Functional mitral regurgitation (FMR) occurs in 20% to 30% of patients with heart failure (HF) and reduced left ventricular ejection fraction (LVEF).1,2 In these patients, FMR increases left ventricular (LV) end-diastolic pressure, contributes to LV remodeling, increases pulmonary hypertension, and worsens right ventricular function, all of which are associated with poor prognosis in HF. The clinical course of FMR depends on the type of heart disease, although the factors that determine its onset and the treatment of choice remain unknown. Treatment options include cardiac resynchronization and transplantation, but in most patients with this condition, it is not cured.3 Percutaneous mitral valve repair has comparable outcomes to surgery for organic mitral regurgitation with reasonable LVEF.4 Observational studies indicate that percutaneous treatment is beneficial in FMR with reduced LVEF. While randomized study results (ClinicalTrials.govNCT01772108) are awaited, it would be interesting to identify the patient profile that could benefit from this treatment.
We present the data on FMR from the Spanish HF Research Network (REDINSCOR). From 2007 to 2011, 2507 patients with symptomatic HF were recruited in 18 hospitals.5 We selected patients with LVEF < 40% with no organic valve disease or hypertrophic cardiomyopathy. Patients were then divided according to whether they had significant FMR (sFMR) (grade II-IV) or nonsignificant FMR (nsFMR) (grade 0-I). The analyses were performed using SPSS 22 and STATA-13.6
The study included 1526 patients: most were male (78%) with a history of hypertension (65%) and overweight (body mass index, 28.4). Fifty-seven percent were in functional class III or IV with elevated natriuretic peptide levels despite optimal HF therapy (86% were receiving beta-blockers, 87% were receiving angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists, and 64% were receiving aldosterone antagonists). The etiology of ventricular dysfunction was mostly ischemic (57%). At the time of study inclusion, 530 patients (35%) had signs of decompensated HF.
Significant FMR was detected in 746 patients (47%). The group with sFMR had a higher frequency of left bundle branch block, left atrial dilatation, and left ventricular dilatation, and worse LVEF. In addition, at the time of inclusion, they had a higher prevalence of decompensated HF, with associated increased natriuretic peptides, hypotension, and renal failure. The variables independently associated with the presence of sFMR were male sex (odds ratio [OR], 0.34; 95% confidence interval [95%CI], 0.25-0.47; P < .001), body mass index (OR, 0.94; 95%CI, 0.91-0.97; P < .001), decompensated HF (OR, 1.33; 95%CI, 1.01-1.74; P = .042), LV diameter (OR, 1.04; 95%CI, 1.02-1.05; P < .001), left atrial diameter (OR, 1.05; 95%CI, 1.03-1.07; P < .001), blood sodium level (OR, 0.97; 95%CI, 0.94-1.00; P = .044), and elevated natriuretic peptides (OR = 1.57; 95%CI, 1.17-2.1; P = .003) (area under the curve, 0.70; 95%CI, 0.67-0.74).
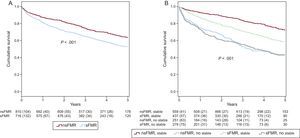
Median survival was 3.4 years [interquartile range, 1.7-4.7]. Survival at 1, 3, and 5 years was 84.5%, 69.9%, and 58.5%. Prognosis was worse (Figure A) in patients with sFMR (cumulative survival at 1 year, 81.5% vs 87.1%; at 3 years, 64.9% vs 74.3%, and at 5 years, 52.7% vs 63.5%; P < .001) due to mortality from refractory HF.
Kaplan-Meier curves. A: prognosis was worse in patients with sFMR (P < .001). B: patients with signs of decompensation (unstable) had lower survival independently of FMR severity. In stable patients, the presence of sFMR identified a group with intermediate prognosis (P < .001). FMR, functional mitral regurgitation; nsFMR, nonsignificant functional mitral regurgitation; sFMR, significant functional mitral regurgitation.
