Prognosis in ST-elevation myocardial infarction (STEMI) is determined by delay in primary percutaneous coronary intervention (PPCI). The impact of first medical contact (FMC) facility type on reperfusion delays and mortality remains controversial.
MethodsWe performed a prospective registry of primary coronary intervention (PCI)-treated STEMI patients (2010-2020) in the Codi Infart STEMI network. We analyzed 1-year all-cause mortality depending on the FMC facility type: emergency medical service (EMS), community hospital (CH), PCI hospital (PCI-H), or primary care center (PCC).
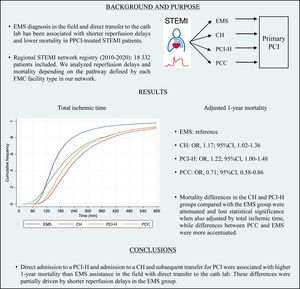
ResultsWe included 18 332 patients (EMS 34.3%; CH 33.5%; PCI-H 12.3%; PCC 20.0%). Patients with Killip-Kimball classes III-IV were: EMS 8.43%, CH 5.54%, PCI-H 7.51%, PCC 3.76% (P <.001). All comorbidities and first medical assistance complications were more frequent in the EMS and PCI-H groups (P <.05) and were less frequent in the PCC group (P <.05 for most variables). The PCI-H group had the shortest FMC-to-PCI delay (median 82 minutes); the EMS group achieved the shortest total ischemic time (median 151 minutes); CH had the longest reperfusion delays (P <.001). In an adjusted logistic regression model, the PCI-H and CH groups were associated with higher 1-year mortality, OR, 1.22 (95%CI, 1.00-1.48; P=.048), and OR, 1.17 (95%CI 1.02-1.36; P=.030), respectively, while the PCC group was associated with lower 1-year mortality than the EMS group, OR, 0.71 (95%CI 0.58-0.86; P <.001).
ConclusionsFMC with PCI-H and CH was associated with higher adjusted 1-year mortality than FMC with EMS. The PCC group had a much lower intrinsic risk and was associated with better outcomes despite longer revascularization delays.
Keywords
According to the European Society of Cardiology guidelines for the treatment of ST-elevation myocardial infarction (STEMI), STEMI treatment should be facilitated by regional hospital networks, linked by an efficient and prioritized ambulance service to provide access to primary percutaneous coronary intervention (PPCI) expeditiously and effectively to as many patients as possible.1
The efficiency of the STEMI network is crucial because long delays to PPCI are associated with worse prognosis.2,3 Specifically, system delay (time from first medical contact [FMC] to reperfusion) has been proven to be related to mortality and is also the most modifiable parameter.2 Therefore, rapid diagnosis and transfer to the catheterization laboratory (cath lab) of a primary PCI-capable hospital (PCI-H) is important and should be optimized regardless of the prehospital pathway followed.
In a given STEMI network, diagnosis and, therefore, system activation permitting early transfer to the cath lab of the PPCI hospital can be made in different facility types (ie, emergency medical services (EMS) assistance “in the field”, a community hospital [CH], a PCI-H, or a primary care center [PCC]), most of them requiring transfer to the PCI-H. The pathways determined by FMC facility type may be associated with different delays in reperfusion and, therefore, FMC with particular facility types may lead to better mortality results.
Previous studies mainly aimed to compare 2 different possible reperfusion pathways in STEMI (ie, EMS vs direct admission to PCI-H, transfer from a CH vs direct admission to PCI-H, etc).4–6
The present study sought to determine mortality results depending on FMC facility type considering all possible care pathways within our STEMI network. We evaluated a public health care system STEMI reperfusion network that aims to provide primary PCI to all STEMI cases in the region to determine whether mortality was lower in pathways with shorter delays than in those with longer delays, to prioritize the former.
METHODSThe regional STEMI network, Codi Infart, was launched in June 2009. This network aimed to enhance reperfusion therapy for all STEMI cases in Catalonia, a region of 32 000km2 with nearly 7.5 million inhabitants. To date, 11 hospitals in this region have gained PPCI capability. The Codi Infart network prioritizes PPCI as the first-choice reperfusion treatment, when the electrocardiogram-to-reperfusion time can be achieved in less than 120minutes. The network is coordinated by the EMS, which also conducts all transfers. The Codi Infart network comprises 4 care pathways depending on the FMC facility where the diagnosis is made: a) direct admission to a primary PCI-capable hospital (PCI-H); b) admission to a hospital or community hospital without PCI capability (CH); c) admission to a primary care center or general practitioner center (PCC); and c) EMS assistance and diagnosis “in the field” (EMS group). In the latter 3 groups, the EMS coordinates and carries out transfers from the FMC directly to the cath lab of a PCI-H (figure 1).
