Tricuspid regurgitation (TR) has received little attention from clinicians and researchers, and in Spain few centers have published their experience with this process.1 In 2013, our group reported the outcomes of surgical treatment of severe TR in a series of 119 consecutive patients who underwent surgery between April 1996 and February 2010, and high perioperative and long-term mortality was found.2 Today, this series should be considered historic, and the outcomes cannot serve as a guide for predicting those that would currently be obtained after surgery for TR. The objective of the present study was to analyze the clinical and echocardiographic outcomes of a recent sample of patients with severe TR who underwent surgery.
This retrospective study included 87 consecutive patients with severe TR who underwent tricuspid surgery in our hospital between March 2010 and December 2013. The indication for tricuspid surgery was established by the presence of a symptomatic and severe tricuspid lesion according to the echocardiographic definition described in our previous study.2 Treatment was decided by consensus among cardiologists, cardiac surgeons, and the patient. Repair was always the preferred option if technically feasible, essentially in cases with absence of significant organ damage. As an exception, valve replacement was considered, according to the judgement of the surgeon, in cases with functional damage and prior cardiac surgery. Perioperative and long-term morbidity and mortality were analyzed, as well as onset of new severe TR. Predictive factors were studied.
In the period analyzed, ring-free annuloplasty according to the De Vega technique was performed in 4 patients while ring annuloplasty was done in 60; 23 patients received biologic prostheses while none received mechanical prostheses. The Table summarizes the patients’ baseline characteristics, complications after surgery, and perioperative mortality. Overall, 74.7% of the patients were women (mean age, 64.64 [10.08] years). The etiology was organic in 60.9% of tricuspid replacements and functional in 85.9% of repairs. In the group with repaired valves, the patients were older (40.6% vs 17.4% > 70 years; P = .044), had higher preoperative pulmonary pressures (pulmonary artery systolic pressure, 55.67 [14.85] vs 39.65 [14.06] mmHg; P<.001), and a lower proportion of tricuspid surgery alone (7.8% vs 52.2%; P<.001). In 47.1% of the patients, a complication arose during the postoperative period, and perioperative mortality was 8%.
Baseline and Surgical Characteristics of the Patients, Surgical Complications, and Perioperative Mortality
| Total number of patients (n = 87) | Triscuspid repair (n = 64; 73.6%) | Triscuspid replacement (n = 23; 26.4%) | P | |
|---|---|---|---|---|
| Age, y | 64.64 ± 10.08 | 65.64 ± 9.95 | 61.87 ± 10.11 | .124 |
| Age > 70 y | 34.5 (30/87) | 40.6 (26/64) | 17.4 (4/23) | .044 |
| Female sex | 74.7 (65/87) | 73.4 (47/64) | 78.3 (18/23) | .648 |
| Renal failure | 10.3 (9/87) | 10.9 (7/64) | 8.7 (2/23) | .762 |
| COPD | 16.1 (14/87) | 20.3 (13/64) | 4.3 (1/23) | .074 |
| Previous CVA | 2.3% (2/87) | 0% (0/64) | 8.7 (2/23) | .017 |
| Charlson comorbidity index | 4.36 ± 1.54 | 4.31 ± 1.31 | 4.53 ± 2.08 | .548 |
| Prior surgery | 32.2 (28/87) | 26.6 (17/64) | 47.8 (11/23) | .061 |
| Sinus rhythm | 82.8 (72/87) | 15.6 (10/64) | 21.7 (5/23) | .506 |
| Organic etiology | 26.4 (23/87) | 14.1 (9/64) | 60.9 (14/23) | < .001 |
| Functional etiology | 73.6 (64/87) | 85.9 (55/64) | 39.1 (9/23) | < .001 |
| LVEF, % | 61.79 ± 9.08 | 62.48 ± 9.19 | 59.87 ± 8.64 | .238 |
| LVEF< 45% | 6.9 (6/87) | 6.2 (4/64) | 8.7 (4/64) | .691 |
| PASP, mmHg | 51.44 ± 16.21 | 55.67 ± 14.85 | 39.65 ± 14.06 | < .001 |
| Presurgical PASP > 35 mmHg | 85.1 (74/87) | 95.3 (61/64) | 56.5 (13/23) | < .001 |
| Presurgical PSAP > 70 mmHg | 17.2 (15/87) | 21.9 (14/64) | 4.3 (1/23) | .056 |
| Tricuspid surgery alone | 19.5 (17/87) | 7.8 (5/64) | 52.2 (12/23) | < .001 |
| Mitral prostheses | 55.2 (48/87) | 64.1 (41/64) | 30.4 (7/23) | .005 |
| Aortic prosthesis | 23 (20/87) | 26.6 (17/64) | 13 (3/23) | .186 |
| Mitral and aortic prostheses | 19.5 (17/87) | 23.4 (15/64) | 8.7 (2/23) | .126 |
| Mitral repair | 17.2 (15/87) | 21.9 (14/64) | 4.3 (1/23) | .056 |
| Coronary surgery | 6.9 (6/87) | 6.2 (4/64) | 8.7 (2/23) | .691 |
