There is current controversy regarding the benefits of percutaneous recanalization (PCI) of chronic total coronary occlusions (CTO). Our aim was to determine acute and follow-up outcomes in our setting.
MethodsTwo-year prospective registry of consecutive patients undergoing PCI of CTO in 24 centers.
ResultsA total of 1000 PCIs of CTO were performed in 952 patients. Most were symptomatic (81.5%), with chronic ischemic heart disease (59.2%). Previous recanalization attempts had been made in 15%. The mean SYNTAX score was 19.5 ± 10.6 and J-score was > 2 in 17.3%. A retrograde procedure was performed in 92 patients (9.2%). The success rate was 74.9% and was higher in patients without previous attempts (82.2% vs 75.2%; P = .001), those with a J-score ≤ 2 (80.5% vs 69.5%; P = .002), and in intravascular ultrasound-guided PCI (89.9% vs 76.2%, P = .001), which was an independent predictor of success. In contrast, severe calcification, length > 20mm, and blunt proximal cap were independent predictors of failed recanalization. The rate of procedural complications was 7.1%, including perforation (3%), myocardial infarction (1.3%), and death (0.5%). At 1-year of follow-up, 88.2% of successfully revascularized patients showed clinical improvement (vs 34.8%, P < .001), which was associated with lower mortality. At 1-year of follow-up, the mortality rate was 1.5%.
ConclusionsCompared with other national registries, patients in the Iberian registry undergoing PCI of a CTO showed similar complexity, success rate, and complications. Successful recanalization was strongly associated with functional improvement, which was related to lower mortality.
Keywords
There is current controversy in the cardiologic community regarding the benefits of percutaneous coronary intervention (PCI) in chronic total coronary occlusions (CTO).1 This has led to some skepticism when ordering these procedures because they are usually complex, take a long time, use higher radiation doses, and have a lower success rate.2,3 Although up to 30% of patients treated by coronary angiography have at least 1 CTO, PCI is currently attempted on this lesion in only ∼4% of patients in our setting.4,5 This reluctance can be explained by 2 main reasons. On the one hand, early concerns about the prognostic benefit (understood as cardiovascular mortality) have not been resolved in more recent studies,6 despite ongoing improvements in parameters, such as the ventricular function, angina grade, and arrhythmic burden of patients in multiple registries.7–11 On the other hand, the success rate at hospitals highly experienced in these interventions is not consistent with that reported in the largest real-life registries,12–15 even with better overall outcomes due to technical improvements and due to the establishment of specific programs and specially trained staff.
The aims of the Iberian registry were first to determine the current success rate for attempts to unblock CTO in our setting by specially trained operators, based on a consecutive 2-year series and second, to learn the impact on prognosis and functional capacity of both success and failure of this intervention.
METHODSCase Definition and RegistryA prospective, consecutive registry of patients who had undergone CTO angioplasty was created through the Iberian registry. A total of 32 sites in Spain and Portugal participated in this registry. A 2-year recruitment period from January 2015 to December 2016 was selected, during which 24 of the participating sites included patients (). We defined CTO as angiographically proven anterograde flow obstruction of a coronary artery, known or suspected to have lasted > 3 months (with Thrombolysis In Myocardial Infarction [TIMI] flow = 0).1 The study included a total of 24 sites selected from around Spain with at least 1 operator experienced in CTO angioplasty who recorded all cases consecutively, independently, and without outside monitoring. An experienced operator was assumed to be any operator who had handled at least 50 chronic occlusions and who had been previously mentored in this intervention. Although this criterion represents a selection bias, the aim was to reflect current outcomes with this technique using a specific strategy. Once informed consent was obtained, data were obtained on clinical, anatomic (including specifically on occlusion), and procedure characteristics. Patients were considered to have a history of ischemic heart disease only if diagnosed before the procedure detecting the CTO to be treated. A total of 99% of the patients included were monitored during their hospital stay and at least once after discharge. A total of 37 procedures were excluded due to inclusion errors or duplicate data. The clinical assessment was performed by the attending clinical cardiologist according to Canadian Cardiovascular Society angina functional class (I to IV) and New York Heart Association dyspnea class (I to IV); clinical improvement was considered to be reduction of at least 1 grade on these scales. Additionally, quality of life was assessed by the EQ-5D Health Questionnaire and the Seattle Angina Questionnaire in a subpopulation. Each site entered the data using an online platform, complying with the requirements of the Law on Data Protection and accessible only to participating operators and registry coordinators. The registry is endorsed by the Cardiac Catheterization and Interventional Cardiology Section of the Spanish Society of Cardiology and was funded by an unconditional grant from Abbott Vascular Spain.
