Heart transplant is the treatment of choice for advanced heart failure. The number of ideal brain-dead donors, however, has decreased in recent decades, requiring the implementation of strategies to increase the number of transplantable hearts. These strategies include expanding donor acceptability criteria and using controlled donation after circulatory determination of death (cDCD), which currently accounts for 40% of organ donations in Spain.1
Promising results have been reported for different cDCD protocols implemented in Spain since 2020. No studies to date, however, have analyzed the potential for cDCD in Spain. To this end, we conducted a retrospective, observational study of all eligible cDCD donors (category-III donors according to the Maastricht classification adapted to Catalan policies) aged between 18 and 50 years who were registered with the Catalan Transplant Organization (OCATT) between January 1, 2013 (when cDCD was initiated in Catalonia) and February 28, 2021. We collected identifying information on donors and hospitals (whether or not they were located in the Barcelona Metropolitan Area [BMA]), demographic data, medical history pertinent to heart donation (hypertension; obesity; diabetes mellitus; dyslipidemia; drug use and type; smoking; and heart, lung, vascular, liver, and kidney disease), and heart retrieval data (use of normothermic regional perfusion, warm ischemia time [total and functional], and liver viability and reasons for nonviability).
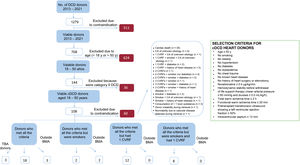
Suitability for cDCD was evaluated using the criteria applied at Hospital Universitario de Bellvitge in Barcelona, Spain (figure 1). To investigate the potential increase in donor availability, we examined 3 additional groups of potential donors: those with a single cardiovascular risk factor (CVRF) other than diabetes, smokers, and smokers with a single CVRF other than diabetes. We also made a note of where the donation took place (within or outside the BMA). Continuous variables are described as mean±SD deviation for normally distributed variables and median [interquartile range] for nonnormally distributed variables. Categorical variables are expressed as frequencies and percentages. Analyses were performed in SPSS version 25 (IBM Statistics).
Flowchart showing the selection of potential heart donors. BMA, Barcelona Metropolitan Area; CA, cardiorespiratory arrest; cDCD, controlled donation after circulatory determination of death; CVRF, cardiovascular risk factor; DCD, donation after circulatory determination of death;DM, diabetes mellitus; TBA, donors to be assessed by the transplant coordinator.
A total of 1279 potential DCD donors (categories IIa, IIb, and III) were registered with the OCATT between January 1, 2013 and February 28, 2021. Of these, 511 (39.95%) were excluded due to medical contraindications or family refusal to donate. Of the 768 potential donors remaining (60.05%), 624 (81.25%) did not meet the age criteria for heart donation. This left 144 (18.75%). Of these, 36 were category IIa or IIb donors and were therefore also excluded, leaving 108 potential cDCD donors (14.06%) aged 18 to 50 years. Eighteen fully met the criteria for donation. Another 3 had characteristics requiring further evaluation: 1 was a lung transplant recipient (previous sternotomy) and 2 were drug users. Two potential donors met all the criteria but were smokers, 12 had a single CVRF, and 8 had a single CVRF and were smokers (figure 1). Five donations (3 from donors who met all the criteria and 2 from donors who met criteria but were smokers) were made outside the BMA. The potential availability of cDCD heart donors was calculated for the different groups analyzed (table 1).
Potential for cDCD heart transplantation in Catalonia 2013 to 2021
| Potential in relation to total number of eligible cDCD donors (n=108)* | Potential in relation to total number of brain-dead transplants (n=435)* | |||||||
|---|---|---|---|---|---|---|---|---|
| BMA | Outside BMA | TBA | Total | BMA-MBA+TBA | BMA and outside BMA-BMA and outside BMA+TBA | BMA-MBA+TBA donors | BMA and outside BMA-BMA and outside BMA+TBA | |
| Full criteria | 18 | 3 | 3 | 24 | 16.66-19.44 | 19.44-22.22 | 4.13-4.82 | 4.82-5.51 |
| Full criteria+smoker | 2 | 2 | 3 | 7 | 1.85-4.62 | 3.70-6.48 | 0.45-1.14 | 0.92-1.61 |
| Full criteria+1 CVRF | 12 | 0 | 3 | 15 | 11.11-13.88 | 11.11-13.88 | 2.75-3.44 | 2.75-3.44 |
| Full criteria+smoker+CVRF | 8 | 0 | 3 | 11 | 7.4-10.18 | 7.4-10.18 | 1.84-2.52 | 1.83-2.53 |
| Total | 40 | 5 | 3 | 48 | 37.03-39.81 | 41.66-44.44 | 9.19-9.88 | 10.34-11.03 |
BMA, Barcelona Metropolitan Area; cDCD, controlled donation after circulatory determination of death; CVRF, cardiovascular risk factor; TBA, donors to be assessed.
cDCD is an emerging practice in several countries, including the United Kingdom, the United States of America, Australia, Belgium, and, more recently, Spain, where it is now available throughout the country. By the end of 2021, 15 transplants had been performed using hearts from cDCD donors in Spain. Survival data are not yet available, but reports from other countries have shown satisfactory outcomes (92% survival at 90 days).2
Based on strict application of the criteria at our hospital, 18 (16.6%) of the donors analyzed during the study period would have been eligible for cDCD. In this same period, 435 hearts from brain-dead donors were transplanted (57% in Catalonia). The 18 cDCD hearts represent a potential increase of 4.14%. Expanding the acceptability criteria would have increased the potential donor pool to 48 (44.4% of the 108 donors analyzed). This corresponds to a potential increase of 11% in heart transplants performed during the study period.
Studies on the potential of cDCD for heart transplants outside Spain have reported similar results to ours. Signalhal et al.3 analyzed 334 transplants performed over a 2-year period and reported a 4% increase in transplantable hearts per year of donation activity. Noterdaeme et al.4 reported an increase of 11% (70 donors over a period of 6 years), Osaki et al.5 an increase of 17% (70 donors in 2 years), and Messer et al.2 an increase of 8.6% (6429 donors in 5 years).
Our study demonstrates that cDCD could increase the potential number of hearts available for transplant. It also shows that the potential donor pool could be further increased by expanding the acceptability criteria to include smoking and/or certain CVRFs. CVRFs do not necessarily have to be a limiting factor in heart donation, as coronary angiography can be performed in advance. Accepting donors from outside the hospital could also increase the pool of transplantable hearts. In such cases, normothermic regional perfusion to reduce ischemia-reperfusion injury could be combined with cold preservation after retrieval or ex situ normothermic perfusion, although the procedure is costly. Another option for increasing the number of available hearts would be to progressively expand the age range for donation.
The main limitation of our study is its retrospective design. One or more of the 18 donors meeting all the criteria for cDCD might have eventually been excluded, and this possibility is even more likely in the group of expanded-criteria donors.
FundingNo funding.
Authors’ ContributionsN. Martínez-Franco: data collection and analysis; literature review; and drafting, revision, and approval of manuscript. E. Oliver-Juan and L. Anguela-Calvet: data analysis and revision and approval of manuscript. J. Tort and N. Manito-Lorite: data analysis and manuscript revision and approval. G. Moreno-González: study design, data analysis, literature review, and manuscript revision and approval.
Conflicts of InterestThe authors certify that they have no conflicts of interest to declare and have no affiliations with or involvement in any organization or entity with any financial interest such as honoraria and educational grants.
AcknowledgementsThis article was supported by a Research Assistance Award from Hospital Universitario de Bellvitge in 2017.