The Codi Infart STEMI network in Catalonia. A. Codi Infart pathways; B. Codi Infart operating area and 11 participating PCI-capable hospitals. Cath Lab, catheterization laboratory; CH, community hospital; EMS, emergency medical service; FMC, first medical contact; PCC, primary care centre; PCI-H, hospital with PCI capability.
Since the inception of the Codi Infart network, all cases have been recorded in a mandatory prospective multicenter registry maintained by the public health administration,7 which has been described elsewhere.8–11 The stored data include demographic variables, previous medical history variables, clinical information at the FMC such as Killip-Kimball class, potential medical complications at the first medical assistance such as ventricular fibrillation, ventricular tachycardia, atrial fibrillation and atrioventricular block, location of the infarct (ie, anterior, inferior, lateral), number of vessels affected, system-dependent factors, PCI and clinical data, and information on long-term all-cause mortality.
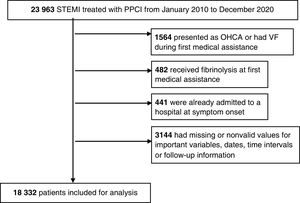
For the present study, we selected all patients with a confirmed STEMI (based on the criteria of ST-elevation in the FMC electrocardiogram determined by the FMC physician and confirmed by the physician of the PCI-H) that were treated with PPCI from January 2010 to December 2020. We excluded patients whose initial presentation was an out-of-hospital cardiac arrest, delayed arrivals (time from symptom onset to FMC> 12 hours), already admitted to a hospital at symptom onset, and those who resided outside the region (due to the inability to obtain follow-up information). Since information on presentation as an out-of-hospital cardiac arrest was only available from 2015, all patients with ventricular fibrillation at the FMC were also excluded to eliminate the strongest potential selection bias (out-of-hospital cardiac arrests are mainly assisted by EMS), and also considering that ventricular fibrillation could impact mortality more than reperfusion time.9 We also excluded patients who had received fibrinolysis at the FMC. Finally, we also excluded participants with invalid or missing values on classification variables, dates, time intervals or follow-up information. Data on the number of affected vessels were only available after 2012 and data from certain baseline characteristics were only available for the last few years.
Patients were grouped according to the FMC facility type (ie, EMS, CH, PCI-H, or PCC).
The primary end point was 1-year all-cause mortality. Secondary objectives included 30-day mortality, time from FMC to reperfusion, and total ischemic time. Mortality data were based on official mortality registries from both the Catalan and Spanish governments. The quality of data included in the registry is periodically verified by an external audit.
The FMC time with EMS was the moment the ambulance reached the patient, after the 112 call. For the remaining groups, FMC was the time of arrival at the emergency department of each facility. For the PCC, CH and PCI-H groups, patients mostly reached those facilities by themselves (especially in the case of PCCs), but they could also have been transferred by paramedical EMS units or by EMS with nondiagnostic electrocardiogram, following the criteria of the EMS physician. In these 3 groups, system delay was considered equivalent to time from FMC to PCI. The time of the EMS call was not available to calculate system delay for the EMS group. Therefore, comparisons between groups were made using the FMC-to-PCI time, symptoms-to-FMC time and total ischemic time.
All study procedures were in accordance with the Helsinki Declaration and Spanish data protection laws.
Statistical AnalysisCategorical variables are presented as absolute and relative frequencies (%). Continuous variables are described as mean±standard deviation (SD) or as the median and interquartile range [IQR], when the data were not normally distributed. Clinical variables and reperfusion times were compared between the groups with the chi-square test when normally distributed, for frequencies, and ANOVA was performed to compare means between more than 2 groups. Variables with nonnormal distributions were compared with nonparametric tests (Mann Whitney or Kruskal-Wallis, as appropriate). P-values <.05 were considered statistically significant. A Cox-proportional hazards model was initially tested to analyze the relationship between all-cause 1-year mortality and FMC facility type (the EMS group was set as reference). Nevertheless, the proportional hazards assumption was not fulfilled for many important covariates (ie, Killip class, sex, anterior STEMI) and, therefore, analyses were finally performed using multiple logistic regression. The model was adjusted with several covariates. The results are expressed as odds ratios (OR) and 95% confidence intervals (95%CI).
To better understand to what extent mortality differences between groups were explained by differences in reperfusion delays, total ischemic time was also introduced in an additional model as a covariate.
Finally, a sensitivity analysis was conducted to assess the robustness of our data regarding the potential effect of the COVID-19 pandemics. For this purpose, we repeated the delay and mortality analyses in patients for the years 2010-2019 and in patients for 2020 separately.
All analyses were performed using Stata/IC 16.1 software (Stata Corp, College Station, United States).
