To the Editor:
Ventricular septal defect (VSD) following closed thoracic trauma is an unusual complication,1,2 that generally has a delayed diagnosis. We present the case of an 18-year-old male who suffered severe thoracic trauma with bilateral pleural effusion, lacerations of abdominal viscera and bone fractures following a road traffic accident. He was intubated for hypovolaemic shock and had multiple transfusions, required splenectomy, repair of liver lacerations and surgical re-exploration due to haemorrhage.
Upon admission, no heart murmurs were detected, the electrocardiogram revealed sinus tachycardia with Q-waves in II, III, and aVF and the maximum troponin-T was 2.33 ng/mL. The initial creatine kinase (CK) (1017 U/L; CK-MB, 79 U/L) increased to a maximum of 2510 U/L (CK-MB, 65 U/L) 24 hours later. The transthoracic echocardiogram (TTE) revealed a contusion of the interventricular septum (IVS), slightly thickened from the middle third to the apex and a reduction in movement, a slightly dilated right ventricle, and a pulmonary artery pressure of 50 mm Hg.
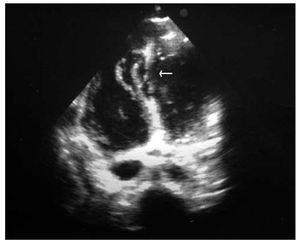
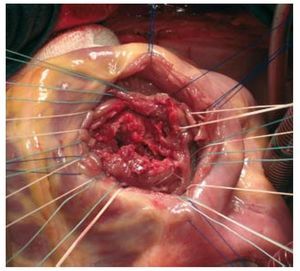
At 24 hours, a proto-mesosystolic murmur was heard at the left sternal border and haemodynamic instability, tachycardia, and the need for vasoactive drugs persisted. High oxygen saturation in the pulmonary artery (PA) led to the suspicion of a VSD, which was confirmed by TTE. Severe dilation of the right ventricle was seen with mild systolic dysfunction, the appearance of an apical pseudoaneurysm and a large irregular longitudinal VSD in the mid-distal portion of the IVS (Figure 1). He underwent urgent intervention, the mid-inferior apical septum had a linear VSD with irregular borders measuring 4x5 cm, which was closed with a Dacron patch (Figure 2). No other lesions were found except for the contusion of the apex of the heart. Subsequent progress was satisfactory.
Figure 1. Transthoracic echocardiographic image (with 4 Chambers) that reveals a wide irregular ventricular septal defect located in the mid-apical interventricular septum (arrow).
Figure. 2. Surgical image of the ventricular septal defect. It is linear with irregular borders and a diameter of approximately 4×5 cm.
Only 5% of closed thoracic traumas are complicated with a VSD. Asymptomatic myocardial contusion with an increase in cardiac enzymes is more common.1,2 Two mechanisms cause rupture of the IVS: the increase in intrathoracic pressure that compresses the heart and the myocardial contusion, with direct cellular damage or a change in coronary blood-flow and a secondary myocardial infarction.1,3 Both mechanisms complement each other in our patient, in whom ischaemia was seen at admission and the apical myocardial contusion was seen during surgery.
VSD following closed trauma usually affects the muscular septum,1,4,5 is located in the apex and is linear; occasionally there can be several.3,4 The diagnosis is usually delayed (between 12 h and 12 days)1,3,5 (in this case, it evolved in 2 phases: initially, from the myocardial contusion seen on the echocardiogram, and delayed, at 24 hours, due to septal necrosis and rupture)1,2,4; it is associated with a murmur at the left sternal border or over the apex, which may occur up to 6-10 days following trauma4; the electrocardiographic changes are usually nonspecific, and sinus tachycardia is more common.1 If coronary blood-flow is altered, it is not unusual to have elevation of the ST and T segments or the appearance of signs of infarction prior to their clinical manifestation,3,4 as in this case.
The diagnostic method of choice is echocardiogram. As in our patient, identification of contractile dysfunction indicates a high probability of complications secondary to trauma and is associated with increased mortality.6 The isolated TTE was diagnostic, but the images are suboptimal in 62% of cases, so transesophageal echocardiogram (TEE) is more specific.6 Even though post-traumatic rupture of the IVS is an unusual complication, it would be advisable to perform serial echocardiographic monitoring (with TTE or TEE), especially if there are signs of septal involvement such as those described above, regardless of the haemodynamic situation, for at least the first week following trauma.
Conservative treatment is recommended if the pulmonary/systemic flow ratio is <1.5-2 since spontaneous closure is possible.3,4 On the other hand, the haemodynamic situation will determine the urgency for intervention. Even in early intervention, surgical results and survival are notably higher than in traditional post-infarct VSD since the tissue damage is more local and there is a lower level of necrosis.