Keywords
INTRODUCTION
Heavily calcified lesions (HCL) present a challenge for percutaneous coronary intervention.1,2 If managed aggressively, they cause dissection or incomplete apposition of the stent, which prior preparation of the plaque would avoid.3
Paclitaxel-eluting stents (PESs) have been shown to help reduce restenosis and revascularization in vessels with HCL.4 Rotational atherectomy (RA) facilitates differential ablation of calcified plaque which, in turn, facilitates angioplasty and implantation.5,6 However, the major studies of PESs have considered this an exclusion criterion.
Small-sample observational studies report good results for sirolimus-eluting stents used in HCL treatment following RA.7
The present study analyzes immediate and 1-year results following treatment of HCL with RA and PES implantation.
METHODS
We analyzed a retrospective series of 50 consecutive patients from the same center who underwent RA and received at least 1 PES implant between April 2005 and April 2007. All presented HCL according to qualitative angiographic criteria determined by the physician responsible for the procedure.
A physician not directly related with the procedure recorded incidence of death (from cardiac or any other cause) and of clinically indicated revascularization of the lesion treated (RLT). Quantitative angiographic evaluation was with QCA-CMS® (Medis Medical Imaging Systems) before and after the procedure.
Procedure
All patients received acetylsalicylic acid (150-300 mg/day) and clopidogrel (300 mg of load, 75 mg/day), from at least 24 h preprocedure. After angiographic confirmation of HCL, treatment began immediately, or not, at the discretion of the operator.
A 0.09 inch guidewire was introduced directly or following exchange using a microcatheter or coaxial balloon. Rotational atherectomy was with a Rotablator® (Boston Scientific-Scimed Corp.) at 140 000-180 000 rpm and a 0.7 burr-to-minor artery ratio. Advancement was slow (maximum 10 s) and saline solution was administered with heparin, nitroglycerin and verapamil during atherectomy. Patients received at least 1 PES following dilatation in all cases. Subsequently, stent dilatation was applied if residual stenosis was >50%. Nonfractioned heparin (70-100 U/kg) and abciximab were administered as coadjuvant medication at the operator's discretion.
Postprocedure, double antiplatelet therapy with clopidogrel (75 mg/day) and aspirin (100-300 mg/ day) was administered for at least 12 months. Creatinkinase (CK) and CK-MB fraction enzymes were recorded at 8, 12, and 24 h postprocedure. In the follow-up, all deaths were considered cardiac unless diagnosed otherwise. Residual stenosis of <20% was considered an angiographic success.
Statistical analysis was with SPSS 15.0. Continuous variables are expressed as mean±SD and categorical variables as number and percentage. Pre-event time lapse was estimated with Kaplan-Meier curves.
RESULTS
Baseline patient characteristics are in Table 1. We enrolled 50 patients with mean age 70 (1.2) years; 68% men; 52% with acute coronary syndrome. In 14 (28%) patients, ejection fraction (EF) was <55%.
Forty patients (80%) presented multivessel disease and 15 (30%) a diseased left main coronary artery (LMCA). Rotational atherectomy was of 1 vessel in 44 (88%) patients, 2 vessels in 4 (8%), and 3 vessels in 2 (4%); RA was of the LMCA in 12 (24%) patients, 3 of whom presented protected LMCA. Angiographic characteristics are in Table 2. Mean reference diameter was 2.83 (0.8) mm; mean lesion length, 29 (2.6) mm; 28 (56%) patients presented >20 mm lesions and 11 (22%) had >45° angulation.
Abciximab was administered to 22 (44%) patients at the operator's discretion. The most frequently used burr size was 1.5 mm (30 [60%] patients). After RA, all lesions were predilatated and at least 1 PES was deployed with 92% angiographic success.
Dissection requiring repair occurred in 1 (2%) patient. Perforation by the intracoronary guidewire occurred in another (2%) although this did not affect the vessel treated with RA. In 1 patient (2%), acute vessel closure occurred and was resolved by stenting.
Prophylactic pacemakers were not implanted although 1 patient subsequently did require one for complete atrioventricular (AT) block. The device was extracted in the laboratory after nodal conduction recovery.