| Logistic EuroSCORE | 10.68 ± 9.68 | 11.22 ± 10.32 | 9.41 ± 8.05 | .456 |
| Duration of ECC, min | 117.43 ± 48.72 | 118.98 ± 44.28 | 112.78 ± 61.40 | .643 |
| Low postsurgical cardiac output | 21.8 (19/87) | 23.4 (15/64) | 17.4 (4/23) | .547 |
| Postsurgical complications | ||||
| Infectious | 8 (7/87) | 10.9 (7/64) | 0% (0/23) | .098 |
| Neurologic | 4.6 (4/87) | 4.7 (3/64) | 4.3% (1/23) | .947 |
| Respiratory | 20.7 (18/87) | 21.9 (14/64) | 17.4 (4/23) | .649 |
| Renal | 13.8 (12/87) | 14.1 (9/64) | 13 (3/23) | .903 |
| Reoperation due to bleeding | 5.7 (5/87) | 3.1 (2/64) | 13 (3/23) | .080 |
| Any complication | 47.1 (41/87) | 50 (32/64) | 39.1 (9/23) | .370 |
| Mortality | 8 (7/87) | 7.8 (5/64) | 8.7% (2/23) | .894 |
CVA, cerebrovascular accident; ECC, extracorporeal circulation; LVEF, left ventricular ejection fraction; PASP, pulmonary artery systolic pressure.
Data expressed as No. (%) or mean ± SD.
A multivariate analysis was performed to identify predictors of perioperative mortality. The analysis included left ventricular ejection fraction < 45%, the only variable significantly associated with the event in the univariate analysis (), as well as the variables identified as predictors in our previous study (age, duration of extracorporeal circulation).2 The only predictor of perioperative mortality was left ventricular ejection fraction < 45% (odds ratio, 10.531; 95% confidence interval [CI], 1.262-87.905; P = .030).
After discharge following the operation, changes in TR were assessed in 66 of the 80 survivors (82.5%) in echocardiographic follow-up (median, 30 [interquartile range, 20-44] months). Severe TR occurred in 4 patients, all belonging to the group of ring-free annuloplasty (7.1% of patients with follow-up in this group). Predictors of the onset of severe TR during follow-up were not assessed, given its low incidence.
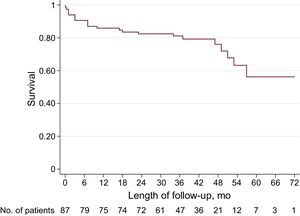
Mortality was assessed after a follow-up that included all survivors of the perioperative period (median, 38 [30.25-48] months).
Mortality during overall follow-up was 18.8% among patients alive on discharge from hospital and the overall mortality (perioperative and during overall follow-up) was 25.3%. A univariate analysis of overall mortality was performed () and multivariate analysis of the variables with a significant association was performed. The only predictor of overall mortality was the duration of extracorporeal circulation (hazard ratio, 1.012; 95% CI, 1.003-1.021; P=.009). The Figure shows the survival curve during follow-up of the cohort of patients in the study.
In the present study, perioperative mortality was 8%, comparable to that found in other extensive studies in Spain,3 but somewhat lower than 18.5%, the mortality rate obtained in our previous study.2 The reasons for the improved perioperative mortality in our study cannot be inferred from this study because of its design. One possibility would be that the indication for surgery is increasingly made in earlier stages of the disease, in line with studies that have shown higher mortality in patients with more advanced symptoms at the time of surgery.4 In addition, clinical and anesthetic experience acquired over time has probably also had a positive impact on outcomes. It is foreseen that these outcomes may be improved through use of different percutaneous treatments already developed for the treatment of severe TR, with a low periprocedural morbidity and mortality.5
In our study, the duration of extracorporeal circulation was a predictor of overall mortality, as in our previous series.2 A long duration of extracorporeal circulation reflects greater valve comorbidity, which supports the prognostic value of this variable for follow-up.
In addition to the impossibility of identifying determinants of improved clinical outcomes, other limitations of this study are due to its retrospective and single-center nature, and the absence of data with prognostic value such as right ventricular volume and function.
In conclusion, in our series of patients with severe TR who underwent surgery, short- and long-term clinical outcomes bore little relation to the suboptimal findings of our previous series. Left ventricular ejection fraction < 45% was identified as a predictor of perioperative mortality, while duration of extracorporeal circulation was a predictor of long-term mortality.