Statistical MethodsData are expressed as absolute and percent frequency in the case of qualitative variables. Quantitative variables are expressed as mean ± standard deviation or median [interquartile range], depending on variable distribution. Group comparisons were analyzed by the Student t test or its nonparametric equivalent, the Mann-Whitney U-test, for continuous variables, and the chi-square test or Fisher's exact test for categorical variables. Statistical significance was defined as P < .05. Variables with P < .10 in the univariate analysis were included in a multivariate logistic regression model to determine the predictors of recanalization success, the predictors of complications, and the predictors of functional improvement. Survival curves during total mortality follow-up were estimated by the log-rank test based on success or failure of CTO recanalization. Predictors of mortality were not analyzed, in order to avoid any overadjustments due to a low incidence.
All analyses were performed using SPSS Statistics, version 24.0.
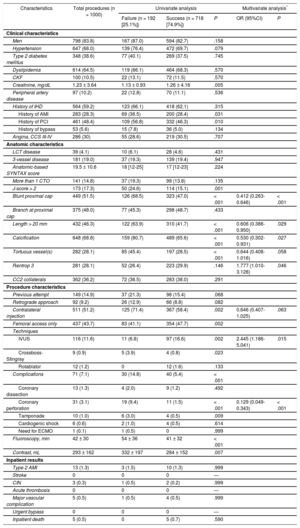
RESULTSBaseline CharacteristicsA total of 1000 CTO angioplasties were performed in 952 patients over a 2-year period; 83.8% were men, and the mean age was 65.5 ± 11.3 years. Most patients had symptoms (81.5%) and a history of ischemic heart disease (59.2%), with surgical revascularization in 5.6%, percutaneous revascularization in 48.4%, and previous attempts at unblocking in 15%. The mean anatomic-based SYNTAX score was 19.5 ± 10.6 (left common trunk disease in 4.1% and more than 1 chronic occlusion in 14.8%), and 17.3% had a J-score > 2. The main clinical and anatomic characteristics are summarized in Table 1.
Clinical, Anatomic, Procedure, and Inpatient Characteristics and Main Predictors of Angiographic Success
| Characteristics | Total procedures (n = 1000) | Univariate analysis | Multivariate analysis* | |||
|---|---|---|---|---|---|---|
| Failure (n = 192 [25.1%]) | Success (n = 718 [74.9%]) | P | OR (95%CI) | P | ||
| Clinical characteristics | ||||||
| Men | 798 (83.8) | 167 (87.0) | 594 (82.7) | .158 | ||
| Hypertension | 647 (68.0) | 139 (76.4) | 472 (69.7) | .079 | ||
| Type 2 diabetes mellitus | 348 (38.6) | 77 (40.1) | 269 (37.5) | .745 | ||
| Dyslipidemia | 614 (64.5) | 119 (66.1) | 464 (68.3) | .570 | ||
| CKF | 100 (10.5) | 22 (13.1) | 72 (11.5) | .570 | ||
| Creatinine, mg/dL | 1.23 ± 3.64 | 1.13 ± 0.93 | 1.26 ± 4.16 | .005 | ||
| Peripheral artery disease | 97 (10.2) | 22 (12.8) | 70 (11.1) | .536 | ||
| History of IHD | 564 (59.2) | 123 (66.1) | 418 (62.1) | .315 | ||
| History of AMI | 283 (28.3) | 69 (36.5) | 200 (28.4) | .031 | ||
| History of PCI | 461 (48.4) | 109 (56.8) | 332 (46.3) | .010 | ||
| History of bypass | 53 (5.6) | 15 (7.8) | 36 (5.0) | .134 | ||
| Angina, CCS III-IV | 286 (30) | 55 (28.6) | 219 (30.5) | .707 | ||
| Anatomic characteristics | ||||||
| LCT disease | 39 (4.1) | 10 (6.1) | 28 (4.6) | .431 | ||
| 3-vessel disease | 181 (19.0) | 37 (19.3) | 139 (19.4) | .947 | ||
| Anatomic-based SYNTAX score | 19.5 ± 10.6 | 18 [12-25] | 17 [12-23] | .224 | ||
