Optimal lipid control is difficult to attain. We assessed preadmission achievement of the European Society of Cardiology targets for low-density lipoprotein-cholesterol (LDL-C) control in patients admitted for acute coronary syndrome.
MethodsFasting LDL-C levels were measured in 3164 patients admitted between 2010 and 2017. We assessed the frequency of adequate LDL-C control, with targets defined according to individual cardiovascular risk, and the predictors of inadequate control.
ResultsThe median LDL-C value was 104 (80-130) mg/dL. Most patients had high or very high cardiovascular risk and only 34.2% had LDL-C levels below the recommended target for their estimated risk. Achievement of LDL-C goals increased moderately throughout the study period. Adequate LDL-C control was inversely associated with patient risk. Dyslipidemia, active smoking, diabetes mellitus, and body mass index ≥ 25 were independent predictors of inadequate lipid control, while ongoing statin therapy was associated with adequate control.
ConclusionsOnly slightly more than one third of patients admitted for acute coronary syndrome meet recommended LDL-C targets on admission. There is broad scope for improvement in primary and secondary prevention, especially among patients who are overweight or have other cardiovascular risk factors.
Keywords
Dyslipidemia is common in patients with acute coronary syndrome (ACS).1–4 One of the cornerstones of cardiovascular disease prevention is a low-density lipoprotein-cholesterol (LDL-C) reduction due to its association with lower rates of cardiovascular events in both apparently healthy individuals and patients with other risk factors or those who have experienced an acute event.5–8 A meta-analysis of 26 clinical trials that evaluated the effect of statins on almost 170 000 patients concluded that each 1 mmol/L (38.67mg/dL) reduction in LDL-C is linked to a 22% lower 5-year incidence of major cardiovascular events,5 with a greater absolute benefit for patients with previous events. For this reason, the guidelines of the European Society of Cardiology (ESC), in agreement with the European Atherosclerosis Society and other scientific societies, recommend an LDL-C reduction in the population at risk, with more or less strict targets according to individual cardiovascular risk.9–11 However, despite the strength of the available evidence, in practice, the lipid control of patients is difficult and often inadequate.12–20
Little is known about the prior LDL-C control of patients admitted for ACS or about the factors associated with inadequate lipid control in this population. This information could help to identify the people most likely to benefit from interventions. Accordingly, we decided to analyze, in patients admitted for ACS to a tertiary hospital with a large referral population, the degree of prior adherence to the recommended LDL-C targets and the changes in adherence in recent years and to identify the variables associated with inadequate lipid control.
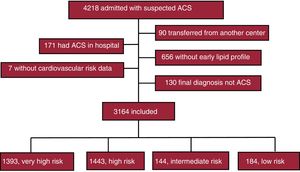
METHODSPatientsThe registry of patients admitted for suspected ACS to the coronary care unit of our center (a tertiary hospital with a referral population of more than 400 000 people) was reviewed between January 1st, 2010, and April 30st, 2017. This systematically and prospectively compiled registry collected their main demographic data, risk factors, comorbidities, previous treatments, clinical presentation, clinical course during admission, results of complementary examinations, including the fasting lipid profile obtained on the morning of the first working day after admission, and treatments during admission and at discharge, according to established recommendations.21 The exclusion criteria were patients transferred from another center, those who had ACS while they were hospitalized for another reason, those whose early lipid profile was unavailable because they were quickly transferred to another hospital or for any other cause, and those whose final diagnosis was not ACS. The study was approved by the clinical research ethics committee of our hospital.
