Predicting the incidence of and/or mortality associated with ischemic heart disease is of crucial importance in public health and consequently a number of scoring systems have been developed to estimate the risk of this disease, such as the Framingham equation1 or the SCORE chart.2 In 2011, the investigators in the INTERHEART study described a specific scoring system to predict the incidence of acute infarction, with a variant based on both low-density and high-density lipoprotein cholesterol.3 The objective of our study was to analyze the prognostic value of the INTERHEART-cholesterol score in patients admitted to hospital for chest pain.
This score is based on a prospective observational registry of all the patients hospitalized consecutively for chest pain in a single cardiology department over a 19-month period. In all, 1312 consecutive patients were recruited, of which 1240 (94.5%) were included in the study, after exclusion of those whose analytical results were not available. The enrolled patients were classified according to a diagnosis of acute coronary syndrome (ACS) or nonischemic chest pain. The INTERHEART-cholesterol score3 was calculated for each participant on the basis of age (> 55 years for men and > 65 years for women, 2 points), low-density lipoprotein cholesterol (77-116mg/dL, 1 point; 177-150mg/dL, 2 points; > 151mg/dL, 5 points), high-density lipoprotein cholesterol (< 40mg/dL, 2 points), tobacco use (ex-smoker, 2 points; smoker of 1-5 cigarettes/d, 2 points; smoker of 6-10 cigarettes/d, 4 points; smoker of 11-20 cigarettes/d, 7 points; smoker of > 20 cigarettes/d, 11 points), diabetes mellitus (7 points), and hypertension (6 points); the patients were divided into tertiles depending on their individual scores. After hospital discharge, the patients were followed up for at least 1 year.
The statistical analysis was carried out with SPSS 20.0 for Mac (SPSS Inc., Chicago, Illinois, United States). Categorical variables were evaluated with the chi-square test and continuous variables with Student's t test and analysis of variance (ANOVA). The survival analysis was performed using Cox proportional hazards regression by means of forward selection; for this analysis, we considered the lowest tertile as the reference variable and analyzed the variables not included in the INTERHEART score but having clinical implications for prognosis or those that obtained a P value ≤ .25 in the univariate analysis. P values < .05 were considered to indicate statistical significance.
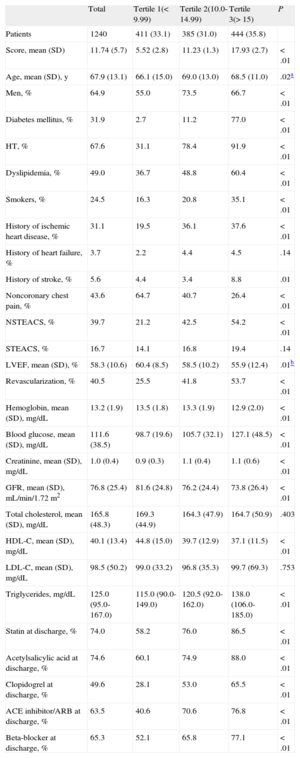
Of the 1240 patients studied, 467 (37.7%) had non-ST-segment elevation ACS, 189 (15.2%) had ST-segment elevation ACS, and 584 (47.1%) had nonischemic chest pain. The mean score (standard deviation) with the INTERHEART-cholesterol scale was lower in the group with nonischemic chest pain than in the ACS group: 10.02 (5.42) vs 13.27 (5.48) (P < .001). When the score results were analyzed by tertiles, the higher the tertile, the higher the cardiovascular risk and incidence of a history of cardiovascular disease, and the lower the prevalence of nonischemic chest pain (Table).
