Keywords
INTRODUCTION
Many recent studies have shown that the resting heart rate (RHR) is an adverse prognostic factor in patients with high blood pressure,1 diabetes,2 and dyslipidemia.3 The same has been reported for patients who have had a heart attack,4 in those with heart failure,5 and even for the general population.6 In patients with stable coronary artery disease (sCAD), the available information on the event-prediction power of RHR stems from three large studies: an analysis of the CASS resgistry,7 which included patients suspected of having coronary disease referred for coronary angiography more than 30 years ago; a substudy of the INVEST clinical trial,8 which included hypertensive patients with sCAD randomized to receive either verampil or atenolol; and a subanalysis of the BEAUTIFUL clinical trial,9 which examined the prognostic impact of RHR on a sample of patients with sCAD and left ventricular dysfunction. Although these three studies showed the adverse prognostic value of the RHR in their own groups of patients, these selected populations may not behave in the same way as patients with sCAD treated in routine clinical practice—a point that the authors of these publications themselves raise.7-9 The aim of the present work was to assess the prognostic importance of the RHR in a general population of non-selected patients with sCAD treated as outpatients at a university hospital.
METHODS
From February 1, 2000 to January, 31 2004, all consecutive patients with sCAD who were monitored at 2 cardiology outpatient clinics offered weekly by a university hospital and led by 2 of the present authors, were included in this prospective study. This study was designed to determine the prognosis of sCAD in the present setting, and to identify any associated predictive factors. Patients were not excluded for any reason other than declining to participate.
Patients were referred to these clinics by their primary care physicians, the emergency room, or a cardiology or internal medicine ward. Patients were deemed to have sCAD when they met one or more of the following criteria: a history of acute coronary syndrome (ACS), ie, unstable angina; or acute myocardial infarction, or surgical or percutaneous coronary revascularization at least 3 months before inclusion; chest pain with exercise testing in the study; isotopic perfusion results or stress echocardiography results compatible with ischemia; and coronary angiography showing >70% stenosis of the lumen diameter of an epicardial vessel without serious valve disease.
Patient demographic and clinical information, physical examination data, and related testx results were collected at the first appointment. The heart rate was recorded from a resting electrocardiogram performed on the same day as the appointment or within the previous month. The baseline rhythm was recorded as sinus or as reflecting atrial fibrillation. The patients were managed according to their doctors' judgment, based on the Clinical Practice Guide of the Sociedad Española de Cardiología, the recommendations of the European Society of Cardiology, and those of the American College of Cardiology/American Heart Association for the management of stable angina.10-12 No formal analysis of adherence to these recommendations was undertaken.
The patients were followed up annually via outpatient appointments. Major events were recorded, including all-cause death, hospitalization for ACS (admission for angina-like chest pain with electrocardiographic or enzyme abnormalities), the need for revascularization (unforeseen in the initial assessment), stroke or transitory ischemic event (a neurological deficit of more or less than 24 h, respectively, diagnosed by a neurologist), or admission for heart failure (with a hospital stay of at least 24 h). Near the end of the study, medical histories, telephone interviews, and contacts with family doctors were used in an effort to minimize missing data and patients lost to follow up. Causes of death for patients who died in hospital was obtained from the analysis of medical records; for other cases of death information was obtained from family doctors and family members. No systematic consultation of death certificates was undertaken.
The study adhered to the Helsinki recommendations for medical studies. All patients provided written, informed consent to be included.
A retrospective analysis of this prospective patient cohort was performed to examine the association between RHR and the incidence of major events and mortality.
Statistical Analysis
Baseline and follow-up data were introduced into a database created using SPSS v.12.0 software (SPSS Inc., Chicago, Illinois, USA). The doctors responsible for each patient introduced the corresponding data. The Kolmogorov-Smirnov test was used to ensure that the quantitative data followed a normal distribution. Parametric quantitative data are presented as means (standard deviation); non-parametric data are presented as medians [interquartile range p25-p75]. Qualitative variables are expressed as percentages. Two subgroups were established: patients with an RHR equal to or above the median of the population, and patients with an RHR below the median. The sample was also divided into quartiles according to the RHR. Comparisons of quantitative parametric variables between subgroups were made using the Student t test or ANOVA; non-parametric quantitative variables were compared using the Mann-Whitney test or the Wilcoxon test as required. The c2 test was used to analyze differences between qualitative variables; the Fisher exact test was used when needed.
