The PR interval is an important electrocardiogram (ECG) feature that reflects conduction through the atrioventricular (AV) node. Prolonged PR interval (or first-degree AV block) is a common—usually benign—ECG manifestation among athletes.1,2 Less information is available on short PR interval, with no data in pediatric athletes. Nevertheless, this is an important question because, when associated with ventricular pre-excitation or with symptoms, this otherwise benign condition could be a cause of of concern, and should not be overlooked in pre-participation screening (PPS) programs.3 We therefore aimed to determine the prevalence of PR alterations in pediatric athletes undergoing PPS.
The protocol conformed to the Declaration of Helsinki. We followed a single-center observational design. We studied athletes aged 5 to 16 years who attended a mandatory PPS launched by the Soccer Federation of Valencia (Spain) from August 2018 to June 2019. Twelve-lead ECG tracings were obtained following standard protocols using a portable PC-based ECG-12R electrocardiograph (Labtech Ltd, Debrecen, Hungary) and a specific software (Cardiospy v5.04.01, Labtech Ltd). First-degree AV block was defined as PR interval> 170ms (for children aged <12 years) or> 180ms (for those aged ≥ 12 years), and short PR as PR interval <90ms (< 12 years) or <95ms (≥ 12 years).4 We excluded rhythms other than sinus or respiratory sinus arrhythmia.
We studied 6307 children (mean±standard deviation age, 11±3 years; 100% Caucasian; 94% male; sports practice, 5.2±2.6h/wk.; regular sinus, 86.4% of total; sinus arrhythmia, 13.6%). The prevalence of first-degree AV block was 2.0% (95% confidence interval [95%CI], 1.6-2.3). No participant had a PR interval above the threshold criterion for pathological first-degree AV block in adult athletes (ie,> 400ms) and none had a PR interval> 300ms. In addition, no child with first-degree AV block had an associated pathological ECG change, and none had high-grade AV block. The prevalence of short PR was 0.6% (95%CI, 0.5-0.9). Nine participants were diagnosed with Wolff-Parkinson-White (WPW) syndrome, of whom 1 (2.5% of the subgroup) showed a short PR. Nevertheless, when we used adult criteria (ie, PR interval <120ms), 7 of the 9 children with WPW had a short PR (with PR interval=120ms in the other 2 children).
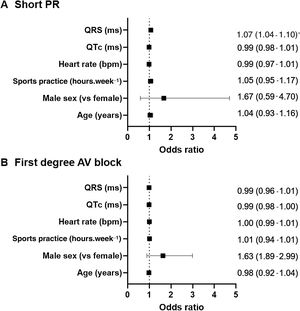
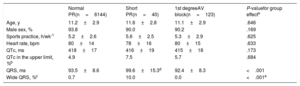
The main demographic and ECG characteristics of participants with abnormal PR duration did not essentially differ compared with those of their peers with normal ECG, except for QRS width (table 1). First-degree AV block was not associated with age, sex, hours of sports practice or other ECG characteristics (all P> .1), whereas children with a short PR were more likely to have a wider QRS (odds ratio, 1.07; 95%CI, 1.04-1.10; P <.001) (figure 1). These results remained unaltered after exclusion from the analyses of the 9 patients with WPW (data not shown).
Descriptive characteristics of study participants.
| Normal PR(n=6144) | Short PR(n=40) | 1st degreeAV block(n=123) | P-valuefor group effecta | |
|---|---|---|---|---|
| Age, y | 11.2±2.9 | 11.6±2.8 | 11.1±2.9 | .646 |
| Male sex, % | 93.8 | 90.0 | 90.2 | .169 |
| Sports practice, h/wk-1 | 5.2±2.6 | 5.6±2.5 | 5.3±2.9 | .625 |
| Heart rate, bpm | 80±14 | 78±16 | 80±15 | .633 |
| QTc, ms | 418±17 | 416±19 | 415±18 | .173 |
| QTc in the upper limit, %b | 4.9 | 7.5 | 5.7 | .684 |
| QRS, ms | 93.5±8.6 | 99.6±15.3d | 92.4±8.3 | <.001 |
| Wide QRS, %c | 0.7 | 10.0 | 0.0 | <.001e |
AV, atrioventricular.
Data are presented mean±standard deviation. See text for definition of short PR and first-degree AV block.
This is the largest cohort of pediatric athletes undergoing PPS to date. Our findings suggest a low prevalence of first-degree AV block among Caucasian pediatric athletes, which is similar to and below previous values reported for Caucasian (1.1%) and African athletes (11.4%), respectively, aged 8 to 18 years.2 An important finding of our study was the absence of pathological first-degree AV block when we used the cutoff for adults, 400ms. In addition, there is scarce data on short PR in athletes, with only Parry-Williams et al.5 reporting the prevalence of this condition (ie, 4.9%). Owing to the older age of the athletes studied by these authors (14-35 years) compared with our cohort, they used the adults’ threshold to define short PR (ie, PR interval <120ms1) whereas here we used the criteria for the pediatric population (< 90ms or <95ms for age <12 years and ≥ 12 years, respectively). This could explain, at least partly, the higher prevalence of short PR in the study by Parry-Williams et al.5—if we applied adult criteria to our cohort, the prevalence of short PR would indeed increase to 16.3%.
Short PR is considered a benign condition and no further evaluation is recommended unless it is associated with ventricular pre-excitation or symptoms. In this regard, the prevalence of WPW syndrome found was very low and in agreement with previous data (0.14%).6 Interestingly, when using pediatric criteria, as we did here, only 1 of the 9 children diagnosed with WPW syndrome had a short PR. This finding has not been reported previously, maybe because adult criteria for short PR (< 120ms) have usually been applied to pediatric cohorts, thereby potentially overestimating the true prevalence of this condition. Indeed, in our study, PR interval was ≤ 120ms in all the children with WPW. Therefore, in the presence of wide QRS complex and slurring of the QRS upslope, a diagnosis of WPW should not be discarded in children in the presence of a normal-for-age PR interval.
In summary, PR interval abnormalities are overall neither prevalent nor pathological among pediatric athletes. It must be noted, however, that some children with a normal PR interval attending to age-standardized thresholds might present with a serious condition that needs careful consideration, WPW syndrome.
FundingThe authors received no specific funding for this work. This work of PLV is supported by the University of Alcalá [contract number FPI2016].
AUTHORS’ CONTRIBUTIONSAll authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
CONFLICTS OF INTERESTNone.
We thank the team of nurses and physicians who helped to obtain and collect the clinical and electrocardiographic data.