In the multivariable model, the variables that were independently associated with mortality were decompensated HF (hazard ratio [HR], 1.7; 95%CI, 1.32-2.13; P < .001), functional class III-IV (HR, 1.3; 95%CI, 1.01-1.67; P = .041), systolic blood pressure (HR, 0.99; 95%CI, 0.98-0.99; P = .01), LA size (HR, 1.02; 95%CI, 1.01-1.03; P = .001), anemia (HR, 1.34; 95%CI, 1.06-1.69; P = .013), glomerular filtration rate (HR, 0.99; 95%CI, 0.98-0.99; P < .001), elevated natriuretic peptides (HR, 1.88; 95%CI, 1.38-2.56; P < .001), blood sodium levels (HR, 0.97; 95%CI, 0.95-0.99; P = .038) and treatment with beta-blockers (HR, 0.51; 95%CI, 0.38-0.68; P < .001).
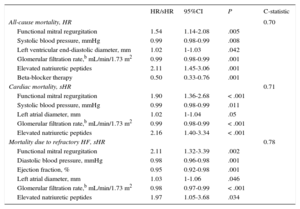
In stable patients without decompensated HF (n = 996), the presence of sFMR was independently associated with overall mortality, cardiac mortality, and mortality due to refractory HF (Table and Figure B). When FMR was included in the basic model, the integrated discrimination improvement index (added discrimination value due to increased sensitivity without compromising specificity) increased by 1.2% (P = .003) for all-cause mortality, 2% (P < .001) for cardiac mortality, and 2.5% (P < .001) for mortality due to refractory HF.
Cox and Fine-Gray Modelsa
| HR/sHR | 95%CI | P | C-statistic | |
|---|---|---|---|---|
| All-cause mortality, HR | 0.70 | |||
| Functional mitral regurgitation | 1.54 | 1.14-2.08 | .005 | |
| Systolic blood pressure, mmHg | 0.99 | 0.98-0.99 | .008 | |
| Left ventricular end-diastolic diameter, mm | 1.02 | 1-1.03 | .042 | |
| Glomerular filtration rate,b mL/min/1.73 m2 | 0.99 | 0.98-0.99 | .001 | |
| Elevated natriuretic peptides | 2.11 | 1.45-3.06 | .001 | |
| Beta-blocker therapy | 0.50 | 0.33-0.76 | .001 | |
| Cardiac mortality, sHR | 0.71 | |||
| Functional mitral regurgitation | 1.90 | 1.36-2.68 | < .001 | |
| Systolic blood pressure, mmHg | 0.99 | 0.98-0.99 | .011 | |
| Left atrial diameter, mm | 1.02 | 1-1.04 | .05 | |
| Glomerular filtration rate,b mL/min/1.73 m2 | 0.99 | 0.98-0.99 | < .001 | |
| Elevated natriuretic peptides | 2.16 | 1.40-3.34 | < .001 | |
| Mortality due to refractory HF, sHR | 0.78 | |||
| Functional mitral regurgitation | 2.11 | 1.32-3.39 | .002 | |
| Diastolic blood pressure, mmHg | 0.98 | 0.96-0.98 | .001 | |
| Ejection fraction, % | 0.95 | 0.92-0.98 | .001 | |
| Left atrial diameter, mm | 1.03 | 1-1.06 | .046 | |
| Glomerular filtration rate,b mL/min/1.73 m2 | 0.98 | 0.97-0.99 | < .001 | |
| Elevated natriuretic peptides | 1.97 | 1.05-3.68 | .034 |
95%CI, 95% confidence interval; HF, heart failure; HR, hazard ratio; sHR, sub-hazard ratio.
In patients with reduced LVEF, FMR is a marker of poor prognosis, but its role in decision-making is undefined. This could be partly because FMR severity varies depending on the patient's clinical condition, and partly because performing longitudinal studies that correctly evaluate the role of FMR in each phase of the disease can be difficult. The benefit of reducing FMR severity in advanced HF is uncertain. However, it is possible that in a certain group of patients, the hemodynamic improvement associated with FMR reduction may promote positive remodeling, as can happen with cardiac resynchronization therapy.3 Our study is the first to analyze the role of the patient's clinical condition in the course of FMR. Our results suggest that stable patients could potentially benefit from a reduction in FMR severity via percutaneous repair, and it would be interesting to study the effects of the procedure in this patient group. Randomized prospective studies are needed.
FUNDINGThis study was funded by the Red de Investigación Cardiovascular (Cardiovascular Research Network).