Three main endpoints were defined: major events (mortality, ACS, need for coronary revascularization, stroke, or admission for heart failure), coronary events (ACS or the need for coronary vascularization), and total mortality. Univariate associations of the baseline variables with these events were examined via Kaplan-Meier curves, using the log-rank test for comparisons between subgroups. Cox proportional hazard ratios were also calculated. Finally, multivariate Cox proportional hazard ratio models were constructed. The dependent variables were the major event rate, the coronary event rate, and total mortality; the independent variable was the RHR, evaluated as a dichotomous variable (equal to or greater than the median value, or lower than the median), by quartiles, and as a continuous variable.
The models initially involved all those variables that, in comparisons between the RHR subgroups, differed with a significance of P<.15 or had demonstrated prognostic significance in univariate analysis. Those variables that showed no significant association with the dependent variable in backward stepwise regression were eliminated. The final models therefore involved only the RHR and the variables that were demonstrated to be independent predictors. The results are presented as hazard ratios (HR) with 95% confidence intervals (95% CI). All statistical analyses were performed under the guidance of the Unidad de Apoyo a la Investigación (Research Support Unit) at our center. All calculations were made using SPSS software. Significance was set at P<.05.
RESULTS
Baseline Clinical and Demographic Characteristics
The study involved 1264 patients. The median age was 68 [60-74] years. Seventy-three percent of the patients were men. Nine percent of the patients were 50 years old or under, 31% were 51-65 years old, 54% were 66-80 years old, and 6% were over 80. At the first appointment, the median RHR was 70 [60-75] beats/min (bpm). The patients were divided into 2 groups: 645 (51%) with an RHR of ≥70 bpm and 619 (49%) with an RHR of <70 bpm. Table 1 shows the baseline characteristics of both groups and the different RHR quartiles. The mean age of the higher RHR group was significantly greater; this group also had a lower percentage of men and showed a higher frequency of diabetes mellitus. No significant differences were seen in terms of inclusion criteria between the 2 groups. In both groups more than 80% of patients had suffered a prior ACS, and more than 40% had undergone revascularization (the majority percutaneously). Surgical revascularization was more common in the higher RHR group, and percutaneous revascularization more common in the lower RHR group. Over 80% of the patients in both groups were asymptomatic. Blood pressure (systolic and diastolic) was higher in the higher RHR group. This group also showed a lower frequency of sinus rhythm, a higher rate of left ventricular dysfunction, and a significantly lower left ventricular ejection fraction. The use of medications of prognostic importance (statins, anti-platelet drugs, beta blockers) was lower among the higher RHR patients, except for the use of angiotensin converting enzyme inhibitors (ACEi), angiotensin II receptor antagonists (ARA-II) and diuretics, the use of which was greater in this group. The findings were similar by quartiles (Table 1).
Follow-up Data
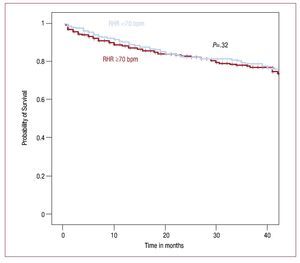
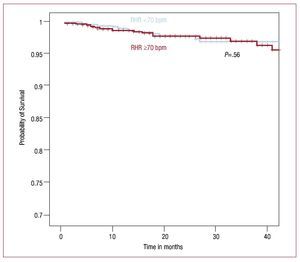
Follow-up data were available for 1257 patients (99.45%) patients (ie, there were just 7 losses), providing a total 2719 patient-years of follow-up. The median follow-up time was 25 [12-39] months. Some 222 patients (17.66%) suffered at least one major event: 116 (18.07%) in the higher RHR group, and 106 (17.24%) in the lower RHR group (P=.69). No significant differences were seen in the rate of any of the assessed events (Table 2). The probability of events, estimated via the use of Kaplan-Meier curves, was practically the same for both groups, at 17.48% for the higher RHR group and 17.67% for the lower RHR group at 25 months (P=.32) (Figure 1), and with the probability for total mortality 2.32% and 2.5% respectively (P=.56) (Figure 2). The univariate predictors of major events were diabetes mellitus, functional class >I, diastolic blood pressure, atrial fibrillation, and treatment with diuretics and nitrates; those of coronary events were functional class >1, diastolic and systolic blood pressure, and treatment with nitrates; and those of total mortality were age, diastolic blood pressure, atrial fibrillation, and treatment with beta blockers, diuretics or digoxin (Tables 3-5).
Figure 1. Probability of event-free survival according to resting heart rate (RHR) (Kaplan-Meier).