RESULTSWe identified 23 963 patients meeting the inclusion criteria from January 2010 to December 2020. Among these, 2487 were excluded because they had exclusion criteria and 3 144 patients had missing or invalid values on the above-mentioned variables. Thus, we finally included 18 332 patients in the analysis (a flowchart is shown in figure 2). Of these, 34.25% were attended by EMS in the field and directly transferred to the cath lab of a PCI-H, 33.47% were initially admitted to a CH, 12.28% were directly admitted to a PCI-H, and 20.01% were initially assisted in a PCC.
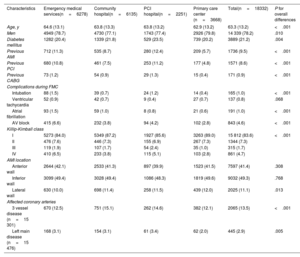
The groups showed important differences in clinical characteristics (table 1) and reperfusion times (table 2). The hospital-related groups (PCI-H and CH) had the highest proportions of women (P=.010) and patients with diabetes (P=.004). Previous episodes of PCI, myocardial infarction, coronary artery bypass grafting, and Killip-Kimball classes III-IV were much common in the PCI-H and EMS groups. The EMS group had the highest frequency of complications (ventricular tachycardia, atrial fibrillation, atrioventricular block, need for intubation) occurring during FMC assistance (P <.001 for most of them, P=.068 for ventricular tachycardia). The PCC group had the lowest risk profile regarding comorbidities and first medical assistance complications (lowest age, diabetes proportion, history of PCI, myocardial infarction or coronary artery bypass grafting, lowest Killip-Kimball class, lowest proportion of atrial fibrillation, intubation, and atrioventricular block at the first medical assistance; P <.05 for all these variables).
Baseline and clinical characteristics. Patients from 2010 to 2020
| Characteristics | Emergency medical services(n=6278) | Community hospital(n=6135) | PCI hospital(n=2251) | Primary care center (n=3668) | Total(n=18332) | P for overall differences |
|---|---|---|---|---|---|---|
| Age, y | 64.6 (13.1) | 63.8 (13.3) | 63.8 (13.2) | 62.9 (13.2) | 63.3 (13.2) | <.001 |
| Men | 4949 (78.7) | 4730 (77.1) | 1743 (77.4) | 2926 (79.8) | 14 339 (78.2) | .010 |
| Diabetes mellitus | 1282 (20.4) | 1339 (21.8) | 529 (23.5) | 739 (20.2) | 3889 (21.2) | .004 |
| Previous AMI | 712 (11.3) | 535 (8.7) | 280 (12.4) | 209 (5.7) | 1736 (9.5) | <.001 |
| Previous PCI | 680 (10.8) | 461 (7.5) | 253 (11.2) | 177 (4.8) | 1571 (8.6) | <.001 |
| Previous CABG | 73 (1.2) | 54 (0.9) | 29 (1.3) | 15 (0.4) | 171 (0.9) | <.001 |
| Complications during FMC | ||||||
| Intubation | 88 (1.5) | 39 (0.7) | 24 (1.2) | 14 (0.4) | 165 (1.0) | <.001 |
| Ventricular tachycardia | 52 (0.9) | 42 (0.7) | 9 (0.4) | 27 (0.7) | 137 (0.8) | .068 |
| Atrial fibrillation | 93 (1.5) | 59 (1.0) | 8 (0.8) | 21 (0.6) | 191 (1.0) | <.001 |
| AV block | 415 (6.6) | 232 (3.8) | 94 (4.2) | 102 (2.8) | 843 (4.6) | <.001 |
| Killip-Kimball class | ||||||
| I | 5273 (84.0) | 5349 (87.2) | 1927 (85.6) | 3263 (89.0) | 15 812 (83.6) | <.001 |
| II | 476 (7.6) | 446 (7.3) | 155 (6.9) | 267 (7.3) | 1344 (7.3) | |
| III | 119 (1.9) | 107 (1.7) | 54 (2.4) | 35 (1.0) | 315 (1.7) | |
| IV | 410 (6.5) | 233 (3.8) | 115 (5.1) | 103 (2.8) | 861 (4.7) | |
| AMI location | ||||||
| Anterior wall | 2644 (42.1) | 2533 (41.3) | 897 (39.9) | 1523 (41.5) | 7597 (41.4) | .308 |
| Inferior wall | 3099 (49.4) | 3028 (49.4) | 1086 (48.3) | 1819 (49.6) | 9032 (49.3) | .768 |
| Lateral wall | 630 (10.0) | 698 (11.4) | 258 (11.5) | 439 (12.0) | 2025 (11.1) | .013 |
| Affected coronary arteries | ||||||
| 3 vessel disease (n=15 301) | 670 (12.5) | 751 (15.1) | 262 (14.6) | 382 (12.1) | 2065 (13.5) | <.001 |
| Left main disease (n=15 476) | 168 (3.1) | 154 (3.1) | 61 (3.4) | 62 (2.0) | 445 (2.9) | .005 |
PCI, primary coronary intervention; AMI, acute myocardial infarction; CABG, coronary-aortic bypass grafting; FMC, first medical contact; SD, standard deviation; COPD, chronic obstructive pulmonary disease.
