Pharmacological challenge tests with sodium channel blockers (SCBs) may have unexpected diagnostic applications in syncope with diagnostic uncertainty.
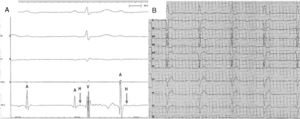
We present the case of a 72-year-old woman who attended the emergency room after syncope of cardiogenic origin (which occurred while the patient was sitting, with no warning signs, and with complete recovery). The only personal history of note was that her son had died suddenly of unknown causes and there had been no autopsy. The initial workup, including echocardiography, showed no abnormal findings except the presence in the ECG of a QRS interval of 100ms with a type 3 Brugada pattern (figure 1) and no significant changes in the high leads.
Given the patient's family history, a pharmacological challenge test was undertaken to rule out Brugada syndrome (flecainide 2mg/kg for 10minutes). During the procedure, no changes were observed in the ST segment in V1 or V2. However, without any prior QRS widening, the patient developed atrioventricular block (AVB), initially second degree but which progressed to complete block (figure 1B). Flecainide perfusion was suspended and a tetrapolar catheter was introduced into the right ventricle via right femoral puncture. This catheter could record His bundle activity and confirmed that AVB was infranodal (figure 2A). Given that complete AVB persisted, the catheter was left at the apex of the right ventricle to provide pacing as a temporary pacemaker. The patient was transferred to the coronary unit. After more than 24hours of monitoring, the complete AVB did not resolve and so a permanent pacemaker was implanted. At 3 years’ follow-up, the patient was asymptomatic (with no recurrences of syncope) and still required pacing from the pacemaker, as complete AVB persisted (figure 2B).
Pharmacological challenge tests with SCBs (normally ajmaline or flecainide, and occasionally procainamide) are usually used to unmask the electrocardiographic pattern of type 1 Brugada syndrome in undiagnosed cases (syncope of diagnostic uncertainty, family screening).1,2 SCBs are also recommended by the clinical practice guidelines for cases of syncope with bifascicular block and HV interval <70ms, with the aim of uncovering disorders in the His-Purkinje system.1 Traditionally, procainamide or, less frequently, ajmaline, is recommended.1,3,4 However, a recent study has shown that flecainide could be more sensitive than procainamide for uncovering His-Purkinaje involvement in these patients.5 Pacemaker placement is indicated if, after administration of SCBs, HV prolongation is> 100ms or if second or third degree infranodal AVB occurs,3,5 as was the case in our patient.
It has been demonstrated that SCBs can be safely used in pharmacological challenge tests, although they might trigger ventricular arrhythmias or transient AVB, particularly in patients with prior atrioventricular or intraventricular conduction abnormalities.5,6 To prevent the onset of AVB, most authors recommend terminating pharmacological challenge when QRS widening> 30% is observed.6 To date, the conduction abnormalities described resulting from use of group Ic antiarrhythmic agents (flecainide, propafenone) have been transient, with a maximum duration in line with the half-life of the drug (≈ 6hours in the case of flecainide, but possibly as long as 58hours in patients with chronic kidney disease).
In the case presented here, it is notable that AVB occurred during the flecainide test with no prior QRS widening despite being infranodal (indicating that AVB in this case was probably intra-Hisian). Also of note is that AVB was permanent and not transient, as reported in previous literature, with the need for a permanent pacemaker.
In short, we believe that flecainide unmasked a disorder in the His-Purkinje system as the cause of the syncope. This case, therefore, highlights the question of whether a pharmacological challenge test with SCBs should be performed in cases of syncope of unknown cause with prolonged QRS but <120ms (incomplete block of the left or right branch, hemiblocks) to uncover abnormalities of His-Purkinaje conduction as the cause of syncope.
.