Definition of preadmission lipid control targetsLDL-C concentrations were calculated using the Friedewald formula22 or were directly measured after ultracentrifugation in individuals with significant hypertriglyceridemia. Patients were deemed to have adequate lipid control at admission if their LDL-C concentrations were within the limits established by the applicable European guidelines on cardiovascular prevention10 or dyslipidemia management.11 According to these recommendations, the LDL-C target is <70mg/dL (or a ≥ 50% reduction if the baseline level is 70-135mg/dL) in patients with documented cardiovascular disease and in those in primary prevention considered at very high risk due to the presence of diabetes with target organ damage or of an associated major cardiovascular risk factor, severe chronic kidney disease (estimated glomerular filtration rate <30mL/min/1.73 m2), or an estimated 10-year risk of cardiovascular mortality ≥ 10%; the LDL-C target is <100mg/dL (or a ≥ 50% reduction if the baseline level is 100-200mg/dL) in patients considered at high risk due to the presence of a poorly controlled risk factor, diabetes mellitus without the above criteria, moderate chronic kidney disease (estimated glomerular filtration rate 30-59mL/min/1.73 m2), or an estimated 10-year risk of cardiovascular mortality of 5% to 10%. The target is <115mg/dL in the other patients with an indication for lipid-lowering therapy due to a moderate estimated risk. Finally, there is no defined target in the rest of the population, although an LDL-C ≥ 155mg/dL is considered inappropriate, unless the estimated risk is extremely low. Due to the limitations in the available information, only the absolute LDL-C targets were considered in the present study because the values prior to therapy initiation were not available for most patients undergoing lipid-lowering therapy and no attempt was made to retrospectively estimate the 10-year risk of cardiovascular mortality.
Statistical analysisCategorical variables are expressed as numbers and percentages and continuous variables as median [interquartile range]. Two categorical variables were compared using the chi-square test, whereas 2 continuous variables were compared using the Mann-Whitney U test. The presence of temporal trends in lipid target adherence was evaluated by comparing 4 consecutive time periods. Comparisons among these periods and among other ordinal variables, such as cardiovascular risk categories, were made using the chi-square test for linear trend for categorical variables and by the Jonckheere-Terpstra test for continuous variables. Variables independently associated with inadequate lipid control at admission were identified through multivariable logistic regression analysis with step-by-step elimination that included demographic variables, other cardiovascular risk factors, and the main comorbidities. Model calibration was assessed using the Hosmer-Lemeshow test and its discriminative capacity using the C statistic. A sensitivity analysis was performed by excluding patients who were admitted on Friday or Saturday and therefore lacked a lipid profile in the first 24hours of admission. However, these patients were kept in the study after verification that the results were practically unchanged. Through multivariable logistic regression analysis, the association between lipid control and hospital mortality was analyzed and the population attributable risk was calculated according to the methodology described.23 All analyses were performed with SPSS statistical software. P values <.05 were considered significant.
RESULTSDuring the study period, 4218 patients were admitted to our unit with suspected ACS; because 1054 patients were excluded for the reasons detailed in figure 1, the study population comprised 3164 patients.
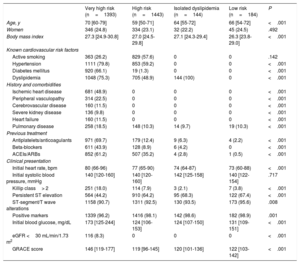
The median age of the patients was 65 [54-76] years, 76.1% were male, and 56.1% had persistent ST-segment elevation. The baseline cardiovascular risk, calculated as described above, was very high in 1393 patients (44.0%; in 901 [28.5%] due to known cardiovascular disease and in 492 [15.5%] due to other characteristics); in addition, 1443 (45.6%) had high risk, 144 (4.6%) had intermediate risk and an indication for lipid-lowering therapy, and 184 (5.8%) had none of these characteristics. The main characteristics of these 4 groups are summarized in table 1. Patients with higher risk were older than the others and, as expected, had a higher prevalence of cardiovascular risk factors and more frequently received drugs for cardiovascular prevention. Patients with higher baseline cardiovascular risk had a worse clinical presentation and less frequent persistent ST-segment elevation than the others.
