To the Editor:
Cholesterol pericarditis, first described in 1919 by Alexander and characterized by the presence of abundant microscopic cholesterol crystals in the pericardial fluid, is an uncommon disease, with fewer than 100 cases so far reported. While 49% are idiopathic, the remainder are associated with hypothyroidism, tuberculosis, rheumatoid arthritis and, very occasionally, with renal polycytosis, heart failure, myocardial infarction, and metastatic carcinomas.1 The case presented here was one of cholesterol pericarditis and hypothyroidism that led to pericardial constriction and required pericardiectomy, which is a very unusual course for this disease.2
The patient was a 64 year old man, who was admitted with a right, frontal parenchymatous hematoma secondary to trauma, and in whom cardiomegaly and severe pericardial effusion were detected. Primary hypothyroidism was diagnosed and treatment was started with thyroxine. At the time of discharge, the patient had no apparent neurologic sequelae, with normalization of the thyroid function. Six months later, he was readmitted with continued effusion in spite of being euthyroid. He was afebrile and eupneic. Physical examination showed jugular ingurgitation, no paradoxical pulse, bibasal pulmonary hypoventilation, mild painful hepatomegaly, and minimal pitting edema. An electrocardiogram showed a sinus rhythm of 100 bpm, low voltages, and a nonspecific repolarization alteration. Chest radiography revealed marked cardiomegaly.
The laboratory tests showed an ESR of 72 mm/h and normochromic normocytic anemia. Kidney and liver function tests, glycemia, cholesterol, and triglycerides were all normal. Tumor markers, C reactive protein (CRP), rheumatoid factor, troponin I, HIV, antinuclear, anticytoplasm and antithyroid antibodies, and antitoxoplasm serology, anti-Coxiella and anti-Brucella were all negative. The thyroid hormones were normal. The echocardiogram confirmed a massive pericardial effusion, abundant fibrin aggregates, right atrial collapse, and dilation of the inferior vena cava (25 mm, with no respiratory variations) and the suprahepatic veins.
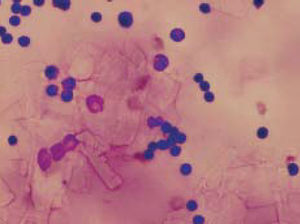
Twenty-four hours after admission the patient underwent subxiphoid pericardiocentesis, extracting 1300 mL of an orange colored serous fluid, compatible with the exudate, with abundant cholesterol crystals (Figure 1). The cultures, cytologies, ADA, Ziehl-Neelsen and Lowenstein stains, and CRP for M tuberculosis, and generic mycobacteria were all negative.
Figure 1. Cytology of the pericardial fluid showing abundant, rectangular crystals corresponding to cholesterol crystals and inflammatory cells consisting of lymphocytes and macrophages (Giemsa, ×400).
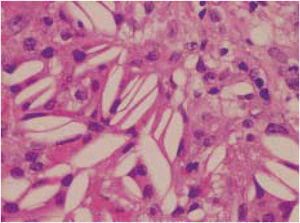
An infectious process, a tumor, or an underlying immunologic disorder were all ruled out. Because of the persistence of the effusion, the intermittent fever and the constitutional syndrome, a pericardial biopsy was performed 21 days after admission for an etiologic study.3 The data from the pathologic study included a markedly enlarged pericardium due to fibrosis, accumulations of cholesterol crystals and a granulomatous, inflammatory reaction (cholesterol granuloma) (Figure 2). The CRP for M tuberculosis and generic mycobacteria was undetectable.
Figure 2. Pericardial biopsy showing cholesterol crystals, which adopt a characteristic long shape with pointed ends, visible in the interstitium and the cytoplasm of giant cells (HE, ×400).
The patient presented progressive symptoms of pericardial constriction (increased hepatomegaly, edema, and bilateral pleural effusion, which required several thoracocentesis for evacuation). The echocardiographic study confirmed the presence of constriction. Seven weeks after admission he underwent a total pericardiectomy, with no complications.4 The pathological study of the specimen was similar to the previous report and confirmed the pericarditis due to cholesterol crystals.
At the time of writing, 6 months after the pericardiectomy, the patient is asymptomatic and only receiving replacement hormone therapy.
Pericardial effusion due to cholesterol crystals is usually massive, but well tolerated as its progression is slow, rarely evolving to tamponade or constriction.2 Our case is particularly interesting because the patient eventually required pericardiectomy, as indicated in the guidelines.5,6 The increase in cholesterol in the pericardial fluid may lead to the formation of crystals by precipitation, which are then deposited in the pericardium and provoke a granulomatous foreign body reaction, perpetuating the inflammation and the effusion.