Correct electrocardiography (ECG) interpretation is essential to accurately diagnose cardiovascular disease.1,2
In everyday clinical practice, medical practitioners are faced with asymptomatic patients, in whom ECG findings play a critical role.4 This is particularly relevant at the first medical contact, when the treating physician may not be a cardiologist.2,3 The diagnostic capacity of ECG for detecting serious clinical conditions has been extensively validated, but no study has analyzed physicians’ abilities to interpret the ECGs.
Our objective was to investigate the ability of noncardiologist specialist physicians and residents to interpret potentially fatal ECG tracings, taking into account their diagnosis and their subjective perception of the seriousness of the findings.
We distributed a questionnaire to the participants of an electrocardiography course for physicians from different healthcare facilities and specialties, which took place in a tertiary hospital. The questionnaire was distributed arbitrarily, following the layout of the classroom. The questionnaire contained 10 diagnostic tracings of potentially fatal conditions that can present with different signs and symptoms, although all patients were asymptomatic at the time of recording. The ECGs had been selected by a group of clinical cardiologists in advance. There were several different questionnaire models, with the tracings arranged in a different order to avoid potential exchange of information between participants.
We asked attendees for their diagnosis and a subjective evaluation of the seriousness of the ECG findings, on a scale of 0 (benign) to 100 (fatal). Prior to this, 2 specialist cardiologists had assessed the possible diagnoses and their seriousness. Concordance was excellent between the cardiologists for the subjective evaluation of seriousness, as demonstrated by the intraclass correlation coefficient (0.92; confidence interval, 0.66-0.98) (Figure).
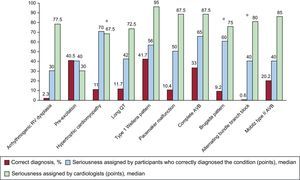
Percentage of correct diagnoses, median seriousness score assigned by the participants who correctly diagnosed the condition, and median seriousness score assigned by the cardiologists. AVB, atrioventricular block; RV, right ventricular.*Insignificant differences between the median seriousness score assigned by the participants and by the cardiologists (P > .05).
For each ECG, 2 points were awarded to each participant who correctly identified the condition, 1 point was awarded to those who accurately evaluated the seriousness, and 0 points were awarded to those with completely incorrect responses. Consequently, each participant could score a possible maximum of 30 points (3 for each ECG multiplied by 10 ECG in total).
In total, 163 physicians participated in the study: 117 were women (71.8%), 112 were residents (68.7%), and the median age was 27 years. Of the residents, 56 (50%) were second-year residents, and 31 (27.6%) were third-year residents. Twenty-eight (17.2%) were primary care physicians and 23 (14.1%) were emergency physicians (in these last 2 groups, the median age was 44 years).
The mean participant score for correct diagnosis was remarkably low at 6 points. There were no differences between the sexes (P = .47) or type of physician (residents, primary care physicians, and emergency physicians) (P = .21).
The percentage of correct diagnoses was extremely low for all 10 ECGs. It ranged from 0.6% for alternating bundle branch block to 41.7% for the classic pattern of Wellens syndrome (which signifies a critical lesion in the left anterior descending artery).
Figure shows the percentage of correct diagnoses. It also shows the median score assigned to each ECG by the physicians who correctly diagnosed the condition, based on their subjective perception of seriousness, as well as the median score assigned by the cardiologists, for comparison. The correlation was zero for the subjective evaluation of seriousness between the cardiologists and the participants that correctly diagnosed the condition (-0.09; confidence interval, -0.24 to 0.33).
There were statistically significant differences in the subjective perception of seriousness between the participants and the experts for most of the ECGs. The exceptions were the ECGs showing hypertrophic cardiomyopathy, Brugada pattern, and alternating bundle branch block (Figure).
Of note was a tracing with a QT interval of 580ms, which received a median seriousness score of 42 (0-100) from the participants who diagnosed it correctly, compared with 72.5 (70-75) from the cardiologists.
For Wellens syndrome, the median seriousness score from the participants was 56 (20-100), while the cardiologists assigned a score of 90.
Of the bradyarrhythmias, 2 deserve comment: complete atrioventricular block and Mobitz type II second degree atrioventricular block. Complete atrioventricular block was correctly identified by just 33%, with a median seriousness score of 65 (20-100) vs 87.5 (85-90) according to the experts. Mobitz type II was correctly diagnosed by 20.2% of participants, with a median seriousness score of 40 (10-90) compared with 85 (80-90) from the cardiologists.
Figure shows how similar discrepancies occurred in the interpretation of all 10 ECG tracings.
Despite the fundamental role played by ECG in the diagnosis of cardiovascular disease, these findings demonstrate that ECG interpretation is in need of remedial action, particularly for physicians who are the first medical contact. This conclusion is in line with the findings of other available studies.3
Our study shows an extremely low percentage of correct diagnoses and poor recognition of electrocardiographic patterns in the population analyzed.
Another even more shocking finding of this study is the incorrect perception of seriousness for several potentially fatal cardiovascular conditions that are diagnosed primarily from ECG. On many occasions, these were considered harmless, highlighting the need for training programs for such physicians on the correct interpretation of ECGs.