Characteristics of the 4 groups of patients according to their baseline cardiovascular risk
| Very high risk (n=1393) | High risk (n=1443) | Isolated dyslipidemia (n=144) | Low risk (n=184) | P | |
|---|---|---|---|---|---|
| Age, y | 70 [60-79] | 59 [50-71] | 64 [55-72] | 66 [54-72] | <.001 |
| Women | 346 (24.8) | 334 (23.1) | 32 (22.2) | 45 (24.5) | .492 |
| Body mass index | 27.3 [24.9-30.8] | 27.0 [24.5-29.8] | 27.1 [24.3-29.4] | 26.3 [23.8-29.0] | <.001 |
| Known cardiovascular risk factors | |||||
| Active smoking | 363 (26.2) | 829 (57.6) | 0 | 0 | .142 |
| Hypertension | 1111 (79.8) | 853 (59.2) | 0 | 0 | <.001 |
| Diabetes mellitus | 920 (66.1) | 19 (1.3) | 0 | 0 | <.001 |
| Dyslipidemia | 1048 (75.3) | 705 (48.9) | 144 (100) | 0 | <.001 |
| History and comorbidities | |||||
| Ischemic heart disease | 681 (48.9) | 0 | 0 | 0 | <.001 |
| Peripheral vasculopathy | 314 (22.5) | 0 | 0 | 0 | <.001 |
| Cerebrovascular disease | 160 (11.5) | 0 | 0 | 0 | <.001 |
| Severe kidney disease | 136 (9.8) | 0 | 0 | 0 | <.001 |
| Heart failure | 160 (11.5) | 0 | 0 | 0 | <.001 |
| Pulmonary disease | 258 (18.5) | 148 (10.3) | 14 (9.7) | 19 (10.3) | <.001 |
| Previous treatment | |||||
| Antiplatelets/anticoagulants | 971 (69.7) | 179 (12.4) | 9 (6.3) | 4 (2.2) | <.001 |
| Beta-blockers | 611 (43.9) | 128 (8.9) | 6 (4.2) | 0 | <.001 |
| ACEIs/ARBs | 852 (61.2) | 507 (35.2) | 4 (2.8) | 1 (0.5) | <.001 |
| Clinical presentation | |||||
| Initial heart rate, bpm | 80 (66-96) | 77 (65-90) | 74 (64-87) | 73 (60-88) | <.001 |
| Initial systolic blood pressure, mmHg | 140 [120-160] | 140 [120-160] | 142 [125-158] | 140 [122-154] | .717 |
| Killip class> 2 | 251 (18.0) | 114 (7.9) | 3 (2.1) | 7 (3.8) | <.001 |
| Persistent ST elevation | 564 (44.2) | 910 (64.2) | 95 (68.3) | 122 (67.4) | <.001 |
| ST-segment/T wave alterations | 1158 (90.7) | 1311 (92.5) | 130 (93.5) | 173 (95.6) | .008 |
| Positive markers | 1339 (96.2) | 1416 (98.1) | 142 (98.6) | 182 (98.9) | .001 |
| Initial blood glucose, mg/dL | 173 [125-244] | 124 [106-153] | 124 [107-150] | 131 [109-151] | <.001 |
| eGFR <30 mL/min/1.73 m2 | 116 (8.3) | 0 | 0 | 0 | <.001 |
| GRACE score | 146 [119-177] | 119 [96-145] | 120 [101-136] | 122 [103-142] | <.001 |
ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers; eGFR, estimated glomerular filtration rate; GRACE, Global Registry of Acute Coronary Events.
Patients were considered to have a cardiovascular risk factor if this diagnosis was recorded in the electronic medical records or if they received treatment to manage a risk factor or reported having been diagnosed with the risk factor in question. Severe kidney disease is defined as creatinine values> 2.0mg/dL or history of dialysis or kidney transplant. Pulmonary disease is defined as a lung disease that requires chronic treatment or induces a functional limitation.
Data are expressed as No. (%) or median [interquartile range].
