Keywords
INTRODUCTION
Coronary fistulae are anomalous communications between a coronary artery and a cardiac chamber or other vessel in the vicinity of the heart. They are the most frequently occurring congenital heart anomalies and are discovered in 0.15% of patients undergoing coronary angiography.1 In general, they are small and lack clinical significance although they can cause an arteriovenous shunt with hemodynamic repercussions. Generally, fistulae are asymptomatic but in time asthenia, dyspnea, and heart failure can appear if the shunt is substantial.2 In adults, fistulae are usually discovered by chance during coronary angiography. Currently, immediate percutaneous closure is preferred and surgical closure is reserved for multiple or larger fistulae.3 Percutaneous balloon or coil occlusion has been safely and efficiently performed since more than a decade ago and has become the first choice therapeutic option.4
From January 2001 thru December 2003, in a total of 3075 coronary angiographies we found 4 (0.13%) adults with coronary fistulae draining into vessels in the pulmonary territory. All 4 patients underwent percutaneous closure with coils.
Description of the Technique
Following selective catheterization of the coronary ostium with a 6 F catheter guide wire, a 260 cm long, conventional, 0.014 inch coronary angioplasty guide wire is introduced. Using an external rotor, this is advanced to the fistula where it is located as distal as possible. A 1.9 F microcatheter is passed along the guide wire through which the coils needed to occlude the fistula are introduced. Diathermic current is used to release the coils from the transport mechanism.
CLINICAL CASES
Case 1
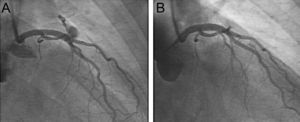
A 47 year-old woman, without risk factors, presented with chest discomfort of 1 month duration. Baseline electrocardiogram (ECG) only showed non-specific repolarization disturbances. Tomography revealed a reversible perfusion defect on the anterolateral surface. Coronary angiography showed no lesions other than a fistula originating in the anterior descending artery (ADA) and draining into the pulmonary artery trunk (Figure 1 A). The fistula was closed with 1 coil and immediate post-deployment angiograms indicated success (Figure 1 B). Clinical symptoms remitted and at 30 months post-procedure the patient remained asymptomatic.
Figure 1. Case 1. Coronary fistula between anterior descending artery and origin of pulmonary artery. Oblique right anterior projection before (A) and after (B) closure with coils.
Case 2
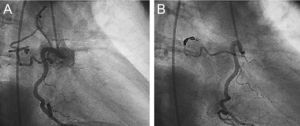
A 71 year-old woman with acute coronary syndrome without ST segment elevation. Coronary angiography showed significant lesions in ADA and circumflex (CX) arteries. Right coronary artery (RCA), without obstructive lesions, presented an anomalous vessel with an irregular trajectory in the proximal segment draining into the left pulmonary vascular bed (Figure 2 A). Stents were implanted in ADA and CX and the fistula closed, requiring deployment of 4 coils (Figure 2 B). The patient remained asymptomatic at 15 months of clinical follow-up.
Figure 2. Case 2. Fistula from right coronary artery to posterior segment of left lung. Images in oblique anterior right projection before (A) and after (B) closure with coils.
Case 3
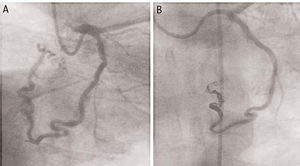
A 68 year-old man with unstable angina refractory to treatment underwent urgent cardiac catheterization. The patient presented significant obstructive lesions in ADA and RCA and fistulous connection from CX draining into the posterior segment of the left lung (Figure 3 A). Following stent implantation in ADA and RCA the fistula was tackled, requiring 6 coils to achieve successful occlusion (Figure 3 B). The patient remained asymptomatic at 1 year follow-up.
Figure 3. Case 3. Fistula from circumflex artery draining into left lung. Images in oblique anterior right projection from outflow angle before (A) and after (B) closure with 6 coils.
Case 4
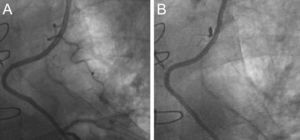
A 55 year-old man with severe multiple vessel coronary heart disease surgically revascularized 6 months earlier (mammary artery to ADA and saphenous vein to RCA and CX). The patient was asymptomatic until admission for progressive angina during exercise. The perfusion study showed reversible hypocaptation on the anterior surface. Coronary angiography showed all grafts functioned well and the only abnormality was the presence of a lateral branch from the internal mammary artery graft draining into left pulmonary territory (Figure 4 A). This was closed with 1 coil (Figure 4 B) and at 5 months post-procedure the patient remained asymptomatic.
Figure 4. Coronary steal from internal mammary artery graft by lateral branch draining into left lung. Images in oblique anterior right projection before (A) and after (B) closure with 1 coil.
DISCUSSION
Coronary artery fistulae can be primary, when isolated, or secondary, when there is a recognizable cause.5,6 Some authors recommend closure of all fistulae during infancy even if they are asymptomatic. However, others propose treatment only in symptomatic patients or in those at risk of complications such as coronary steal, aneurysm or substantial arteriovenous shunt,7 which can cause myocardial ischemia.8 Currently, percutaneous treatment is proposed as the first choice because it is less radical and entails a shorter period of hospitalization3; surgery is reserved for cases of multiple fistulae, those affecting large branches during embolization of coils, or when the fistulous connection is narrow, restrictive and draining into a cardiac chamber.2,9
Among fistula embolization products are polyvinyl alcohol foam,10 balloons,11 and coated stents1,12 but the most widely used devices are undoubtedly coils.2,13-17 Although complications have been described in some isolated cases of coil embolization, these have been exceptions and of little significance.14,18,19 In our 4 patients, the fistula was successfully closed and symptoms disappeared without complications.
Correspondence: Dr. L.S. Díaz de la Llera.
Pinsapo, 10. Urb. Pinares de Oromana. 41500 Alcalá de Guadaira. Sevilla. España.
E-mail: luissalvadordiaz@hotmail.com