Values are expressed as No. (%).
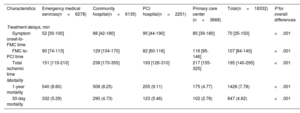
Delays to reperfusion and mortality depending on first medical care facility type. Patients from the entire study period
| Characteristics | Emergency medical services(n=6278) | Community hospital(n=6135) | PCI hospital(n=2251) | Primary care center (n=3668) | Total(n=18332) | P for overall differences |
|---|---|---|---|---|---|---|
| Treatment delays, min | ||||||
| Symptom onset-to-FMC time | 52 [30-100] | 88 [42-180] | 95 [44-190] | 85 [39-180] | 70 [35-150] | <.001 |
| FMC-to-PCI time | 90 [74-113] | 129 [104-170] | 82 [60-116] | 116 [95-146] | 107 [84-140] | <.001 |
| Total ischemic time | 151 [119-210] | 238 [170-355] | 193 [126-310] | 217 [155-325] | 195 [140-295] | <.001 |
| Mortality | ||||||
| 1-year mortality | 540 (8.60) | 506 (8.25) | 205 (9.11) | 175 (4.77) | 1426 (7.78) | <.001 |
| 30-day mortality | 332 (5.29) | 290 (4.73) | 123 (5.46) | 102 (2.78) | 847 (4.62) | <.001 |
PCI, primary coronary intervention; FMC, first medical contact.
Values are expressed as No. (%) or median [interquartile range].
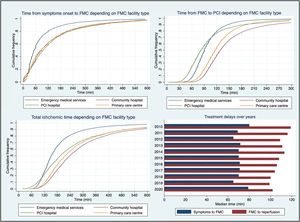
The shortest delay from FMC to reperfusion was observed in the PCI-H group (median 82minutes, P <.001), but the shortest total ischemic time was achieved by the EMS group (median 151minutes, P <.001). The CH group had the longest reperfusion times (FMC-to-PCI delay 129minutes, total ischemic time 238 minutes; P <.001 for both) (table 2, figure 3A-C).
Reperfusion delays. A. Cumulative frequencies of symptom-to-FMC delay depending on FMC facility type. B. Cumulative frequencies of FMC-to-PCI delay depending on FMC facility type. C. Cumulative frequencies of total ischemic time depending on FMC facility type. D. Median symptom-to-FMC and FMC-to-PCI delays over the years (in the global population). FMC, first medical contact; PCI, primary coronary intervention.
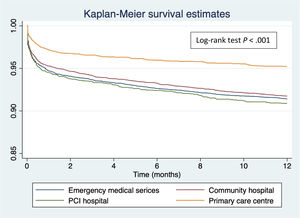
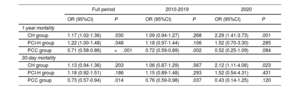
Crude 1-year all-cause mortality was higher in the PCI-H group (9.11%) and in the EMS group (8.60%) than in the CH (8.25%) and PCC (4.77%) groups (log-rank test P <.001) (table 2, figure 4). In a logistic regression model adjusting for covariates (ie, age, sex, diabetes, previous acute myocardial infarction, anterior location of STEMI, Killip-Kimball class, ventricular tachycardia in FMC) with the EMS group set as reference (because its shorter total ischemic time), the PCI-H (OR, 1.22; 95%CI 1.00-1.48; P=.048) and CH (OR, 1.17; 95%CI 1.02-1.36; P=.030) groups were associated with higher 1-year mortality, while the PCC group remained associated with lower 1-year mortality (OR, 0.71; 95%CI 0.58-0.86; P=.001) compared with the EMS group. In an additional model also adjusted for total ischemic time, mortality differences in the PCI-H and CH groups compared with the EMS group were attenuated and lost statistical significance (OR for CH was 1.09; 95%CI 0.94-1.27; P=.254 and OR for PCI-H was 1.17; 95%CI 0.97-1.43; P=.109), while mortality differences in the PCC group compared with EMS slightly increased (OR, 0.67; 95%CI 0.55-0.81; P <.001).