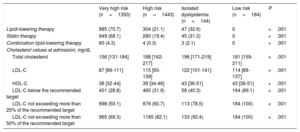
The median total cholesterol concentration was 174 [147-205] mg/dL: 104 [80-130] mg/dL for LDL-C and 39 [33-46] mg/dL for high-density lipoprotein-cholesterol (HDL-C). In total, 1083 patients (34.2%) had LDL-C values at admission within the guideline-recommended target range for their previous level of risk. In addition, 59.1% of patients did not exceed the recommended LDL-C target by more than 25% and 78.0% did not exceed it by more than 50%.
table 2 shows the cholesterol concentrations and those of their main fractions, the percentages of patients with ongoing lipid-lowering therapy, and the percentages of patients with adequate lipid control at the time of admission in the 4 risk groups. Almost a third of patients at very high risk and approximately 80% of those at high risk were not taking statins at the time of admission. In addition, although the LDL-C concentrations at admission were lower in patients with higher cardiovascular risk, the proportion of patients with optimal LDL-C levels also decreased as the cardiovascular risk increased. About 30% of the patients at very high risk and 20% of those at high risk had LDL-C values at admission that exceeded the recommended limits by more than 50%.
Baseline lipid-lowering therapy and cholesterol levels at admission in 4 groups of patients according to their baseline cardiovascular risk
| Very high risk (n=1393) | High risk (n=1443) | Isolated dyslipidemia (n=144) | Low risk (n=184) | P | |
|---|---|---|---|---|---|
| Lipid-lowering therapy | 985 (70.7) | 304 (21.1) | 47 (32.6) | 0 | <.001 |
| Statin therapy | 949 (68.1) | 280 (19.4) | 45 (31.3) | 0 | <.001 |
| Combination lipid-lowering therapy | 60 (4.3) | 4 (0.3) | 3 (2.1) | 0 | <.001 |
| Cholesterol values at admission, mg/dL | |||||
| Total cholesterol | 156 [131-184] | 188 [162-217] | 196 [171-219] | 181 [159-211] | <.001 |
| LDL-C | 87 [66-111] | 115 [93-139] | 122 [101-141] | 114 [89-137] | <.001 |
| HDL-C | 38 [32-44] | 39 [34-46] | 43 [36-51] | 43 [36-51] | <.001 |
| LDL-C below the recommended target | 401 (28.8) | 460 (31.9) | 58 (40.3) | 164 (89.1) | <.001 |
| LDL-C not exceeding more than 25% of the recommended target | 698 (50.1) | 876 (60.7) | 113 (78.5) | 184 (100) | <.001 |
| LDL-C not exceeding more than 50% of the recommended target | 965 (69.3) | 1185 (82.1) | 133 (92.4) | 184 (100) | <.001 |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein-cholesterol.
Data are expressed as No. (%) or median [interquartile range].
During hospitalization, 3097 patients (98.0%) received statins. Of the 3027 patients discharged alive, 96.0% were prescribed a lipid-lowering therapy, such as statins in 95.6% and combination therapy in 2.6%.
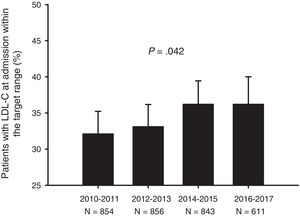
A significant, although small, tendency for better LDL-C control at the time of admission was observed over the study period. The percentage of patients with optimal control increased by about 4% between the beginning and end of this period (figure 2).
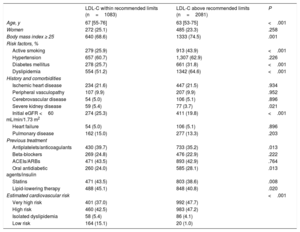
The baseline characteristics of the patients with adequate or inadequate LDL-C control according to guideline recommendations are shown in table 3. Patients with worse lipid control were younger and had a higher prevalence of overweight or obesity, active smoking, diabetes mellitus, and dyslipidemia and higher estimated cardiovascular risk, whereas renal failure and ongoing lipid-lowering therapy were associated with better LDL-C control. Of the patients taking statins, 37.5% had LDL-C levels within the target range.
