To the Editor,
Persistent left superior vena cava (LSVC) is a relatively common congenital anomaly, with an estimated prevalence of around 0.5%. In patients with congenital heart disease, the figure reaches almost 5% and in 10% there is no right superior vena cava. There are numerous case reports in the literature and a few small series in which pacemakers or defibrillators have been implanted through the LSVC. All describe specific techniques used to place electrical stimulation leads at a stable site;1, 2, 3 some also propose techniques to locate the electrode lead in the right ventricular apex (RVA).4 To date, however, there have been few reports on the possibility of or the techniques used to implant leads in the region of the right ventricle outflow tract (RVOT).5
We present 2 cases in which the electrode lead was implanted in the RVOT via the LSVC. The first case was a 72-year-old female with a history of obesity and hypertension who was admitted for clinical fatigue of several weeks duration. In the electrocardiogram (ECG) and subsequent ECG monitoring, we documented alternation between an atrioventricular (AV) junctional rhythm at 45 bpm and sinus bradycardia with left anterior hemiblock. Echocardiography was performed and revealed slight concentric left ventricular hypertrophy with preserved systolic function. The electrophysiological study showed an HV interval of 60ms and a slightly prolonged (600ms) corrected sinus node recovery time, with significant secondary breaks (2800ms).
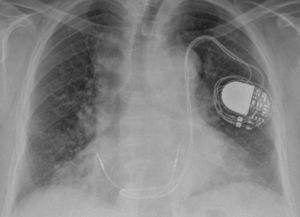
A dual chamber permanent pacemaker was implanted via the left axillary vein. However, the guidewire route led to a suspicion of LSVC persistence which was confirmed by venography. It was decided to implant the leads through the LSVC. In the first place, a 58cm active fixation lead (Medtronic CapSure Fix 5076) with a distal electrode was inserted in the RVOT. This was done using a manually preformed stylet with a 180° curve approximately 4cm from the tip. A 52cm active fixation lead (Medtronic CapSure Fix 5076) with a distal electrode was then implanted on the upper side of the right atrium (RA), using a manually preformed stylet with a 60° curve approximately 3cm from the tip. Both showed optimum electrical parameters, so the procedure was completed. No dislocations or changes in the stimulation parameters were observed during follow-up (Figure 1, Figure 2).
Figure 1. Posteroanterior chest radiograph, with leads inserted through the left superior vena cava. Distal ventricular electrode anchored in the right ventricular outflow tract.
Figure 2. Lateral chest radiograph, with distal ventricular electrode in the right ventricular outflow tract.
The next case was an 82-year-old male with a history of hypertension, hyperlipidemia, ischemic heart disease (acute inferior myocardial infarction), chronic obstructive pulmonary disease, and multiple myeloma. The patient was admitted for repetitive syncope after the ECG showed sinus rhythm with bifascicular block (RBBB+LAFB). Interrupted episodes of complete paroxysmal AV block were detected during electrocardiographic monitoring on the ward. Echocardiography showed mild left ventricular systolic dysfunction with inferior akinesis.
During implantation of a two-chamber permanent pacemaker via the left axillary vein, we observed LSVC persistence, the characteristics of which were similar to those described in the previous case. Two active fixation leads with distal electrodes were implanted in RA and RVOT, using manually preformed curved stylets identical to those described in case 1.
No dislocations or changes in the stimulation parameters were observed during follow-up.
Persistent LSVC can make implantation of a permanent pacemaker difficult. The fact that the coronary sinus ostium is not aligned with the tricuspid annulus means that the main technical problem consists of inserting the lead in the RV. The RVA has been the site of choice for cardiac stimulation, but reaching it in these cases usually means that the probe electrode forms a big loop in the RA.
Stimulation in the RVOT has been proposed as an alternative to RVA stimulation. In terms of lead stability, it has shown similar long-term results to those achieved with stimulation at the apex,6 and has also been shown to produce less dyssynchrony. Ventricular dyssynchrony promotes remodeling and in patients with left ventricular systolic dysfunction may have a deleterious effect on cardiac function. However, to date the benefits of RVOT stimulation have not been demonstrated in a randomized clinical trial. We have proposed a technique to reach this stimulation site in patients with persistent LSVC which only requires a manually preformed stylet. This can be similar to those used in normal conditions to reach the RVA, but without the need to form a loop in the RA.
Corresponding author: javierjimenezdiaz@wanadoo.es