| More than 1 CTO | 141 (14.8) | 37 (19.3) | 99 (13.8) | .135 | ||
| J-score > 2 | 173 (17.3) | 50 (24.6) | 114 (15.1) | .001 | ||
| Blunt proximal cap | 449 (51.5) | 126 (68.5) | 323 (47.0) | < .001 | 0.412 (0.263-0.646) | < .001 |
| Branch at proximal cap | 375 (48.0) | 77 (45.3) | 298 (48.7) | .433 | ||
| Length > 20 mm | 432 (46.3) | 122 (63.9) | 310 (41.7) | < .001 | 0.606 (0.386-0.950) | .029 |
| Calcification | 648 (68.8) | 159 (80.7) | 489 (65.6) | < .001 | 0.530 (0.302-0.931) | .027 |
| Tortuous vessel(s) | 282 (28.1) | 85 (45.4) | 197 (28.5) | < .001 | 0.644 (0.408-1.016) | .058 |
| Rentrop 3 | 281 (28.1) | 52 (26.4) | 223 (29.9) | .146 | 1.777 (1.010-3.128) | .046 |
| CC2 collaterals | 362 (36.2) | 72 (36.5) | 283 (38.0) | .291 | ||
| Procedure characteristics | ||||||
| Previous attempt | 149 (14.9) | 37 (21.3) | 98 (15.4) | .068 | ||
| Retrograde approach | 92 (9.2) | 26 (12.9) | 66 (8.8) | .082 | ||
| Contralateral injection | 511 (51.2) | 125 (71.4) | 367 (58.4) | .002 | 0.646 (0.407-1.025) | .063 |
| Femoral access only | 437 (43.7) | 83 (41.1) | 354 (47.7) | .002 | ||
| Techniques | ||||||
| IVUS | 116 (11.6) | 11 (6.8) | 97 (16.6) | .002 | 2.445 (1.186-5.041) | .015 |
| Crossboss-Stingray | 9 (0.9) | 5 (3.9) | 4 (0.8) | .023 | ||
| Rotablator | 12 (1.2) | 0 | 12 (1.6) | .133 | ||
| Complications | 71 (7.1) | 30 (14.8) | 40 (5.4) | < .001 | ||
| Coronary dissection | 13 (1.3) | 4 (2.0) | 9 (1.2) | .492 | ||
| Coronary perforation | 31 (3.1) | 19 (9.4) | 11 (1.5) | < .001 | 0.129 (0.049-0.343) | < .001 |
| Tamponade | 10 (1.0) | 6 (3.0) | 4 (0.5) | .009 | ||
| Cardiogenic shock | 6 (0.6) | 2 (1.0) | 4 (0.5) | .614 | ||
| Need for ECMO | 1 (0.1) | 1 (0.5) | 0 | .999 | ||
| Fluoroscopy, min | 42 ± 30 | 54 ± 36 | 41 ± 32 | < .001 | ||
| Contrast, mL | 293 ± 162 | 332 ± 197 | 284 ± 152 | .007 | ||
| Inpatient results | ||||||
| Type 2 AMI | 13 (1.3) | 3 (1.5) | 10 (1.3) | .999 | ||
| Stroke | 0 | 0 | 0 | — | ||
| CIN | 3 (0.3) | 1 (0.5) | 2 (0.2) | .999 | ||
| Acute thrombosis | 0 | 0 | 0 | — | ||
| Major vascular complication | 5 (0.5) | 1 (0.5) | 4 (0.5) | .999 | ||
| Urgent bypass | 0 | 0 | 0 | — | ||
| Inpatient death | 5 (0.5) | 0 | 5 (0.7) | .590 | ||
AMI, acute myocardial infarction; CC2, collateral connection grade 2; CCS, Canadian Cardiovascular Society; 95%CI, 95% confidence interval; CIN, contrast-induced nephropathy; CKF, chronic kidney failure; CTO, chronic total occlusion; ECMO, extracorporeal membrane oxygenator; IHD, ischemic heart disease; IVUS, intravascular ultrasound; LCT, left common trunk; OR, odds ratio; PCI, percutaneous coronary intervention.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
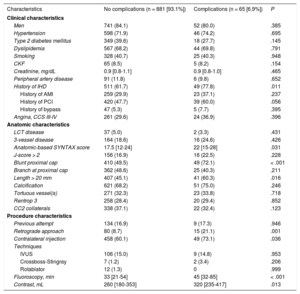
The characteristics of the procedure, as well as the predictive factors of successful recanalization and complications, are summarized in Table 1 and Table 2, respectively. The right coronary artery was most commonly affected (50.2%; 73.7% successful), followed by the anterior interventricular artery (34.3%; 83.5% successful) and circumflex artery (14.9%; 87.3% successful). The procedure was retrograde in 92 patients (9.2%) and considered as a first option in 75%.