Baseline characteristics of patients with LDL-C levels at admission within or above the recommended limits
| LDL-C within recommended limits (n=1083) | LDL-C above recommended limits (n=2081) | P | |
|---|---|---|---|
| Age, y | 67 [55-76] | 63 [53-75] | <.001 |
| Women | 272 (25.1) | 485 (23.3) | .258 |
| Body mass index ≥ 25 | 640 (68.6) | 1333 (74.5) | .001 |
| Risk factors, % | |||
| Active smoking | 279 (25.9) | 913 (43.9) | <.001 |
| Hypertension | 657 (60.7) | 1,307 (62.9) | .226 |
| Diabetes mellitus | 278 (25.7) | 661 (31.8) | <.001 |
| Dyslipidemia | 554 (51.2) | 1342 (64.6) | <.001 |
| History and comorbidities | |||
| Ischemic heart disease | 234 (21.6) | 447 (21.5) | .934 |
| Peripheral vasculopathy | 107 (9.9) | 207 (9.9) | .952 |
| Cerebrovascular disease | 54 (5.0) | 106 (5.1) | .896 |
| Severe kidney disease | 59 (5.4) | 77 (3.7) | .021 |
| Initial eGFR <60 mL/min/1.73 m2 | 274 (25.3) | 411 (19.8) | <.001 |
| Heart failure | 54 (5.0) | 106 (5.1) | .896 |
| Pulmonary disease | 162 (15.0) | 277 (13.3) | .203 |
| Previous treatment | |||
| Antiplatelets/anticoagulants | 430 (39.7) | 733 (35.2) | .013 |
| Beta-blockers | 269 (24.8) | 476 (22.9) | .222 |
| ACEIs/ARBs | 471 (43.5) | 893 (42.9) | .764 |
| Oral antidiabetic agents/insulin | 260 (24.0) | 585 (28.1) | .013 |
| Statins | 471 (43.5) | 803 (38.6) | .008 |
| Lipid-lowering therapy | 488 (45.1) | 848 (40.8) | .020 |
| Estimated cardiovascular risk | <.001 | ||
| Very high risk | 401 (37.0) | 992 (47.7) | |
| High risk | 460 (42.5) | 983 (47.2) | |
| Isolated dyslipidemia | 58 (5.4) | 86 (4.1) | |
| Low risk | 164 (15.1) | 20 (1.0) | |
ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers; eGFR, estimated glomerular filtration rate; LDL-C, low-density lipoprotein-cholesterol.
Patients were considered to have a cardiovascular risk factor if this diagnosis was recorded in the electronic medical records or if they received treatment to manage a risk factor or reported having been diagnosed with the risk factor in question. Severe kidney disease is defined as creatinine values> 2.0mg/dL or history of dialysis or kidney transplant. Pulmonary disease is defined as a lung disease that requires chronic treatment or induces a functional limitation.
Data are expressed as No. (%) or median [interquartile range].
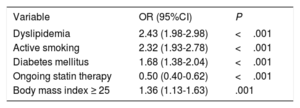
The results of the logistic regression analysis are shown in table 4. Dyslipidemia, active smoking, diabetes mellitus, and body mass index ≥ 25 were independent predictors of inadequate LDL-C control, whereas ongoing statin therapy was associated with adequate control. Model calibration was adequate (P=.303) and its discriminative capacity low (C=0.67). Independent predictors of very poor LDL-C control (> 50% above the target) were dyslipidemia, diabetes, smoking, lack of statin therapy, and younger age.
