patients.1, 2, 3 Early diagnosis and treatment of DM is essential to reduce cardiovascular morbidity and mortality rates.2 Bramlage et al.4 demonstrated that secondary prevention in coronary patients with diabetes is only viable when optimal standards are met. Therefore, early diagnosis and optimal treatment would provide potential improvement for coronary patients with diabetes.
We analyzed 338 patients that underwent percutaneous coronary interventions (PCI) for revascularization, with systematic oral glucose tolerance tests (OGTT) and no known DM.3 We divided the patients into a group treated with metabolic interventions and a control group. We attempted to determine whether differences could be observed after 1 year of follow-up in terms of: a) adequacy of secondary prevention; b) prevalence of metabolic syndrome (MS), and c) combined cardiovascular events (death, myocardial infarction, stroke, new coronary revascularization, and hospitalization for unstable angina).
The methodology of our study has already been described.3 We performed a clinical interview, a patient examination, and laboratory analyses including OGTT and glycosylated hemoglobin at 15 days after hospital discharge and again at 1 year.
Our center serves as a PCI referral center for 8 hospitals. We offered our patients intensive multidisciplinary treatment. Patients from other hospitals received standard medical treatment and served as the control group. All patients and their responsible physicians were informed of the results of all the tests performed.
Intensive multidisciplinary treatment, based on clinical guidelines,2 was provided during diabetic education nursing, cardiology, and endocrinology visits. All patients were informed as to the nature of the disease, lifestyle changes, tobacco abstinence, treatment (indefinite platelet therapy, beta blockers, statins), and target blood pressure (BP) values<140/90mm Hg and low-density lipoprotein cholesterol (LDL-C) values<100mg/dL. In addition, prediabetic and/or obese patients received personalized hypocaloric diet recommendations, and in patients with occult diabetes, recommendations included diet, metmorphin if there was glycosylated hemoglobin≥6.5% and/or associated obesity, target BP<130/80mm Hg, LDL-C<70mg/dL, and renin-angiotensin system inhibitors.
We described our study sample using traditional descriptive statistics. We compared continuous variables using Student's t-test, the Mann-Whitney U-test, and the Wilcoxon test, as appropriate. We used chi-square tests to compare categorical variables. We performed log rank (Mantel-Cox) and Kaplan-Meier survival curve analyses to test for associations between events and patient groups. We also performed a multivariate Cox regression analysis, adjusted by age, sex, hypertension, MS, renal function, vascular disease, glycemia, acute coronary syndrome, previous infarction, ejection fraction, multivessel disease, and treatment.
There were no significant baseline differences between the treatment (n=104) and control (n=234) groups in terms of age, sex, hypertension, tobacco use, MS, vascular disease, history of infarction, multivessel disease, ejection fraction, BP, weight, lipids, renal function, or glycemia after performing the OGTT (occult DM: 24% vs 22.2%, P=.779; prediabetes: 39.4% vs 33.3%, P=.32; normal glycemia: 36.5% vs 44.4%; P=.190). The only significant differences were found in treatment upon discharge (Table).
Changes in the Various Parameters Measured for Secondary Prevention in the Study Population at 12 Months
| Treatment (n=98) | Control (n=220) | P * | |||||
| Baseline | 12 months | P | Baseline | 12 months | P | ||
| SBP, mm Hg | 132.2±19.6 | 126.7±22.3 | .036 | 135.9±18.8 | 135.8±18.8 | .916 | .035 |
| Controlled BP (<140/90 without DM and <130/80 with DM) | 42 (45.7) | 65 (70.7) | <.001 | 68 (31.3) | 116 (53.5) | <.001 | .819 |
| Weight, kg | 79±14.9 | 77.4±15.4 | <.001 | 78.7±10.8 | 78.5±12.6 | .688 | .045 |
| Waist circumference, cm | 98.8±9.7 | 96.4±9.7 | <.001 | 97.4±7.7 | 96±12.2 | .054 | .001 |
| BMI, kg/m2 | 29.3±4.4 | 28.7±4.7 | .595 | 28.8±3.3 | 28.8±4.1 | .729 | .042 |
| Glucose, mg/dL | 102.2±21.9 | 96.9±12.5 | .005 | 99.03±13.5 | 96.4±12.9 | .001 | .130 |
