To the Editor,
Intramyocardial dissecting hematoma (IMDH) is a rare condition that can occur after cardiac trauma or, more frequently, following myocardial infarction, and is considered by some to be a form of subacute cardiac rupture. Spontaneous onset of IMDH in sporadic cases has also been reported. Intramyocardial dissecting hematoma tends to be more frequent in patients with acute myocardial infarction with ST segment elevation, and has been associated with reperfusion injury following infarction, mainly after thrombolysis or percutaneous revascularization.
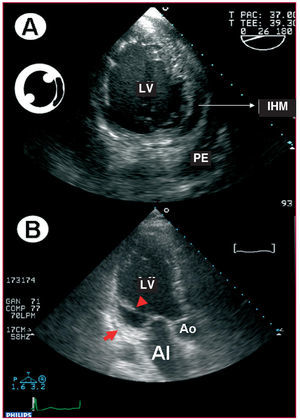
A 61-year-old man with a history of exertional angina and ex-smoker came to the hospital for chest pain with electrocardiographic changes, ST segment elevation in II, III, and aVF and depression in V2 through V4, and elevated cardiac enzymes (creatine kinase [CK], 1981 U/L; troponin-T, 1.66 ng/dL). In the emergency room, he again presented chest pain, coinciding with an episode of atrial fibrillation and accentuation of the electrocardiographic changes; emergency cardiac catheterization was performed. Coronary angiography showed mild left ventricular dysfunction due to moderate posterobasal hypokinesia and mitral regurgitation, proximal occlusion of the circumflex artery, with irregularities in the anterior descending and right coronary arteries, but no significant lesions. The patient underwent revascularization, aspiration, and intracoronary stent implantation with abciximab administration, as well as aspirin 100 mg/day, clopidogrel 75 mg/day, and intravenous enoxaparin 30 mg and 1 mg/kg/12 h thereafter. One day after surgery, he presented 2:1 atrial flutter with hypotension that was treated with electrical cardioversion. However, he remained hypotensive with no response to expansion and therefore, required positive inotropic drugs. The echocardiogram showed mild pericardial effusion with no signs of cardiac tamponade, ejection fraction of 45% with posterolateral hypokinesia, and moderate mitral regurgitation. Due to the patient's worsening condition, he was intubated and placed on mechanical ventilation, later undergoing transesophageal echocardiography that showed LV ejection fraction of 40%, with posterolateral hypokinesia, grade III/IV mitral regurgitation, mild pericardial effusion, and an intramyocardial hypoechoic area in the posterolateral wall consistent with an IMDH. Color Doppler ultrasound confirmed the absence of a defect with the pericardium or the endocardial cavity (Figure 1A). Follow-up echocardiography was performed at 3 weeks, revealing an aneurysm in the area corresponding to the IMDH, that caused distortion of the mitral subvalvular apparatus (Figure 1B) and severe mitral regurgitation.
Figure 1. A: transgastric short axis view at 26º showing involvement of the posterolateral wall of the left ventricle (LV) with an intraparietal echolucent image corresponding to intramyocardial hematoma (IHM) and pericardial effusion (PE). B: scar on the posterior aspect of the left ventricle (arrow) with tension on the subvalvular apparatus (arrowhead), leading to severe mitral insufficiency.
The hematoma initially contained in the myocardium tends to dissect it through the spiral fibers, leading to a neocavitation. The neocavitation is usually ovoid and produces an echolucent area inside the myocardial wall, delimited by the endocardial and epicardial layers. Echodense structures can be found in the interior and may be related to thrombi in different stages. The differential diagnosis of IMDH includes prominent ventricular trabeculations, intracavitary thrombi, and pseudoaneurysms. Careful examination of the endocardial and epicardial layers is extremely important, and contrast material is useful to delimit the endocardial borders and distinguish prominent ventricular trabeculations, thrombi, or pseudoaneurysms, whereas color Doppler ultrasound is able to detect the presence of a communication with the endocardial or pericardial cavities.1
One of the first series of IMDH described in the scientific literature compiles 15 cases, 8 of them diagnosed postmortem (cases prior to 1977), and the rest, 4 by echocardiography, 1 by ventriculography, and 2 in surgery. It is difficult to estimate the incidence of postinfarction IMDH, since most reports are isolated case studies, and many may go unnoticed if the spontaneous evolution is favorable.2
The treatment of IMDH is controversial, although surgical treatment is usually advisable. However, surgery is generally not performed until the condition results in complications (pseudoaneurysm, rupture, tamponade, etc), associated with higher mortality without surgery.3 In fact, good results with conservative treatment and follow-up with echocardiography, computed tomography, or magnetic resonance imaging have been described.4,5 Intramyocardial dissecting hematoma is a changeable entity that can progress to pseudoaneurysm or cardiac rupture,6 aneurysm formation, or complete resolution of the aneurysm. In autopsies of patients with cardiac rupture, IMDH is observed in 21% of cases. The presence of IMDH should be suspected when the ST segment remains high for more than 72 h after a myocardial infarction,1 with echocardiography useful for the diagnosis, follow-up, and therapeutic decision-making process.