Catheter ablation is very effective for symptom control in atrial fibrillation (AF).1 Because of the high volume of procedures performed, strategies are required to optimize allocated resources. In this letter we present the results of the first day-case program for AF catheter ablation in Spain.
We prospectively analyzed all elective AF catheter ablation procedures performed over 2 consecutive years, using a conventional strategy (n=100), from April 1, 2018 to March 31, 2019, and using an early-discharge strategy (n=123), from April 1, 2019 to March 31, 2020.
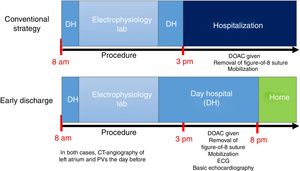
The patient flowchart for each strategy is shown in figure 1. Patients who were receiving oral anticoagulant treatment (n=182, of whom 11 were taking acenocoumarol) omitted it on the morning of the procedure. Independently of the treatment discharge strategy, the catheter ablation itself was carried out using the same method, following current recommendations. Conscious sedation with dexmedetomidine was given as a continuous infusion2 and a figure-of-eight suture was used for hemostasis.3 In the conventional strategy, patients were admitted to hospital following the procedure. In the early-discharge strategy, they were discharged before 8 pm on the same day, provided there were no complications; if complications occurred, per protocol, they were admitted. Patients who had early discharge were contacted at 48 hours and 10 days after the procedure.
The primary efficacy objective was to determine the proportion of patients in the early-discharge strategy who were discharged on the same day having spent less than 12 hours in hospital. The primary safety objective was to determine the need for emergency department care in the 10 days after discharge (ED-10), presumably related to the procedure. The secondary objective was to perform an economic analysis comparing the 2 strategies. The estimated saving was calculated as the mean difference in cost per procedure in day-hospital care, days of hospital stay, and ED-10. The prices used were taken from the public prices for health care services from 3 public health boards in Spain.
Continuous variables with normal distribution are described as mean±standard deviation, and categorical variables as absolute number and percentage. Comparison of categorical variables was performed with the chi-square test. Comparison of 2 continuous variables with normal distribution was performed with Student t test. Logarithmic ranges were used to compare the ED-10 cumulative incidence. A P value<.05 was considered statistically significant.
Table 1 shows the patient characteristics, immediate outcomes, and procedural complications, which were similar for the 2 strategies. In the early-discharge strategy, in 111 (90%) of 123 procedures, the patient was discharged within 12 hours of arrival at the hospital; the remaining 12 patients (10%) were admitted to hospital. The reasons for admission were: immediate complications (n=8), vagal response on mobilization (n=2), Brugada type 1 pattern after administration of oral flecainide (n=1), and observation due to a history of contrast allergy (n=1). The frequency of early discharge was similar in cryoablation (n=69; 88%) and radiofrequency ablation (n=42; 93%); (P=.5).
Comparison of epidemiological, clinical, and procedural characteristics according to the strategy used
| Variable | Conventional strategy (n=100) | Early discharge (n=123) | P |
|---|---|---|---|
| Age, y | 59±10 | 59±10 | .8 |
| Women | 29 | 25 | .5 |
| Type of AF | .2 | ||
| Paroxysmal | 55 | 47 | |
| Permanent | 45 | 53 | |
| CHA2DS2-VASc | 1.2±0.1 | 1.1±0.1 | .5 |
| Previous long-term oral anticoagulation | 82 | 81 | .9 |
| Hypertension | 37 | 44 | .3 |
| Diabetes | 34 | 37 | .6 |
| Obesity | 30 | 33 | .7 |
| History of heart failure | 17 | 10 | .1 |
| LVEF, % | 57±8 | 58±7 | .06 |
| LVEF ≤ 45% | 10 | 9 | .9 |
| Left atrial area, mm2 | 27±10 | 28±9 | .8 |
| Chronic kidney disease | 3 | 4.3 | .6 |
| Energy used | .8 | ||
| Cryoablation | 62 | 63 | |
| Radiofrequency | 38 | 37 | |
| Previous AF ablation | 12 | 18 | .2 |
| Ablation of CTI during procedure | 18 | 16 | .5 |
| Ablation of substrates outside the PVs | 10 | 12 | .7 |
| Duration of procedure, min | 132±42 | 129±45 | .6 |
| Isolation of all PVs | 100 | 97.5 | .8 |
| Acute complications | 5 | 5.7 | .8 |
| Small hematoma | 3 | 4 | |
| Femoral pseudoaneurysm | 1 | 1 | |
| Non-Q wave AMI | 0 | 1 | |
| Pericarditis | 1 | 2 | |
| Time procedure ended | .5 | ||
| Before 12 noon | 2 | 4 | |
| 12 noon-1 pm | 64 | 62 | |
| 1-2 pm | 21 | 19 | |
| 2-3 pm | 11 | 12 | |
| After 3 pm | 2 | 3 | |
| Hospital stays | 1±0.3 | 0.1±0.6 | <.001 |
| Attended emergency department within 10 days of discharge | 12 | 13.8 | .7 |
| AF/atrial flutter | 4 | 6 | |
| Pericarditis | 1 | 3 | |
| Small hematoma | 4 | 3 | |
| Urticaria | 1 | 3 | |
| Epistaxis | 0 | 1 | |
| Dizziness | 0 | 1 | |
| Gastroparesis | 1 | 0 | |
| Bronchopneumonia | 1 | 0 | |
| Mean cost per patient, € * | |||
| Sanidad de Castilla y León health board, 2013 | 496 (467-525) | 125 (75-125) | <.001 |
| Servicio Murciano de Salud health board, 2019 | 775 (732-819) | 230 (156-304) | <.001 |
| Osakidetza health board, 2019 | 1372 (1303-1440) | 474 (353-594) | <.001 |
AF, atrial fibrillation; AMI, acute myocardial infarction; CTI, cavotricuscpid isthmus; LVEF, left ventricular ejection fraction; PVs, pulmonary veins.
Values are expressed as percentage, mean±standard deviation or mean (95% confidence interval).
The incidence of ED-10 was 12% in the conventional strategy vs 13.8% in the early-discharge group (P=.7). Table 1 shows the reasons for ED-10. All of these patients were discharged within 8 hours. In the early-discharge group, only one ED-10 occurred, the day after discharge. The mean cost per procedure was lower in the early-discharge strategy (table 1).
Several studies have shown that, in experienced centers, AF catheter ablation with same-day discharge is feasible (more than 80% of cases) and safe.4,5 Our data support this: 90% of our patients were able to be discharged after less than 12 hours in hospital, with a similar frequency for cryoablation and radiofrequency procedures. Compared with the conventional strategy, the early-discharge strategy is safe, in that the need for ED-10 was similar, and was mainly due to recurrence of AF/flutter or small hematomas. Regarding timing, only 1 patient from the early-discharge group attended the ED, the day after the procedure, due to a small hematoma. This was the only incidence of ED care that could have been avoided by hospitalization after the procedure.
The early-discharge strategy allows a reduction in hospital stay. This becomes more even more relevant in the context of the COVID-19 pandemic, as several scientific societies have suggested prioritizing day-case procedures.6 Given that same-day discharge does not increase short-term mortality, it also generates a significant economic saving.