| HbA1c, % | 4.9±0.72 | 4.8±0.57 | .035 | 4.8±0.57 | 4.8±0.051 | .154 | .080 |
| LDL-C, mg/dL | 90.7±29.2 | 87.2±32.9 | .364 | 94.6±34.3 | 97.6±34.4 | .198 | .134 |
| Controlled LDL-C (<100 without DM and <70 with DM) | 56 (63.6) | 56 (63.6) | 1 | 112 (57.1) | 101 (51.5) | .185 | .401 |
| HDL-C, mg/dL | 43.7±11.1 | 48.7±12.7 | <.001 | 47.6±13.1 | 52.1±13.3 | <.001 | .583 |
| Triglycerides, mg/dL | 141.6±64.6 | 118.9±70.7 | <.001 | 130.9±72.8 | 116.4±61.2 | <.001 | .225 |
| Microalbuminuria, mg/g creatinine | 5.4±15.8 | 4.8±11.3 | .133 | 4.2±12.6 | 4.3±10.9 | .240 | .419 |
| MS | 53 (54.1) | 36 (36.7) | .005 | 99 (45) | 88 (40) | .208 | .066 |
| Number of MS criteria met | 2.4±1.1 | 2.1±1.2 | .011 | 2.2±1.1 | 2±1.1 | .001 | .727 |
| Statins | 89 (90.8) | 89 (90.8) | 1 | 175 (79.5) | 186 (84.5) | .029 | .839 |
| ACE inhibitors/ARB | 50 (51) | 68 (69.4) | <.001 | 75 (34.1) | 75 (34.1) | 1 | <.001 |
| Beta blockers | 78 (82.6) | 71 (79.6) | .092 | 156 (70.9) | 148 (67.2) | .815 | .125 |
| Anti-platelets | 97 (99) | 97 (99) | 1 | 219 (99.5) | 219 (99.5) | 1 | 1 |
| Quadruple therapy | 42 (40.4) | 45 (48.9) | .180 | 45 (19.2) | 48 (22.1) | .424 | .710 |
ACE inhibitors/ARB, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers; BMI, body mass index; BP, blood pressure; DM, diabetes mellitus; HbA1c, glycosylated hemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; MS, metabolic syndrome.
Quadruple therapy: combined treatment with statins, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, beta blockers, and antiplatelets.
Categorical variables are expressed as the absolute value (%), while numerical variables are expressed as mean±standard deviation.
* Test for heterogeneity of differences between treatment and control groups.
Six patients (5.7%) were lost to follow-up in the intensive multidisciplinary care group vs 14 in the control group (6%).
The Table shows the changes observed in the secondary prevention group after 1 year. The prevalence of MS, as a paradigm of global secondary prevention, decreased in the treatment group (54.5% vs 36.7%; P=.005) but did not vary in the control group (45% vs 40%; P=.208).
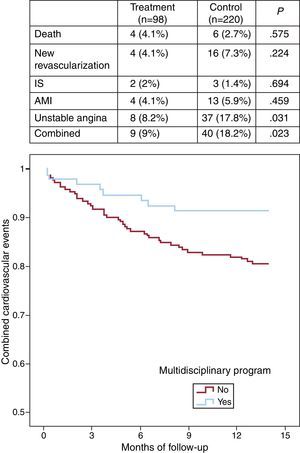
After 1 year of follow-up (Figure), we observed a lower rate of cardiovascular events in the treatment group (9.2% vs 18.2%; P=.023). The decrease in cardiovascular events was primarily in rehospitalizations for unstable angina. Inclusion in the intensive multidisciplinary treatment program was associated with fewer events (odds ratio=0.36; 95% confidence interval, 0.15-0.86; P=.022).
Figure. Kaplan-Meier curve for survival free of cardiovascular events. Event details. AMI, acute myocardial infarction; IS, ischemic stroke.
In this study, we show that a multidisciplinary group of health care professionals that provide coordinated care to coronary patients with no known DM can achieve positive results in 3 distinct aspects: a) improved optimization of secondary prevention, with increased use of quadruple therapy (48.9% vs 22.1%), yielding a higher percentage of targets reached and lower BP and LDL-C levels; b) decreased prevalence of MS, and c) a decrease in combined cardiovascular events.
Our study's limitations are due to the sample size (e.g., absence of statistical significance for MS despite clinically relevant changes) and its observational, nonrandomized design. Since other inherent variables come into play with the intensive treatment protocol (tertiary hospital, shifts, and a coronary unit run by cardiologists), not all changes can be attributed to the intensive treatment.
At a time when European and American medical societies have not reached an agreement on the recommendations for using OGTT,2, 5 our study poses the following question: does the use of OGTT in coronary patients (even those selectively chosen6) aid in improving the health of our patients? Our data suggests that it does.
FundingThis study was partially funded by a clinical research grant from the Spanish Society of Cardiology. Pablo Martínez-Camblor was supported by the Grant MTM2011-23204 of the Spanish Ministry of Science and Innovation (FEDER support included).
Corresponding author: jesusdelahera@gmail.com