Figure 2. Probability of survival according to resting heart rate (RHR) (Kaplan-Meier).
The initial multivariate models were adjusted by age, sex, hypertension, diabetes mellitus, angina, and ischemia revealed in imaging tests as an inclusion criterion, percutaneous or surgical revascularization, functional class, blood pressure, baseline rhythm (sinus/atrial fibrillation), and treatment with statins, antiaggregants, beta-blockers, ACEi or ARA-11, diuretics, calcium antagonists, digoxin or nitrates. After refining the models (Table 6), no association was found between the RHR and the rate of major events, coronary events or total mortality in any analysis (ie, with the RHR as a continuous variable, a dichotomous variable, or by quartiles). All the variables included in multivariate analysis had a rate of missing data under 10%. The number of patients with complete data for all covariables (those valid for the initial multivariate models) was 1210 (96% of the sample). No ejection fraction data were available for 28% of the patients before the study began; this variable was, therefore, not included in the initial models. However, given its association with RHR and its recognized prognostic importance, additional analyses were performed in which it was included. Thus, the number of patients with all covariables complete and valid for use in this added multivariate analysis was 869 (69% of the sample). No association was seen between RHR and the rate of adverse events in these models either (Table 6).
DISCUSSION
As reported in earlier studies,7-9 significant differences were seen between the baseline characteristics of the patients according to their RHR. In general, those in the higher RHR group had a poorer risk profile, ie, a greater frequency of diabetes mellitus, older age, high blood pressure, and less use of statins, aspirin and beta blockers. However, no significant association was found between the RHR and the rate of major events or total mortality. No association was found even after adjusting for the variables showing significant differences at the initial appointment. This seems quite surprising given the overwhelming amount of evidence in favor of the RHR having a prognostic role in other populations1-6 and even in similar populations.7-9 This discrepancy might be explained in that the studies on sCAD published to date have involved highly selected populations that may not reflect the reality of everyday clinical practice. Table 7 shows that the patients of these earlier studies differed from those of the present work in several important ways. For example, the CASS study analysis7 included patients with suspected coronary heart disease referred for coronary angiography over a period that ended 30 years ago. In addition, the relatively young mean age of the patients (53 years), the low proportion of diabetics, and the scant use of medication with prognostic influence resulted in a population very different from that of the present work. Two more of these earlier studies based their conclusions on groups of patients recruited for clinical trials, with the possible bias that entails. For example, in the INVEST study,8 the proportion of women and hypertensive patients were in proportions higher than expected in a population with sCAD. In addition, the revascularization rate was relatively low, as was the use of medications with prognostic impact. Further more, in the BEAUTIFUL trial,9 although medical treatment was adequate, a population at especially high risk had been selected—patients with left ventricular systolic dysfunction. These differences had a clear impact on general prognosis, with total mortality reaching 6.31% after one year in the placebo group of the BEAUTIFUL trial, compared to 2.24% and 2.89% in the CASS registry and INVEST study, respectively, and 1.24% in the present work. Thus, in populations at lower risk, the prognostic impact of RHR is lower.
The INVEST8 study reports an incidence of arrhythmia of 6.6% in its population. This was significantly associated with a poorer prognosis, but the authors did not mention the type of arrhythmia involved. The BEAUTIFUL study9 only included patients with sinus rhythm, and the CASS registry7 recorded no information in this respect. In the present study, the frequency of atrial fibrillation at baseline was greater in the higher RHR patients, and was found to be a univariate predictor of major events and total mortality. However, after including this variable in initial multivariate analysis, it had no impact on the results.
The present study is a retrospective analysis of a cohort of prospectively enrolled and followed-up patients. Although the sample was not specifically designed to assess the prognostic value of the heart rate, this variable was recorded in a standardized fashion in all patients. The methodology is identical to that used in the CASS registry7 and INVEST study.8 Only the analysis of the placebo group in the BEAUTIFUL study9 involved an analysis of the prognostic value of RHR as a pre-specified objective.
