Invasive treatment in high-risk patients with non–ST-elevation acute coronary syndrome (NSTEACS) has been shown to improve their prognosis in terms of cardiovascular death and reinfarction.1 The prevalence of multivessel disease in these patients stands at about 50% and experts agree that performing complete revascularization is beneficial in such patients.1
Patients older than 75 years are underrepresented in studies and account for up to 35% of the total.1 Although these older patients benefit from invasive treatment,2 only a small percentage undergo percutaneous coronary intervention (PCI) and/or complete revascularization compared with younger patients.1,2
We have observed a growing interest in residual disease burden after PCI. The residual SYNergy between PCI with TAXus and cardiac surgery (SYNTAX) score (rSS), described by Généreux et al,3 is a strong prognostic factor of coronary events and all-cause death in patients who have undergone PCI.3
The aim of this study was to investigate the predictive value of rSS in a sample of octogenarian patients with NSTEACS and multivessel disease.
We performed a retrospective analysis of the data of 76 consecutive patients, aged 80 years or older, admitted with NSTEACS to a tertiary referral hospital between June 2013 and June 2014, and who received invasive treatment. All patients had multivessel disease. Patients received PCI at the decision of their cardiologist, at a site that generally performs culprit-vessel PCI in high-risk patients. The primary study variable was a composite of all-cause death and myocardial infarction (5-fold increase of baseline troponin) during admission and at 6 months. We calculated the GRACE score (Global Registry of Acute Coronary Events) for death and infarction during admission and at 6 months, the baseline SYNTAX score (bSS), rSS, and the Charlson comorbidity index. As in other studies,3 we grouped patients into terciles, according to their bSS and rSS (Table). Two interventional cardiologists analyzed untreated lesions and classified patients as “revascularizable” if they found any treatable lesions. We then performed a multivariable analysis with the GRACE and Charlson scores, bSS/rSS, left ventricular ejection fraction, age, creatinine, use of drug-eluting stents, and left main/3-vessel disease as variables, calculating logistic regression during admission and at follow-up.
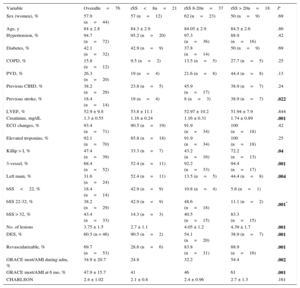
Baseline Characteristics and Variables During Admission by Residual SYNTAX Score
| Variable | Overalln=76 | rSS<8n=21 | rSS 8-20n=37 | rSS > 20n=18 | P |
|---|---|---|---|---|---|
| Sex (women), % | 57.9 (n=44) | 57 (n=12) | 62 (n=23) | 50 (n=9) | .69 |
| Age, y | 84 ± 2.8 | 84.3 ± 2.9 | 84.05 ± 2.9 | 84.5 ± 2.6 | .86 |
| Hypertension, % | 94.7 (n=72) | 95.2 (n=20) | 97.3 (n=36) | 88.9 (n=16) | .42 |
| Diabetes, % | 42.1 (n=32) | 42.9 (n=9) | 37.8 (n=14) | 50 (n=9) | .69 |
| COPD, % | 15.8 (n=12) | 9.5 (n=2) | 13.5 (n=5) | 27.7 (n=5) | .25 |
| PVD, % | 26.3 (n=20) | 19 (n=4) | 21.6 (n=8) | 44.4 (n=8) | .13 |
| Previous CIHD, % | 38.2 (n=29) | 23.8 (n=5) | 45.9 (n=17) | 38.9 (n=7) | .24 |
| Previous stroke, % | 18.4 (n=14) | 19 (n=4) | 8 (n=3) | 38.9 (n=7) | .022 |
| LVEF, % | 52.9 ± 9.8 | 53.8 ± 11.1 | 52.97 ± 10.2 | 51.94 ± 7.9 | .844 |
| Creatinine, mg/dL | 1.3 ± 0.55 | 1.16 ± 0.24 | 1.16 ± 0.31 | 1.74 ± 0.89 | .001 |
| ECG changes, % | 93.4 (n=71) | 90.5 (n=19) | 91.9 (n=34) | 100 (n=18) | .42 |
| Elevated troponins, % | 92.1 (n=70) | 85.8 (n=18) | 91.9 (n=34) | 100 (n=18) | .25 |
| Killip > I, % | 47.4 (n=39) | 33.3 (n=7) | 43.2 (n=16) | 72.2 (n=13) | .04 |
| 3-vessel, % | 68.4 (n=52) | 52.4 (n=11) | 92.2 (n=33) | 94.4 (n=17) | .001 |
| Left main, % | 31.6 (n=24) | 52.4 (n=11) | 13.5 (n=5) | 44.4 (n=8) | .004 |
| bSS<22, % | 18.4 (n=14) | 42.9 (n=9) | 10.8 (n=4) | 5.6 (n=1) | .001* |
| bSS 22-32, % | 38.2 (n=29) | 42.9 (n=9) | 48.6 (n=18) | 11.1 (n=2) | |
| bSS > 32, % | 43.4 (n=33) | 14.3 (n=3) | 40.5 (n=15) | 83.3 (n=15) | |
| No. of lesions | 3.75 ± 1.5 | 2.7 ± 1.1 | 4.05 ± 1.2 | 4.39 ± 1.7 | .001 |
| DES, % | 60.5 (n = 46) | 90.5 (n=2) | 54.1 (n=20) | 38.9 (n=7) | .001 |
| Revascularizable, % | 69.7 (n=53) | 28.6 (n=6) | 83.8 (n=31) | 88.9 (n=16) | .001 |
| GRACE mort/AMI during adm, % | 34.9 ± 20.7 | 24.8 | 32.2 | 54.4 | .002 |
| GRACE mort/AMI at 6 mo, % | 47.9 ± 15.7 | 41 | 46 | 61 | .001 |
| CHARLSON | 2.4 ± 1.02 | 2.1 ± 0.8 | 2.4 ± 0.96 | 2.7 ± 1.3 | .161 |
bSS, baselyne SYNTAX score; CIHD, chronic ischemic heart disease; COPD, chronic obstructive pulmonary disease; DEL, drug-eluting stent; ECG, electrocardiogram; GRACE mort/AMI during adm and at 6 mo, risk of mortality and acute myocardial infarction, by GRACE score during admission and at 6 months; LVEF; left ventricular ejection fraction; No. of lesions, number of coronary artery lesions per patient; PVD, peripheral vascular disease; rSS, residual SYNTAX score; 3-vessel, coronary disease involving 3 vessels.