Incidence and Predictors of Procedure-related Complications
| Characteristics | No complications (n = 881 [93.1%]) | Complications (n = 65 [6.9%]) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Men | 741 (84.1) | 52 (80.0) | .385 |
| Hypertension | 598 (71.9) | 46 (74.2) | .695 |
| Type 2 diabetes mellitus | 349 (39.6) | 18 (27.7) | .145 |
| Dyslipidemia | 567 (68.2) | 44 (69.8) | .791 |
| Smoking | 328 (40.7) | 25 (40.3) | .948 |
| CKF | 65 (8.5) | 5 (8.2) | .154 |
| Creatinine, mg/dL | 0.9 [0.8-1.1] | 0.9 [0.8-1.0] | .465 |
| Peripheral artery disease | 91 (11.8) | 6 (9.8) | .652 |
| History of IHD | 511 (61.7) | 49 (77.8) | .011 |
| History of AMI | 259 (29.9) | 23 (37.1) | .237 |
| History of PCI | 420 (47.7) | 39 (60.0) | .056 |
| History of bypass | 47 (5.3) | 5 (7.7) | .395 |
| Angina, CCS III-IV | 261 (29.6) | 24 (36.9) | .396 |
| Anatomic characteristics | |||
| LCT disease | 37 (5.0) | 2 (3.3) | .431 |
| 3-vessel disease | 164 (18.6) | 16 (24.6) | .426 |
| Anatomic-based SYNTAX score | 17.5 [12-24] | 22 [15-28] | .031 |
| J-score > 2 | 156 (16.9) | 16 (22.5) | .228 |
| Blunt proximal cap | 410 (49.5) | 49 (72.1) | < .001 |
| Branch at proximal cap | 362 (48.6) | 25 (40.3) | .211 |
| Length > 20 mm | 407 (45.1) | 41 (60.3) | .016 |
| Calcification | 621 (68.2) | 51 (75.0) | .246 |
| Tortuous vessel(s) | 271 (32.3) | 23 (33.8) | .718 |
| Rentrop 3 | 258 (28.4) | 20 (29.4) | .852 |
| CC2 collaterals | 338 (37.1) | 22 (32.4) | .123 |
| Procedure characteristics | |||
| Previous attempt | 134 (16.9) | 9 (17.3) | .946 |
| Retrograde approach | 80 (8.7) | 15 (21.1) | .001 |
| Contralateral injection | 458 (60.1) | 49 (73.1) | .036 |
| Techniques | |||
| IVUS | 106 (15.0) | 9 (14.8) | .953 |
| Crossboss-Stingray | 7 (1.2) | 2 (3.4) | .206 |
| Rotablator | 12 (1.3) | 0 | .999 |
| Fluoroscopy, min | 33 [21-54] | 45 [32-85] | < .001 |
| Contrast, mL | 260 [180-353] | 320 [235-417] | .013 |
AMI, acute myocardial infarction; CC2, collateral connection grade 2; CCS, Canadian Cardiovascular Society; CKF, chronic kidney failure; IHD, ischemic heart disease; IVUS, intravascular ultrasound; LCT, left common trunk; PCI, percutaneous coronary intervention.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
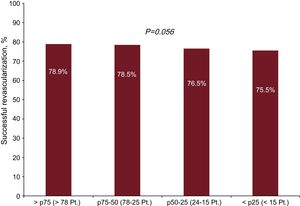
The overall success rate was 74.9%, higher in patients with no previous attempts (82.2% vs 75.2%; P = .001), in patients with J-score ≤ 2 (80.5% vs 69.5%; P = .002) and in procedures performed with intravascular ultrasound (IVUS) guidance (89.9% vs 76.2%; P < .001). In fact, the use of IVUS was the only modifiable factor that was an independent predictor of success (odds ratio [OR] = 2.445; 95% confidence interval [95%CI], 1.186-5.041; P < .015). Patients with worse kidney function and patients with complications during the procedure had lower success rates, and in particular, the presence of coronary perforations was associated with significantly fewer successful recanalizations (34.5% vs 79.9%; P < .001). The main factors described by the J-score, such as severe calcification, length > 20mm, and a blunt proximal cap, were also independent predictors of failed recanalization. Success varied from 68% to 91% among sites and was higher in the top quartile according to number of procedures (P = .056).