Significant (>1.5 mm) branch loss occurred in 2 (4%) patients. We recorded CK-MB elevation (<20 mg/dL) in 14 (28%) patients although data did not follow a normal distribution (median, 4.7; interquartile range, 3.45-8.70). This was relevant (>20 mg/dL) in 7 (14%) patients.
No deaths occurred during the procedure. Two deaths occurred during hospitalization: one patient died at 24 h due to cardiac tamponade related with the intracoronary guidewire that perforated a vessel other than the one treated by RA. Another patient (81 years, diseased LMCA, and 3 vessels) died of cardiac arrest at 5 days.
The remaining patients (96%) were followed up for median 14 months after discharge. One patient (65 years, severely depressed EF, 3 diseased vessels) died at 4 months postprocedure. We recorded another 2 postprocedure deaths due to noncoronary causes: 1 patient died of leukemia at 9 months; another died of a stroke at 4 months.
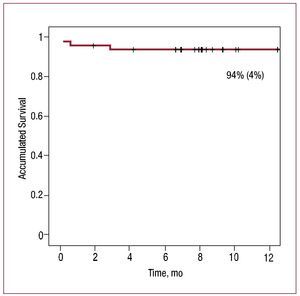
Kaplan-Meier curves showed 94% (4%) survival free of cardiac death at 1 year (Figure 1) and 89% (5%) overall survival (free of any cause death).
Figure 1. One-year survival free of cardiac cause death.
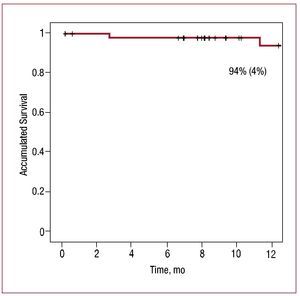
At 1-year follow-up, 94% (4%) of surviving patients were RLT-free and 3 required revascularization (Figure 2). When contacted at 1 year, 81% of survivors were free of angina.
Figure 2. One-year survival free of revascularization of the lesion treated.
DISCUSSION
In an unselected series of patients with complex lesions, RA and PES implantation produced 92% angiographic success. These results coincide with other published series of patients treated with RA.8-10
Two (4%) patients died in-hospital, which is comparable with previously reported studies.9,11,12 Kini et al8 found 0.2% in-hospital mortality in a younger population (65 [11] years) with a more favorable angiographic profile (17 [8] mm mean lesion length; 58% calcified; 7% bifurcated). We recorded minimal intraprocedural complications by comparison with prior studies.7,11 Incidence of type B or greater dissection (2%) and acute vessel closure (2%) was minimal. The only major complication (perforation by intracoronary guidewire) occurred in a vessel not treated with RA.
We recorded substantial CK-MB elevation (>20 ng/mL) in 14% of patients, exceeding that reported elsewhere, although with no repercussions on clinical results.9,12 Both procedural and follow-up results for this series were good despite the high-risk population with complex lesions.
The results show excellent 1-year survival from cardiac-cause death. Overall mortality at 1 year was 2 deaths from proven noncardiac causes and 2 deaths in-hospital.
Clavijo et al7 describe a series of patients with HCL treated by RA and sirolimus-eluting stent (SLS) implantation and report 6.8% 6-month mortality among discharged patients.
The RLT was 6% per year, indicating a substantial reduction versus the 16%-25% described for conventional stents after RA.6,9,13 Clavijo et al report 4.2% 6-month RLT using SLS.7
At >1 year, >80% of patients remain free of angina versus 75% at 9 months and 58% at 1 year reported in conventional stent studies.9,13
The principle limitations of the study are its retrospective design, small sample size and lack of a control group.
CONCLUSIONS
The present paper describes results of using PES after RA in heavily calcified lesions. This strategy produces a high angiographic success rate with low incidence of short-term major clinical events. At 1-year follow-up, we found a high rate of survival from cardiac death with low RLT.
Similar findings have been published on the use of SLS after RA in patients with HCL. More extensive studies are needed to confirm these findings.
Correspondence: Dr. J. García de Lara.
Servicio de Cardiología. Hospital Virgen de la Arrixaca. Carretera de Cartagena, s/n. 30120 El Palmar. Murcia. España.
E-mail: garciadelara@secardiologia.es
Received November 18, 2008.
Accepted for publication May 20, 2009.