Independent predictors of inadequate LDL-C control
| Variable | OR (95%CI) | P |
|---|---|---|
| Dyslipidemia | 2.43 (1.98-2.98) | <.001 |
| Active smoking | 2.32 (1.93-2.78) | <.001 |
| Diabetes mellitus | 1.68 (1.38-2.04) | <.001 |
| Ongoing statin therapy | 0.50 (0.40-0.62) | <.001 |
| Body mass index ≥ 25 | 1.36 (1.13-1.63) | .001 |
95%CI, 95% confidence interval; LDL-C, low-density lipoprotein-cholesterol; OR, odds ratio.
Patients with LDL-C concentrations at admission within the target range had a worse presentation than the other patients (Killip class> 2, 15.6% vs 9.9%; P <.001; GRACE score, 139 [114-169] vs 126 [102-155]; P <.001) and higher hospital mortality (7.3% vs 2.8%; P <.001). After adjustment for other baseline predictors, adequate lipid control was not associated with mortality (odds ratio=1.41; 95% confidence interval [95%CI], 0.89-2.23; P=.139; population attributable risk, 16.8%; 95%CI, –7.1% to 31.8%).
DISCUSSIONIn the present study, 34.2% of patients admitted for ACS to the coronary care unit of a tertiary hospital between 2010 and 2017 had LDL-C values at admission within the target range for their level of risk. There was a slight increase in the percentage of patients with good lipid control during the study period. Patients’ LDL-C control was inversely associated with their cardiovascular risk. Dyslipidemia, smoking, diabetes mellitus, and body mass index ≥ 25 were all independent predictors of inadequate control, whereas ongoing statin therapy was associated with adequate control.
Lipid control in patients with stable ischemic heart diseaseMost studies evaluating the degree of lipid control have focused on stable patients. In recent surveys conducted in Europe or in other regions around the world, the percentage of patients with stable coronary heart disease and LDL-C concentrations <70mg/dL ranged between 7% and 30%.15,16,19,20 In studies restricted to patients being treated with statins, with or without documented cardiovascular disease, optimal control percentages ranged from 27% to 52%.13,14,17 In Spain, analysis of the Spanish cohort of one of these last studies obtained results that were in line with the general figures.24 In addition, also in Spain, LDL-C percentages within the target range were recently reported in 26% of 1103 patients with stable coronary heart disease25 and in 41.5% of 392 young people with familial hypercholesterolemia.18
Baseline lipid control in patients admitted for acute coronary syndromeAlthough inadequate lipid control has been associated with a higher incidence of ACS,5,6,8,26 dyslipidemia has often been considered as a dichotomous variable and few studies have analyzed the degree of baseline lipid control in patients admitted for ACS. In a large North American registry that included patients admitted for stable or unstable coronary disease between 2000 and 2006, 17.6% of the 136 905 patients whose LDL-C was measured (59% of the total) had levels <70mg/dL.12 Recently, the DYSIS-II registry27 included, in addition to patients with stable coronary disease, 3867 patients admitted for ACS in 2012 and 2013 in hospitals from 18 countries in Asia, Europe, and the Middle East; 18.9% had LDL-C concentrations at admission <70mg/dL. Finally, in a Greek study of 687 patients with ACS, patients with LDL-C concentrations in line with the recommended targets comprised less than 20% of the highest risk groups and between 30% and 40% of the lowest risk groups.28
This study provides contemporary information on the degree of LDL-C control in unselected patients admitted for ACS in Spain. No data had been available on this topic because Spanish hospitals were not involved in the DYSIS-II study. Compared with the studies mentioned, the proportion of patients with LDL-C levels within the recommended target range was higher in the present study, but still insufficient. Some data provide hope that the situation will improve. First, and in line with other registries,12,29,30 there was an increase, although small, in the proportion of patients with optimal lipid control in recent years. Second, the percentage of patients with extreme deviations from the target was relatively low. Finally, the lipid-lowering therapy was far from optimal in a considerable number of patients. As already observed,5,7,13,19,27 the percentage of patients with adequate LDL-C concentrations should be significantly increased by a more aggressive drug therapy based on the prescription of appropriate doses of potent statins to patients with high or very high risk, close analytical monitoring, and the use of combination therapies when monotherapy is insufficient. Lipid control can be improved with simple interventions,31,32 which must be maintained over time to avoid loss of treatment adherence among patients.33
Predictors of inadequate lipid controlThe degree of LDL-C control was inversely associated with the patients’ cardiovascular risk. This association, consistent with previous observations,14,17,28 is partly because the targets are more stringent for patients with higher risk, although it may also be more difficult for these patients to achieve strong and persistent LDL-C reductions due to worse adherence to treatments and healthy lifestyles or for other reasons. Specifically, poor LDL-C control was independently associated with dyslipidemia, smoking, diabetes, and excess weight, whereas statin therapy was associated with better control. These results also partly agree with previous observations,12–14,18,27 although diabetes has been associated with better lipid control in some studies.12,25,27 The results identify a subgroup of patients (with excess weight or these other risk factors) that warrant priority attention.