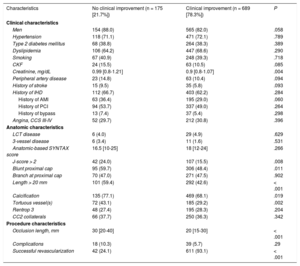
The procedure-related complication rate was 6.9%: coronary perforation (3%), cardiac tamponade (1%), myocardial infarction (1.3%), and death (0.5%). Complication-related factors are summarized in Table 2; independent predictors were a history of ischemic heart disease (OR = 2.230; 95%CI, 1.104-4.505; P = .025), blunt proximal cap (OR = 2.068; 95%CI, 1.088-3.934; P = .027), and retrograde access (OR = 3.527; 95%CI, 1.691-7.359; P < .001). The overall hospital mortality rate was 0.5%, and there were no significant differences according to PCI success or failure.
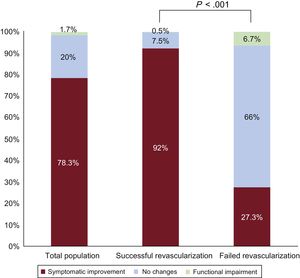
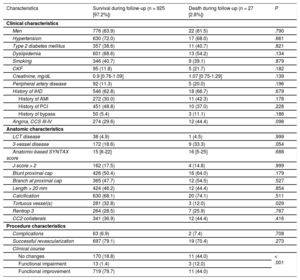
Clinical Results and Prognostic ImpactAfter a median follow-up of 365 [167-532] days, 78.3% of patients showed an improvement in New York Heart Association functional class for dyspnea or in Canadian Cardiovascular Society grade for angina. In 95% of patients with at least 2 years of follow-up who improved in the first year, the improvement persisted afterwards. In addition, a subpopulation of 183 patients showed significant improvement in the EQ-5D scale from 0.794 ± 0.115 to 0.869 ± 0.097 (P = .092) and in the Seattle Angina Questionnaire from 83.4 (75.4-90.0) to 95.1 (87.3-99.0) (P < .001). The main factors associated with functional improvement are shown in Table 3. Clinical improvement was significantly lower in the case of failed PCI (27.3% vs 92%; P < .001), as summarized in Figure 1. In addition to failed recanalization, the presence of other clinical conditions associated with functional impairment, such as a history of infarction or stroke and peripheral arterial disease, was associated with a lack of clinical improvement. Moreover, patients who experienced less clinical improvement had higher mortality (Table 4).