Continuous quantitative variables are expressed as mean ± standard deviation.
The Table shows baseline characteristics and variables during admission, by rSS. Three-vessel disease was found in 68.4% of the patients, and left main coronary artery disease was found in 31.6%. With regard to baseline coronary disease, 38.2% and 43.4% of patients had a bSS score of 22-32 and>32, respectively. After PCI (with drug-eluting stents deployed in 6.5% of patients), 27.6% of patients achieved an rSS<8, while 48.7% and 23.7% still had an rSS of 8-20 and > 20, respectively. By rSS tercile, 28.6%, 83.8%, and 88.9% of patients had potentially revascularizable lesions after PCI.
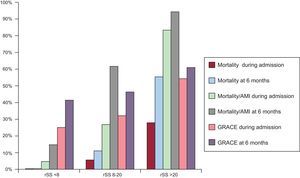
We found the composite variable was present in 34.2% of patients during admission (26 events: 4.7% with rSS<8, 27.1% with rSS 8-20, and 83.3% with rSS > 20; P<.001) and in 56.6% at 6 months (43 events: 14.3% with rSS<8, 62.1% with rSS 8-20, and 94.4% with rSS > 20; P<.001). All patients survived in the rSS<8 tercile. During admission, 7 patients died (2 with rSS 8-20 and 5 with rSS > 20; P=.006), and during follow up, 14 patients died (4 with rSS 8-20 and 10 with rSS > 20; P<.001). The Figure shows the primary variable and all-cause death by rSS. In the multivariable analysis of events during admission, the following variables were significant predictors: the GRACE score [odds ratio (OR)=1.07; 95% confidence interval (95%CI), 1.005-1.15; P=.036; area under the curve (AUC), 0.83: 95%CI, 0.72-0.94; P<.001], bSS (OR=1.13; 95%CI, 1.02-1.25; P=.023; AUC, 0.82; 95%CI, 0.70-0.94; P<.001), and rSS (OR=3.4; 95%CI, 1.005-12.39; P=.05; AUC, 0.86; 95%CI, 0.76-0.96; P<.001). At 6 months, the following variables reached statistical significance: the GRACE score (OR=1.45: 95%CI, 0.995-2.12; P=.05; AUC, 0.75; 95%CI, 0.62-0.86; P=.002), bSS (OR=1.33; 95%CI, 1.11-1.59; P=.002; AUC, 0.87; 95%CI, 0.78-0.97; P<.001), and rSS (OR=9.4; 95%CI, 1.61-55.1; P=.013; AUC, 0.86; 95%CI, 0.76-0.96; P<.001). The bSS and rSS were independent predictors when one or the other was removed from the analysis to avoid any colinearity between them.
Our study results confirm the relevance of the GRACE score and bSS as predictors of cardiovascular events in octogenarian patients with NSTE-ACS and multivessel disease and, for the first time, identify rSS as a predictive factor for these events.
Despite the existing tendency toward conservative treatment in octogenarian patients,2 our results suggest that more extensive revascularization might improve the prognosis of octogenarian patients with NSTE-ACS. In our opinion, advanced age and frailty should not be contraindications to performing the most complete revascularization possible. Since the need for dual antiplatelet therapy is already present in culprit-vessel PCI, complete revascularization should have a limited impact on the risk, and it should enhance the benefit. Although the differences in mortality may be explained by higher (but not statistically significant) comorbidity rates in the top tercile, we believe that the cardiovascular risk inherent in untreated lesions may play an important role.
The limitations of our study stem from its retrospective design and its short 6-month follow-up. Although we were unable to control all possible confounders and had a limited sample size, the differences are of sufficient significance to suggest that rSS has a prognostic value.
In conclusion, we believe our results show that rSS is a strong predictor of cardiovascular events in octogenarian patients with NSTEACS and that more extensive revascularization might improve the prognosis of these patients. However, randomized studies are needed to confirm this hypothesis.