Differences in 30-day mortality were less pronounced. Table 2 shows unadjusted 30-day mortality. In the logistic regression analysis adjusted for the same covariates, only a trend toward higher mortality was observed in CH and the PCI-H groups compared with the EMS group (OR, 1.13; 95%CI 0.94-1.36; P=.203 and OR, 1.18; 95%CI 0.92-1.51%; P=.186). Conversely, the PCC group (OR, 0.73; 95%CI 0.57-0.94; P=.014) was associated with lower mortality than the EMS group.
Impact of COVID-19 pandemicsWhen we excluded patients from 2020 and analyzed patients from 2010 to 2019, adjusted mortality differences were attenuated. Crude 1-year mortality was 8.90% for the EMS group, 7.99% for the CH group, 9.30% for the PCI-H group and 5.04% for the PCC group. In the logistic regression analysis adjusted for the same covariates, mortality differences disappeared for CH (OR, 1.09; 95%CI, 0.94-1.27; P=.268) and only a trend toward higher mortality was observed for PCI-H (OR, 1.18; 95%CI, 0.97-1.44; P=.106), whereas the PCC group remained associated with lower 1-year mortality (OR 0.72; 95%CI, 0.59-0.89; P=.002) compared with the EMS group.
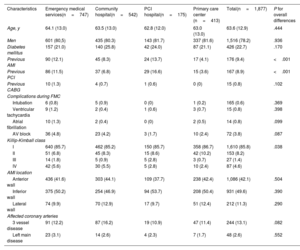
Data from 2020 showed some differences in the profile of patients in each group compared with the previous period (table 3). A total of 1877 patients were treated in 2020 (1871 in 2019), and group distribution was as follows: EMS 39.8%, CH 28.9%, PCI-H 9.32% and PCC 22.0%. In this period, and unlike the previous period, patients in the CH group had a risk profile very similar to EMS group regarding Killip-Kimball class or complications at first medical assistance (P=.038 for Killip class). The PCC group continued to have the lowest risk profile. In 2020, time from symptom onset to FMC was longer but the medians of FMC-to-reperfusion time did not differ from previous years (figure 3D), following the same pattern described for the entire period: PCI-H with the shortest FMC-to-PCI time (78 minutes), EMS with the shortest total ischemic time (156 minutes) and CH with the longest reperfusion times (FMC-to-PCI 120minutes, total ischemic time 238 minutes) (P <.001 for all of them; table 4). Unadjusted 1-year mortality is shown in table 4. The logistic regression analysis showed, compared with the EMS group, a higher mortality in CH group (OR, 2.29; 95%CI, 1.41-3.73; P=.001), no significant differences in the PCI-H group (OR, 1.52; 95%CI, 0.70-3.30; P=.285), and a trend toward lower mortality in PCC group (OR, 0.52; 95%CI, 0.25-1.09; P=.084). Table 5 shows the results of logistic regressions for all periods, for both 1-year and 30-day mortality, and figure 5 summarizes the key findings of this study.
Baseline and clinical characteristics. Patients from 2020
| Characteristics | Emergency medical services(n=747) | Community hospital(n=542) | PCI hospital(n=175) | Primary care center (n=413) | Total(n=1,877) | P for overall differences |
|---|---|---|---|---|---|---|
| Age, y | 64.1 (13.0) | 63.5 (13.0) | 62.8 (12.0) | 63.0 (13.0) | 63.6 (12.9) | .444 |
| Men | 601 (80,5) | 435 (80.3) | 143 (81.7) | 337 (81.6) | 1,516 (78.2) | .936 |
| Diabetes mellitus | 157 (21.0) | 140 (25.8) | 42 (24.0) | 87 (21.1) | 426 (22.7) | .170 |
| Previous AMI | 90 (12.1) | 45 (8.3) | 24 (13.7) | 17 (4.1) | 176 (9.4) | <.001 |
| Previous PCI | 86 (11.5) | 37 (6.8) | 29 (16.6) | 15 (3.6) | 167 (8.9) | <.001 |
| Previous CABG | 10 (1.3) | 4 (0.7) | 1 (0.6) | 0 (0) | 15 (0.8) | .102 |
| Complications during FMC | ||||||
| Intubation | 6 (0.8) | 5 (0.9) | 0 (0) | 1 (0.2) | 165 (0.6) | .369 |
| Ventricular tachycardia | 9 (1.2) | 2 (0.4) | 1 (0.6) | 3 (0.7) | 15 (0.8) | .398 |
| Atrial fibrillation | 10 (1.3) | 2 (0.4) | 0 (0) | 2 (0.5) | 14 (0.8) | .099 |
| AV block | 36 (4.8) | 23 (4.2) | 3 (1.7) | 10 (2.4) | 72 (3.8) | .087 |
| Killip-Kimball class | ||||||
| I | 640 (85.7) | 462 (85.2) | 150 (85.7) | 358 (86.7) | 1,610 (85.8) | .038 |
| II | 51 (6.8) | 45 (8.3) | 15 (8.6) | 42 (10.2) | 153 (8.2) | |
| III | 14 (1.8) | 5 (0.9) | 5 (2.8) | 3 (0.7) | 27 (1.4) | |
| IV | 42 (5.6) | 30 (5.5) | 5 (2.8) | 10 (2.4) | 87 (4.6) | |
| AMI location | ||||||
| Anterior wall | 436 (41.6) | 303 (44.1) | 109 (37.7) | 238 (42.4) | 1,086 (42.1) | .504 |
| Inferior wall | 375 (50.2) | 254 (46.9) | 94 (53.7) | 208 (50.4) | 931 (49.6) | .390 |
| Lateral wall | 74 (9.9) | 70 (12.9) | 17 (9.7) | 51 (12.4) | 212 (11.3) | .290 |
| Affected coronary arteries | ||||||
| 3 vessel disease | 91 (12.2) | 87 (16.2) | 19 (10.9) | 47 (11.4) | 244 (13.1) | .082 |
| Left main disease | 23 (3.1) | 14 (2.6) | 4 (2.3) | 7 (1.7) | 48 (2.6) | .552 |
PCI, primary coronary intervention; AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; FMC, first medical contact; SD, standard deviation.