Main Predictors of Clinical Improvement During Follow-up After Percutaneous Coronary Procedure
| Characteristics | No clinical improvement (n = 175 [21.7%]) | Clinical improvement (n = 689 [78.3%]) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Men | 154 (88.0) | 565 (82.0) | .058 |
| Hypertension | 118 (71.1) | 471 (72.1) | .789 |
| Type 2 diabetes mellitus | 68 (38.8) | 264 (38.3) | .389 |
| Dyslipidemia | 106 (64.2) | 447 (68.6) | .290 |
| Smoking | 67 (40.9) | 248 (39.3) | .718 |
| CKF | 24 (15.5) | 63 (10.5) | .085 |
| Creatinine, mg/dL | 0.99 [0.8-1.21] | 0.9 [0.8-1.07] | .004 |
| Peripheral artery disease | 23 (14.8) | 63 (10.4) | .094 |
| History of stroke | 15 (9.5) | 35 (5.8) | .093 |
| History of IHD | 112 (66.7) | 403 (62.2) | .284 |
| History of AMI | 63 (36.4) | 195 (29.0) | .060 |
| History of PCI | 94 (53.7) | 337 (49.0) | .264 |
| History of bypass | 13 (7.4) | 37 (5.4) | .298 |
| Angina, CCS III-IV | 52 (29.7) | 212 (30.8) | .396 |
| Anatomic characteristics | |||
| LCT disease | 6 (4.0) | 29 (4.9) | .629 |
| 3-vessel disease | 6 (3.4) | 11 (1.6) | .531 |
| Anatomic-based SYNTAX score | 16.5 [10-25] | 18 [12-24] | .266 |
| J-score > 2 | 42 (24.0) | 107 (15.5) | .008 |
| Blunt proximal cap | 95 (59.7) | 306 (48.4) | .011 |
| Branch at proximal cap | 70 (47.0) | 271 (47.5) | .902 |
| Length > 20 mm | 101 (59.4) | 292 (42.6) | < .001 |
| Calcification | 135 (77.1) | 469 (68.1) | .019 |
| Tortuous vessel(s) | 72 (43.1) | 185 (29.2) | .002 |
| Rentrop 3 | 48 (27.4) | 195 (28.3) | .204 |
| CC2 collaterals | 66 (37.7) | 250 (36.3) | .342 |
| Procedure characteristics | |||
| Occlusion length, mm | 30 [20-40] | 20 [15-30] | < .001 |
| Complications | 18 (10.3) | 39 (5.7) | .29 |
| Successful revascularization | 42 (24.1) | 611 (93.1) | < .001 |
AMI, acute myocardial infarction; CC2, collateral connection grade 2; CCS, Canadian Cardiovascular Society; CKF, chronic kidney failure; IHD, ischemic heart disease; LCT, left common trunk; PCI, percutaneous coronary intervention.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Main Predictors of Cumulative Total Mortality After Percutaneous Coronary Procedure
| Characteristics | Survival during follow-up (n = 925 [97.2%]) | Death during follow-up (n = 27 [2.8%]) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Men | 776 (83.9) | 22 (81.5) | .790 |
| Hypertension | 630 (72.0) | 17 (68.0) | .661 |
| Type 2 diabetes mellitus | 357 (38.6) | 11 (40.7) | .821 |
| Dyslipidemia | 601 (68.6) | 13 (54.2) | .134 |
| Smoking | 346 (40.7) | 9 (39.1) | .879 |
| CKF | 95 (11.8) | 5 (21.7) | .182 |
| Creatinine, mg/dL | 0.9 [0.76-1.09] | 1.07 [0.75-1.29] | .139 |
| Peripheral artery disease | 92 (11.3) | 5 (20.0) | .196 |
| History of IHD | 546 (62.8) | 18 (66.7) | .679 |
| History of AMI | 272 (30.0) | 11 (42.3) | .178 |
| History of PCI | 451 (48.8) | 10 (37.0) | .228 |
| History of bypass | 50 (5.4) | 3 (11.1) | .186 |
| Angina, CCS III-IV | 274 (29.6) | 12 (44.4) | .098 |
| Anatomic characteristics | |||
| LCT disease | 38 (4.9) | 1 (4.5) | .999 |
| 3-vessel disease | 172 (18.6) | 9 (33.3) | .054 |
| Anatomic-based SYNTAX score | 15 [8-22] | 16 [5-25] | .688 |
| J-score > 2 | 162 (17.5) | 4 (14.8) | .999 |
| Blunt proximal cap | 426 (50.4) | 16 (64.0) | .179 |
| Branch at proximal cap | 365 (47.7) | 12 (54.5) | .527 |
| Length > 20 mm | 424 (46.2) | 12 (44.4) | .854 |
| Calcification | 630 (68.1) | 20 (74.1) | .511 |
| Tortuous vessel(s) | 281 (32.8) | 3 (12.0) | .029 |
| Rentrop 3 | 264 (28.5) | 7 (25.9) | .767 |
| CC2 collaterals | 341 (36.9) | 12 (44.4) | .416 |
| Procedure characteristics | |||
| Complications | 63 (6.9) | 2 (7.4) | .708 |
| Successful revascularization | 697 (79.1) | 19 (70.4) | .273 |
| Clinical course | |||
| No changes | 170 (18.8) | 11 (44.0) | < .001 |
| Functional impairment | 13 (1.4) | 3 (12.0) | |
| Functional improvement | 719 (79.7) | 11 (44.0) | |
AMI, acute myocardial infarction; CC2, collateral connection grade 2; CCS, Canadian Cardiovascular Society; CKF, chronic kidney failure; IHD, ischemic heart disease; LCT, left common trunk; PCI, percutaneous coronary intervention.