The present work used a resting electrocardiogram to establish the RHR. Certainly, the heart rate shows wide variation over the course of a day and depends on many circumstances. It is therefore difficult to accept that a measurement taken at any particular time can adequately reflect such a complex variable. In fact, the adjustment of anti-angina medication, an objective of which is to obtain a relatively low RHR, is better based on a series of measurements than on a single measurement. However, all studies that have examined the value of the RHR in determining the prognosis of patients with sCAD have used single measurements, obtained either by physical examination7,8 or by electrocardiogram.9
Another possible explanation for the discrepancy in the prognostic value of RHR between the present and other studies might be an insufficient sample size. Table 7 shows that other studies involved between 5438 and 24 913 patients, many more than in the present work. No required sample size was calculated before the present study began: rather, as in other studies,7 we analyzed the information contained in the large database generated by our study and specifically. If the rates of major events and mortality seen in the present patients in the lower RHR group (17.24% and 2.44% in 2 years, respectively) are taken into account, for a 95% CI, a statistical power of 80% and a magnitude of expected effect expressed as a relative risk of 35%-40% for the higher RHR patients (in patients with an RHR ≥70 bpm the BEAUTIFUL study9 recorded a relative risk of 34% for cardiovascular death, 53% for admission for heart failure, 46% for myocardial infarction, and 38% for the need for coronary revascularization), between 1138 and 1456 patients would have been required to detect significant differences in major events, and 9770-12 450 would have been necessary to detect the same in total mortality (expected relative risks 40% and 35%, respectively). The present study included 1264 patients, a number that appears clearly insufficient for detecting significant differences in total mortality, and at the limit for establishing differences between RHR groups in terms of major events.
Finally, the present study is not the only one not to have found an association between the RHR and prognosis. In the Systolic Hypertension in Europe Trial,13 a relationship was only seen between these variables in elderly patients with high systolic blood pressure in the placebo group. No relationship was seen in the treatment group, which, however, returned a lower rate of events. Thus, it would seem that the prognostic impact of RHR is less when the risk of events is lower.
Limitations of the Study
Patient enrollment was undertaken just 2 cardiologists at our center, and patients were enrolled in weekly clinics, explaining the slow rate of recruitment. Given that both clinics cared for non-selected cardiological patients referred without restriction by primary care physicians, emergency room physicians, and hospital wards, the sample likely reflects very well the actual population of patients with sCAD cared for at our center. It need not, however, be representative of the populations cared for at other centers in Spain. Multicenter studies performed at national scale would be required to determine whether the present results are valid for these other populations. Secondly, the sample size or the rate of events may have been too small for significant differences to have been noticed. Note that in Table 6 the majority of hazard ratios are >1, reaching 2.29 for the quartile with the highest RHR with respect to total mortality. This might indicate a possible greater risk for patients with a high RHR, although with a wide confidence level. This could mean that the number of events registered was insufficient to provide adequate statistical power. However, the present findings could be clinically relevant since they indicate that the prognostic impact of RHR in populations at low risk is small.
Thirdly, no adjustment was made for the ejection fraction for the entire sample, since data were missing for 28% of the patients at the time of inclusion. This limitation is shared by other studies.7
Fourthly, no exhaustive analysis of the cause of death was undertaken. This, plus the reduced number of events, precluded a separate analysis of cardiovascular mortality.
Finally, the multivariate analysis did not take into account the changes that, over time, the prognostic variables (eg, medical treatment or the control of cardiovascular risk factors) may have experienced. As in similar studies, the present work only took into account the initial appointment results.
CONCLUSIONS
Despite its limitations, the present study found no significant association between the RHR and the prognosis of non selected patients with sCAD treated at a university hospital in Spain. The prognostic value of the RHR in routine clinical practice may be low in this population. However, it is possible that some effects may have failed to show a significant association because of a lack of statistical power. Studies with more patients and more events are required for more reliable conclusions to be drawn. However, while the results of larger studies are awaited (which should include non selected populations receiving appropriate treatment), the present findings suggest caution should be exercised against overestimating the prognostic impact of the RHR in patients with sCAD at low risk of a cardiac event.
ACKNOWLEDGMENTS
The authors thank Dr Elisa Muñoz Gomariz, of the Unidad de Apoyo a la Investigación at our center for her inestimable assistance in the statistical analysis of the data, and nurses Muñoz Álamo, Mercedes Ortiz Funes and M. Dolores Lara Lara for their essential, painstaking work in the cardiology clinics. Without their help this work would not have been possible.
ABBREVIATIONS
ACS: Acute coronary syndrome
RHR: resting heart rate
sCAD: stable coronary artery disease
This work was partially funded by a research grant from the Sociedad Andaluza de Cardiología.
Correspondence: Dr. M. Ruiz Ortiz.
San Adolfo, 18. 3o A. 14005 Cordoba. Spain
E-mail: maruor@gmail.com
Received November 27, 2009.
Accepted for publication May 19, 2010.