Values are are expressed as No. (%).
Delays to reperfusion and mortality depending on FMC facility type in 2020
| Characteristics | Emergency medical services(n=747) | Community hospital(n=542) | PCI hospital(n=175) | Primary care center (n=413) | Total(n=1,877) | P for overall differences |
|---|---|---|---|---|---|---|
| Treatment delays | ||||||
| Symptom onset-to-FMC time | 59 [30-113] | 90 [45-181] | 109 [46-205] | 108 [47-211] | 79 [37-165] | <.001 |
| FMC-to-PCI time | 90 [73-110] | 120 [99-158] | 78 [60-107] | 112 [93-135] | 102 [82-130] | <.001 |
| Total ischemic time | 156 [120-225] | 238 [167-358] | 204 [124-335] | 233 [158-346] | 195 [137-297] | <.001 |
| Mortality | ||||||
| 1-year mortality | 48 (6.43) | 59 (10.89) | 12 (6.86) | 11 (2.66) | 130 (6.93) | <.001 |
| 30-day mortality | 30 (4.02) | 33 (6.09) | 7 (4.00) | 5 (1.21) | 75 (4.00) | .002 |
FMC, first medical contact; PCI, percutaneous coronary intervention.
Values are expressed as No. (%) or median [interquartile range].
Multiple logistic regressions for 30-day and 1-year mortality in the full period, from 2010 to 2019 and in 2020
| Full period | 2010-2019 | 2020 | ||||
|---|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | |
| 1-year mortality | ||||||
| CH group | 1.17 (1.02-1.36) | .030 | 1.09 (0.94-1.27) | .268 | 2.29 (1.41-3.73) | .001 |
| PCI-H group | 1.22 (1.00-1.48) | .048 | 1.18 (0.97-1.44) | .106 | 1.52 (0.70-3.30) | .285 |
| PCC group | 0.71 (0.58-0.86) | <.001 | 0.72 (0.59-0.89) | .002 | 0.52 (0.25-1.09) | .084 |
| 30-day mortality | ||||||
| CH group | 1.13 (0.94-1.36) | .203 | 1.06 (0.87-1.29) | .567 | 2.12 (1.11-4.06) | .023 |
| PCI-H group | 1.18 (0.92-1.51) | .186 | 1.15 (0.89-1.48) | .293 | 1.52 (0.54-4.31) | .431 |
| PCC group | 0.73 (0.57-0.94) | .014 | 0.76 (0.59-0.98) | .037 | 0.43 (0.14-1.25) | .120 |
Reference group: EMS. Adjusted for covariates: age, sex, diabetes, previous acute myocardial infarction, anterior STEMI location, Killip-Kimball class (as a categorical variable with 4 categories with Killip I as reference), and ventricular tachycardia at first medical assistance. CI, confidence interval; EMS, emergency medical service; FMA, first medical assistance; OR, odds ratio; PCC, primary care center; PCI-H, hospital with percutaneous coronary intervention capability; STEMI, ST-elevation myocardial infarction; VT, ventricular tachycardia.
Central illustration. Impact of first medical contact facility type on ischemic time and 1-year mortality. CH, community hospital; EMS, emergency medical services; PPCI, primary percutaneous coronary intervention; PCC, primary care center; PCI-H, primary percutaneous coronary intervention hospital; STEMI, ST-elevation myocardial infarction.
The Codi Infart registry provided an excellent opportunity to examine the performance of a public health care system STEMI network that covers an entire territory and, therefore, must attempt to offer the fastest route to reperfusion to all inhabitants of the region, independently of the FMC facility type and location. We evaluated the prognostic impact of the FMC facility type and the reperfusion delays of the derived network pathways.