Data are expressed as No. (%) or median [interquartile range].
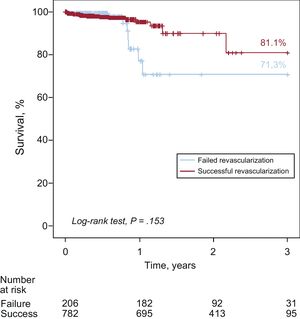
Of the 877 patients who completed 1-year follow-up (92.1% of total), 14 (1.5%) died, with no significant differences according to recanalization outcome. One-year mortality curves showed some divergence in favor of patients with successful recanalization. In patients with 3 years of follow-up, the mortality rate was higher in the case of failed recanalization (28.7% vs 18.9%), although the difference was not statistically significant (P = .153) (Figure 2). The main determinants of mortality during follow-up are summarized in Table 4.
DISCUSSIONThe Iberian registry on chronic occlusions is an initial contemporary effort to prospectively record the results of specific CTO recanalization programs recently implemented at many Spanish hospitals by operators trained in this technique. Following these criteria, a total of 952 patients from 24 sites were recruited, which accounts for 15.8% of all CTO treated during the same period at the 80 public sites with data published in the Spanish Cardiac Catheterization and Coronary Intervention Registries.4,5 The main findings were: a) evidence of similar success rates to those seen in other national and international registries and, consistent with them, the existence of a noticeable interhospital variability, with success rates of 68% to 91%, which are higher in the top quartile according to the number of procedures (Figure 3); b) although this registry does not have an arm with medical therapy only, it does show that patients referred for percutaneous recanalization who finally required medical therapy due to a failed procedure not only had worse functional status, but also had higher absolute mortality after the first year of follow-up, although this was not statistically significant, and c) although the validation of some traits of complexity (summarized in the J-score) was useful to predict failed recanalization, this registry identified modifiable factors that had an adverse impact on outcomes, such as low use of IVUS or low success rates by retrograde approach, which indicate reference points for future studies and targets where work can be done to improve these outcomes.
Patients with CTO were characterized by a high incidence of multiple cardiovascular risk factors and injury to other target organs, as well as multivessel disease, with a mean anatomic-based SYNTAX score of 19.5 ± 10.6, and complex lesions with J-score > 2 in 17.3% of patients. This is consistent with the data of the Canadian Multicenter CTO Registry7 and other similar registries7,16–19 indicating that isolated CTO are only present in 47% of patients. It is common for surgery to be ruled out in patients with single-vessel or multivessel disease but other comorbidities or poor distal bed visualization. In this situation, medical therapy was the first alternative for decades, but a significant percentage of patients still show evidence of ischemia or relevant symptoms8–11; in particular, up to 30% of patients included in the Iberian registry had Canadian Cardiovascular Society functional class III or IV angina. These data, along with the poor progress of patients with failed vs successful recanalization, appear to show that the indications of PCI for CTO are adequate in our setting.
Technical Aspects and Interhospital VariabilityImaging techniques such as IVUS or computed tomography are not commonly used in our setting (∼11%), even though they could provide diagnostic and therapeutic benefits to patients with limited angiographic visualization. Some studies report that IVUS is mainly used in more complex CTO and that it increases the success rate. This technique was used in more than 40% of patients in the Japanese Multicenter CTO Registry20 and the Multicenter Korean CTO Registry.21 However, the European Registry of Chronic Total Occlusion10,22 had lower rates (2.9% in all; 9.2% of retrograde) and indicate, like the Iberian registry, that it is not used as often by less expert operators. Habara et al.23 has already analyzed the impact of operator experience, showing that IVUS guidance to cross the guidewire has a clear learning curve affecting the need for support from expert operators for this technique to have a positive impact.24 This could also be said of the retrograde approach which, in our series, was a predictor of complications and is another modifiable factor that could increase the success rate. The use of 2 catheters (1 for contralateral injection) is not an independent predictor of success, which might indicate that this strategy is only used in the most complex cases and not in all situations in which it may be beneficial20,21; this could also explain why the rate of successful recanalizations is higher for PCI on the circumflex artery, even though previous series have always reported lower rates.20–23 In fact, less than 15% of attempts were performed on this artery, showing that a nonnegligible percentage of patients who might benefit from percutaneous recanalization by specific techniques are using medical therapy as the first and only option. On the other hand, the fact that eventually patients with failed attempts have more complications could indicate another potentially modifiable point that might increase the success rate and identify patients at risk of complications, making it possible to halt the procedure or to change how it is being done before complications occur.