Methodological considerations and limitationsAlthough the patients were enrolled from a single center, their origin was diverse, not only because they belonged to the large catchment area of our hospital, but also because many patients admitted in line with the infarction code program came from remote regions. On the other hand, the series was large and includes almost as many patients with ACS as the largest multinational study published to date.27 Thus, the results are probably representative of the population of our country.
The lipid control targets were based on cardiovascular risk stratification of the patients according to the applicable European guidelines.10,11 Although, the treatment guidelines for dyslipidemia of 2011 were in force during most of the analyzed period,9 these recommendations were ambitious because they considered all patients with type 2 diabetes or moderate renal dysfunction as being at very high risk (with an LDL-C target <70mg/dL). Given that these targets were substantially reduced in subsequent guidelines and that there is a delay between recommendation publication and implementation, we believe that the current targets provide a more realistic and up-to-date view of patients’ lipid control.
As mentioned, we decided not to exclude patients admitted on Friday and Saturday—most of whom did not undergo an analysis within the first 24hours of admission—after verifying that their exclusion did not modify the results. This observation contrasts with some previous findings34 but is in line with those of the largest relevant study, which showed that LDL-C values do not vary significantly during ACS admission.35 In our study, low LDL-C values at admission were associated with worse clinical presentation and higher hospital mortality. This association may have influenced the results and indicates that, in the most severe patients, the LDL-C values at admission are probably not representative of the degree of prior control. Finally, a limitation in the available data prevented calculation of the 10-year cardiovascular risk and analysis of the association of the degree of lipid control with potential variables of interest, such as the patients’ psychological profile, therapeutic adherence, and statin potency or dose.
CONCLUSIONSMost patients admitted for ACS in Spain have high or very high cardiovascular risk and just over a third have LDL-C levels at admission within the recommended target range. Adequate LDL-C control is inversely related to patient risk. Dyslipidemia, smoking, diabetes, and excess weight are independent predictors of inadequate lipid control and identify a subgroup of patients with priority need for improved outpatient lipid control and general cardiovascular prevention.
FUNDINGJA Barrabés receives research funding from the Carlos III Health Institute (PI16/00232) and CIBERCV, cofinanced by the European Regional Development Fund (ERDF).
CONFLICTS OF INTERESTJA Barrabés has received fees from AstraZeneca and Menarini for educational activities and from Bayer for consulting. RM Lidón has received fees from Ferrer Laboratories for consulting. The remaining authors have not declared conflicts of interest.
- –
Dyslipidemia is common in patients with ACS. The LDL-C control of patients with stable ischemic heart disease is suboptimal, but there are few data on the degree of baseline lipid control of patients admitted for ACS and on the predictors of inadequate control in this population.
- –
Just over a third of patients admitted for ACS in Spain have LDL-C levels at admission within the recommended target range, a proportion that has tended to slightly improve in recent years. Excess weight and the coexistence of other risk factors are independent predictors of inadequate lipid control. Patients with these characteristics warrant priority attention to improve LDL-C control and decrease cardiovascular risk.