General Characteristics of the Study Population Divided Into Tertiles According to the INTERHEART-cholesterol Risk Score
| Total | Tertile 1(< 9.99) | Tertile 2(10.0-14.99) | Tertile 3(> 15) | P | |
| Patients | 1240 | 411 (33.1) | 385 (31.0) | 444 (35.8) | |
| Score, mean (SD) | 11.74 (5.7) | 5.52 (2.8) | 11.23 (1.3) | 17.93 (2.7) | <.01 |
| Age, mean (SD), y | 67.9 (13.1) | 66.1 (15.0) | 69.0 (13.0) | 68.5 (11.0) | .02a |
| Men, % | 64.9 | 55.0 | 73.5 | 66.7 | <.01 |
| Diabetes mellitus, % | 31.9 | 2.7 | 11.2 | 77.0 | <.01 |
| HT, % | 67.6 | 31.1 | 78.4 | 91.9 | <.01 |
| Dyslipidemia, % | 49.0 | 36.7 | 48.8 | 60.4 | <.01 |
| Smokers, % | 24.5 | 16.3 | 20.8 | 35.1 | <.01 |
| History of ischemic heart disease, % | 31.1 | 19.5 | 36.1 | 37.6 | <.01 |
| History of heart failure, % | 3.7 | 2.2 | 4.4 | 4.5 | .14 |
| History of stroke, % | 5.6 | 4.4 | 3.4 | 8.8 | .01 |
| Noncoronary chest pain, % | 43.6 | 64.7 | 40.7 | 26.4 | <.01 |
| NSTEACS, % | 39.7 | 21.2 | 42.5 | 54.2 | <.01 |
| STEACS, % | 16.7 | 14.1 | 16.8 | 19.4 | .14 |
| LVEF, mean (SD), % | 58.3 (10.6) | 60.4 (8.5) | 58.5 (10.2) | 55.9 (12.4) | .01b |
| Revascularization, % | 40.5 | 25.5 | 41.8 | 53.7 | <.01 |
| Hemoglobin, mean (SD), mg/dL | 13.2 (1.9) | 13.5 (1.8) | 13.3 (1.9) | 12.9 (2.0) | <.01 |
| Blood glucose, mean (SD), mg/dL | 111.6 (38.5) | 98.7 (19.6) | 105.7 (32.1) | 127.1 (48.5) | <.01 |
| Creatinine, mean (SD), mg/dL | 1.0 (0.4) | 0.9 (0.3) | 1.1 (0.4) | 1.1 (0.6) | <.01 |
| GFR, mean (SD), mL/min/1.72 m2 | 76.8 (25.4) | 81.6 (24.8) | 76.2 (24.4) | 73.8 (26.4) | <.01 |
| Total cholesterol, mean (SD), mg/dL | 165.8 (48.3) | 169.3 (44.9) | 164.3 (47.9) | 164.7 (50.9) | .403 |
| HDL-C, mean (SD), mg/dL | 40.1 (13.4) | 44.8 (15.0) | 39.7 (12.9) | 37.1 (11.5) | <.01 |
| LDL-C, mean (SD), mg/dL | 98.5 (50.2) | 99.0 (33.2) | 96.8 (35.3) | 99.7 (69.3) | .753 |
| Triglycerides, mg/dL | 125.0 (95.0-167.0) | 115.0 (90.0-149.0) | 120.5 (92.0-162.0) | 138.0 (106.0-185.0) | <.01 |
| Statin at discharge, % | 74.0 | 58.2 | 76.0 | 86.5 | <.01 |
| Acetylsalicylic acid at discharge, % | 74.6 | 60.1 | 74.9 | 88.0 | <.01 |
| Clopidogrel at discharge, % | 49.6 | 28.1 | 53.0 | 65.5 | <.01 |
| ACE inhibitor/ARB at discharge, % | 63.5 | 40.6 | 70.6 | 76.8 | <.01 |
| Beta-blocker at discharge, % | 65.3 | 52.1 | 65.8 | 77.1 | <.01 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CP, chest pain; GFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; HT, hypertension; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; NSTEACS, non–ST-segment elevation acute coronary syndrome; SD, standard deviation; STEACS, ST-segment elevation acute coronary syndrome.
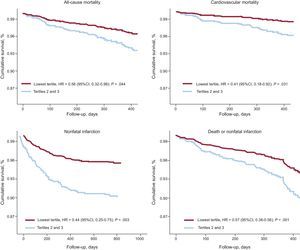
A 1-year follow-up was achieved in 96% of the patients (mean, 453.7 days [152.2 days]). Going from the lowest to the highest tertile, we observed a clear pattern of increasing rates of all-cause mortality (4.8%, 10.0%, and 13.4%; P < .01), cardiovascular mortality (2.6%, 7.1%, and 11.1%; P < .01), and nonfatal infarction (6.1%, 16.8%, and 22.5%; P < .01). Cox regression multivariate analysis demonstrated that the lowest tertile (< 10.0) was independently associated with a better prognosis for all the complications studied (Figure); age and a history of heart failure were associated with a higher incidence of these complications.
The INTERHEART-cholesterol score was designed to provide a highly specific tool for predicting the incidence of ACS, but its predictive power for ACS is low.3 This scoring system differs markedly from the Framingham score or the SCORE chart, which appears to make it useful in patients with chest pain. Its major advantage seems to lie in its ability to identify very low-risk patients, and our results provide evidence of its prognostic value after a hospital stay for chest pain.
The development of ACS is a multifactorial process that goes beyond the mere presence of cardiovascular risk factors.4 The identification of the determinants that lead to the destabilization of stable coronary lesions and cause ACS continues to be one of the great challenges in the knowledge of atherosclerosis. One of the major challenges in the knowledge of atherosclerosis continues to be the identification of the determinants that lead to the destabilization of stable coronary lesions and cause ACS. These determinants could be intrinsic characteristics of plaques5 or nonclassical factors.6
A limitation of this study is that the scoring system applied was designed for primary prevention in patients admitted to hospital for chest pain; however, this report is of interest because useful data such as those provided by the study are not available either in Spain or in Europe as a whole.
In short, the INTERHEART-cholesterol score identifies patients at low risk for complications following a hospital stay for chest pain. Therefore, it could be used to identify patients who, although they may not require mandatory follow-up, could nevertheless benefit from less exhaustive monitoring.