Prognostic ImpactThis study was not intended to demonstrate impact on mortality, as this is a controversial aspect that requires well-designed studies with a control group, although such studies are often a matter of debate in the field of CTO.25 However, there was a low rate of complications, with no cases of urgent heart surgery and with a periprocedure mortality of only 0.5%. In addition, patients clearly experienced functional benefit, which was also associated with lower mortality during follow-up (P < .001) (Table 4), confirming that there are undeniable benefits to patients treated by CTO recanalization in cases with a clear indication. Although some studies, such as SYNTAX26 or the study by Banerjee et al.,18 have compared percutaneous recanalization in CTO vs surgery with slightly more favorable results in the percutaneous recanalization arm, these cohorts are not recent and also include patients with multivessel disease, without considering that the surgical outcomes were clearly worse when saphenous vs mammary grafts were used. This explains the minimal use of surgery in patients with single-vessel disease, particular in those with occlusion of the right coronary artery, which usually cannot be revascularized with mammary graft and is actually the artery most commonly affected by CTO.27–29 The Iberian registry indicates that, although not obvious during the first year after the intervention, mortality during longer term follow-up could be significantly reduced and also indicates that percutaneous recanalization of CTO in patients with no surgical indication (due to high risk or low SYNTAX score) is an alternative to consider in our setting, particularly in patients with symptoms and ischemia no longer alleviated by medical treatment.
LimitationsThe main limitations of this study is that, although it was performed prospectively and systematically, the data are informative and not monitored and there is no centralized angiographic analysis. In fact, the patients included are those selected by each hospital to undergo PCI, which could lead to heterogeneity between the clinical indications. This also explains why ischemia test data are not recorded, as the indication was defined at each hospital and there were no restrictions on indication in terms of inclusion criteria. Nevertheless, the study helps provide an accurate picture of clinical practice in our setting. Additionally, complications could be underestimated because the registry did not include a systematic record of electrocardiograms and sequential measurements of necrosis markers. It is true that a strict definition of infarction or perforation may increase the overall rate of complications when compared with other, less rigorous registries. Consequently, it should be taken into account that not all complications involve the same risk burden for the patient, as seen by the fact that no patients died during the procedure or required urgent recanalization surgery. Last, the data on clinical improvement were based on dyspnea status (New York Heart Association) and angina status (Canadian Cardiovascular Society), but there was no routine use of specific questionnaires or other objective examinations.
CONCLUSIONSThe Iberian registry is the first national registry on interventional cardiology in CTO and includes a large number of hospitals and patients. These patients had similar clinical and anatomic complexity to patients in other national registries, with comparable success and complication rates and with successful recanalization having a major impact on functional improvement.
FUNDINGThis study was funded by an unconditional grant from Abbott Vascular Spain.
CONFLICTS OF INTERESTJ.M. de la Torre Hernández received unconditional research grants from Boston and Abbott Vascular. J. Núñez Villota has given lectures sponsored by Abbott Vascular. All other authors declare no conflict of interests.
- –
There is controversy in the cardiologic community regarding the outcome of percutaneous recanalization procedures in CTO. Success rates at hospitals highly experienced in these surgeries are not consistent with those obtained in larger clinical practice registries. In fact, the current results of this intervention in our setting are unknown.
- –
The Iberian registry is the first contemporary interventional cardiology registry on CTO in our setting. The mean rate of successful recanalization was 74.9%, similar to that of other national registries. The use of IVUS was an independent predictor of success, whereas a high J-score and retrograde approach were independent predictors of failure. Successful recanalization had a major impact on functional improvement, which was associated with lower mortality during follow-up.