The main finding of this study was that direct admission to a PCI-H and admission to a CH and subsequent transfer to the PCI-H were associated with higher adjusted 1-year mortality than EMS assistance “in the field” with direct transfer to the cath lab of the PCI-H. The EMS group also had the shortest total ischemic time, and an FMC-to-reperfusion time not too dissimilar from the PCI-H group (medians: 90 vs 82min, respectively). These mortality differences, although weak, especially in the case of the PCI-H group (P=.048), were observed even though the EMS group had the highest rate of complications in the first medical assistance, reflecting the much higher STEMI risk profile associated with EMS use, also described in previous studies.12,13 Furthermore, the attenuation of these differences after adjustment also by total ischemic time supports the notion that the mortality benefit in the EMS group was at least partially driven by shorter reperfusion delays, especially compared with the CH group, which showed the largest attenuation in the association when total ischemic time was added to the model. On the other hand, the PCC group was associated with better 1-year outcomes than the EMS group despite longer delays (FMC-to-PCI delay: 116 vs 90min, total ischemic time: 217 vs 151minutes, respectively), a finding that could be explained by the much lower risk profile in terms of patient baseline characteristics and STEMI risk in the PCC group. Indeed, the higher mortality differences when adjustment was also performed by total ischemic time support this hypothesis.
The fact that the PCI-H group was associated with worse prognosis even though this group had the shortest FMC-to-PCI delay deserves some comments. First, as shown in figure 3B, in patients with FMC-to-PCI delay> 105minutes in the PCI-H and EMS groups (that is, 30% of the patients in both groups), the latter had, in fact, better results. Second, although system delay has classically been the focus of attention as the most modifiable parameter and because of its more linear relationship with mortality as it is less influenced by selection biases, there is sufficient evidence to believe that achieving a shorter total ischemic time should be a priority rather than focusing only on system delay.14 In this matter, it is worth noting that part of the shorter total ischemic time in the EMS group was due to the provision of early assistance in the field and shortening the symptom-to-FMC time (figure 3A), considered a patient delay in the other pathways, but being, in fact, due to the system. Third, patients in the PCI-H group had slightly worse baseline characteristics than those in the EMS group, which could have contributed to the differences in 1-year mortality; indeed, this is endorsed by the lower change in mortality differences when adjustment was also performed by total ischemic time.
The impact of the COVID-19 pandemics on our analysis also needs to be discussed. Apparently, the benefit on mortality in favor of the EMS group was strongly related to the weight of 2020, since the analysis excluding this year showed attenuation of the differences, especially with the CH group, and since the mortality benefit in 2020 for EMS in comparison to CH group was marked. There are many reasons for considering this year unique, such as the longer symptom-to-FMC delays, which could be explained by the patients’ fear of being admitted to a hospital, the lower proportions of STEMI-treated patients during the first wave,15 and the modified risk profile distribution regarding FMC facilities, exemplified by the higher proportions of Killip-Kimball classes III-IV in CH during this year. Nevertheless, time from FMC to PCI was not significantly different from previous years,16,17 the number of patients treated during the entire year was almost equal to that in 2019 and, most important, we cannot omit this year, since it also reflects the performance of our health care system and because the pandemics or its consequences are not yet over.
Indeed, the analysis of 2020 provides valuable information that may contribute to a better understanding of other results of the study: despite the logical benefit of improving PCI delays, numerous studies have attempted to demonstrate that direct admission to a PCI-H and a transfer “from the field” directly to the cath lab were associated with a better prognosis compared with a diagnosis and transfer from facilities without PCI capabilities; however, the results of those studies were fairly variable.4,5,18–23 The mortality benefit with the reduction of treatment delay proven in studies comparing prehospital and in-hospital fibrinolysis24,25 is far more difficult to demonstrate in the current setting of PPCI26 given that current studies remain subject to the confounding and selection biases inherent to registry data. Nevertheless, the COVID-19 pandemics actually modified the risk profile associated with the CH group and made it more similar to that of the EMS group. Therefore, the resulting association of the CH group with higher mortality in this period could be explained by patients in that group having a higher risk similar to those initially treated by the EMS but being associated with longer reperfusion times. Conversely, patients in the PCC group continued to have both the lowest risk baseline characteristics and lowest Killip-Kimball class and complications. Hence, outcomes in this group were probably less delay-dependant due to its intrinsic low mortality.13
The fact that differences between groups were much lower in 30-day than in 1-year mortality was an expected finding considering that the benefit of a higher proportion of myocardial salvage by reduced total ischemic time not only determines complications and mortality during admission but also long-term complications; in addition, the lack of events due to a shorter follow-up period may partially explain the lower differences; therefore, it is likely that a longer period of time than 30 days is needed to demonstrate this benefit.
Regarding delays in reperfusion, the best results were irrefutably achieved in the EMS group: it was associated with a shorter symptom-to-FMC time than the other groups, with an FMC-to-PCI delay not far from that of the PCI-H group and with the shortest total ischemic time. Indeed, 50% of patients in this group achieved an FMC-to-reperfusion time <90minutes. Concerning the shorter time from symptom onset to FMC, and considering that early presenters have been previously associated with worse outcomes,27,28 the good demonstrated results of this pathway constitute a valuable opportunity to provide prompter revascularization and improved prognosis to a high risk group. In contrast, only 40% of patients in the CH group had a system delay <120minutes. The present analysis should prompt more extensive studies about sources of delay in the PCC group but especially in the CH group of the network to improve them. Therefore, and taking into consideration the findings of this study, the use of EMS as the FMC in STEMI should be greatly boosted bypassing the CH and PCC facilities. Thus, awareness-raising campaigns are needed to tend to the higher rates (50%-70%) of field-triage by EMS described in some studies.12,13,29 For that purpose, it will also be necessary for public administrations to support this strategic objective of public health both logistically and economically.
Our findings serve to reinforce the pursuit of shorter total ischemic times and not only focus on system delays, a goal that EMS can achieve better than any other FMC facility type. Moreover, our study exemplifies how selection biases can hinder the association of clearly and directly related parameters such as total ischemic time and mortality, and shift the focus and efforts to more bias-free and measurable ones such as system delay. Perhaps more long-term strategies to increase public awareness will be able to significantly reduce the forgotten components of total ischemic time.
Study LimitationsAll observational and nonrandomized studies are subject to biases and our analysis is no exception. First, there might be additional characteristics not available for the present analysis that influenced prognosis in our groups and whose absence partially explains the observed results.30 Second, the exclusion of patients with missing data introduced a selection bias that cannot be corrected. Third, the results during COVID-19 pandemics may also have additional interpretations. Finally, the variable that determined if a patient was already admitted to a hospital at symptom onset was only available from 2015 onward; the manner and extent of impact of this partial exclusion on our results is unknown to us.
CONCLUSIONSIn this comprehensive, real-life evaluation of the impact of FMC facility type on prognosis and reperfusion delays in a public health care system STEMI network, FMC with EMS was associated with shorter total ischemic time than any other pathway, accounting for higher adjusted 1-year mortality in the PCI-H and CH groups compared with EMS. FMC with PCCs, despite longer reperfusion delays, was associated with better outcomes, probably of because the intrinsic low risk characteristics of this group of patients. Public campaigns to enhance awareness are required to reduce patient delay and emphasize the need to contact the EMS when faced with MI-compatible symptoms.
FUNDINGThis study was supported by the Catalan Health Service, Generalitat de Catalunya.
AUTHORS’ CONTRIBUTIONSO. de Diego takes responsibility for all aspects of the reliability and lack of bias of the data and their discussion. O. de Diego: data collection, statistical analysis, manuscript drafting, final approval.
C. García-García, J. Lupón, F. Rueda, X. Carrillo, R. Andrea: data collection, contributions to statistical analysis and manuscript drafting, final approval.
T. Oliveras, N. El Ouaddi, J. Serra, C. Labata, M. Ferrer, M. J. Martínez-Membrive, S. Montero, J. Mauri, J. García-Picart, S. Rojas, A. Ariza, H. Tizón-Marcos, M. Faiges, M. Cárdenas, R. M. Lidón, J. F. Muñoz-Camacho, X. Jiménez Fàbrega, J. Lupón, A. Bayés-Genís: data collection, critical review of the manuscript, final approval.
CONFLICTS OF INTERESTThis research work has no relationships with industry.
Many studies have assessed the mortality impact of the type of FMC in STEMI networks by comparing 2 different options (mainly FMC with EMS vs direct admission to a PCI hospital and direct admission to a PCI hospital vs interhospital transfer) but a direct comparison of all possible pathways in a given STEMI network is needed to improve its performance.
WHAT DOES THIS STUDY ADD?We found that STEMI patients assisted by the EMS as the FMC achieved shorter total ischemic times than any other pathway, not only by shortening FMC-to-PCI time but also by being the only circuit that shortened symptom-to-FMC delay. FMC with EMS was associated with better 1-year outcomes than direct admission to a PCI hospital or FMC to a community hospital. An in-depth analysis of the performance of STEMI networks and public health care strategies should be endorsed to reduce all components of treatment delay in STEMI and to optimize all possible pathways by boosting EMS as the FMC and improving the slower circuits.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2022.12.010