Despite increased awareness of sex disparities in care and outcomes of acute myocardial infarction (AMI), there appears to have been no consistent attenuation of these differences over the last decade. We investigated differences by sex in management and 30-day mortality using the European Society of Cardiology Acute Cardiovascular Care Association quality indicators (QIs) for AMI.
MethodsProportions and standard errors of the 20 Acute Cardiovascular Care Association QIs were calculated for 771 patients with AMI who were admitted to the cardiology departments of 2 tertiary hospitals in Portugal between August 2013 and December 2014. The association between the composite QI and 30-day mortality was derived from logistic regression.
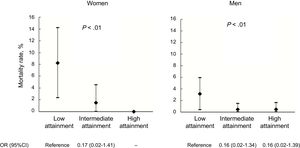
ResultsSignificantly fewer eligible women than men received timely reperfusion, were discharged on dual antiplatelet therapy and high-intensity statins, and were referred to cardiac rehabilitation. Women were less likely to receive recommended interventions (59.6% vs 65.2%; P < .001) and also had higher mean GRACE 2.0 risk score-adjusted 30-day mortality (3.0% vs 1.7%; P < .001). An inverse association between the composite QI and crude 30-day mortality was observed for both sexes (OR, 0.08; 95%CI, 0.01-0.64 for the highest performance tertile vs the lowest).
ConclusionsPerformance in AMI management is worse for women than men and is associated with higher 30-day mortality, which is also worse for women. Evidence-based QIs have the potential to improve health care delivery and patient prognosis in the overall AMI population and may also bridge the disparity gap between women and men.
Keywords
In recent decades, basic and clinical investigation has helped to elucidate the multifactorial and multidimensional differences between women and men with acute coronary syndrome (ACS).1 Emerging interest in coronary heart disease in women has revealed sex differences in pathophysiology and clinical presentation, preventive interventions and diagnostic strategies, and ACS management and therapeutic responses.2 Despite these differences, the literature supports equal benefit from evidence-based treatment of ACS for women and men and the need to promote and implement stringent guidelines for the management of ACS in women.3
Comparisons of sex differences in the quality of care for ACS pose challenges due to the multiple dimensions within the care process.4 Based on European Society of Cardiology (ESC) guidelines for the management of ACS, the ESC Acute Cardiovascular Care Association (ACCA) proposed a set of quality indicators (QIs) for the management of acute myocardial infarction (AMI).4 This set comprises 20 QIs across 7 domains and includes evaluation of the key aspects within the AMI care pathway. These indicators were recently validated using data from the National Health Service of England and Wales (Myocardial Ischaemia National Audit Project) and showed their potential to improve care and reduce unwarranted variation in death from AMI.5 The indicators may also be a useful tool to study sex inequalities in the process of care and outcomes of ACS in current settings. Through a prospective cohort study, we assessed differences by sex in quality of care and 30-day mortality using the ESC ACCA QIs for AMI.
METHODSStudy Design and Sample SelectionThe EPIHeart cohort study was designed with the a priori working hypothesis of inequalities in management and outcomes of patients with coronary heart disease in Portugal. This study included all patients consecutively admitted between August 2013 and December 2014 to the cardiology departments of 2 tertiary hospitals in 2 regions in northern Portugal (Hospital de São João, Porto, which covers part of the Porto metropolitan area on the coast, and Hospital de São Pedro, Vila Real, which covers the northeastern interior region). These 2 centers are high-volume units (ie, with more than 250 ACS hospitalizations annually). Eligible patients were 18 years or older, living in the catchment areas of these hospitals, not institutionalized before the event, expected to be hospitalized for at least 48hours, and diagnosed with type 1 (spontaneous) ACS. The diagnosis of ACS was not confirmed in 164 of the 1297 patients initially considered; a further 60 were discharged or transferred and 18 died before being invited to participate. Additionally, 44 patients were unable to answer the questionnaire due to clinical instability, inability to understand Portuguese, hearing problems, or cognitive impairment. Seventy-two patients refused to participate. Enrolled patients who were discharged alive, had valid contact details, and agreed to participate in the study were interviewed 6 months after hospital discharge (n = 890). For this analysis, only patients with a discharge diagnosis of ST-segment elevation myocardial infarction (STEMI) or non—ST-segment elevation myocardial infarction (NSTEMI) were included because the ESC ACCA QIs were proposed for only these types of ACS.4 In total, 771 patients were analyzed. The study protocol was in compliance with the principles of the Declaration of Helsinki and was approved by the Ethics Committees of both hospitals. All patients provided written informed consent.
Procedures, Data Collection, and Variable DefinitionsData were collected by trained researchers through structured patient interviews and via an extensive review of medical records, including discharge notes and clinical examinations and reports. Patients were also asked to complete the Mini-Mental State Examination6 and their self-care and mobility activities of daily living were assessed using the Modified Barthel Index.7 Vital status was obtained from the 6-month follow-up interview for patients who were hospitalized for less than 30 days and discharged alive.
Marital status was considered “partnered” for married patients or those in a civil union. Education/completed years of schooling was classified into 4 categories: a) less than 4 years (little formal education); b) 4 years (elementary school); c) less than 12 years (high school); and d) 12 or more years (secondary education or more).
Cognitive impairment was defined based on the Mini-Mental State Examination score,6 taking into account established cutoffs for individual education levels.8 Physical disability was determined by the Barthel Index; those who scored less than 90 on the Barthel Index were categorized as physically disabled.7,9
European Society of Cardiology Quality IndicatorsEach of the 20 QIs4 was calculated for eligible patients with complete procedure/treatment data and without contraindications. For the “reperfusion/invasive strategy” QI domain, patients were considered eligible using the following criteria: a) STEMI patients with a symptom onset to diagnosis (first medical contact) time less than 12 hours; and b) NSTEMI patients at intermediate or high risk (ie, those presenting at least 1 of the following criteria: diabetes mellitus, renal dysfunction defined as a Cockcroft-Gault estimated glomerular filtration rate < 30 mL/min/1.73 m2, left ventricular ejection fraction ≤ 0.40, heart failure, prior percutaneous coronary intervention [PCI], prior coronary artery bypass surgery, GRACE risk score > 140).4 Major contraindications related to coronary angiography were severe anemia (admission hemoglobin < 8 mg/dL) and/or severe renal failure (estimated glomerular filtration rate < 30 mL/min/1.73 m2 at admission).10,11
Variables for calculating the “reperfusion/invasive strategy” QI domain were directly derived from the collected data with the exception of the door-in door-out time for transferred STEMI patients, which was indirectly ascertained. We obtained exact admission times to non-PCI- and PCI-capable hospitals and were therefore able to estimate the transport time between the 2 hospitals via ambulance using ArcGIS (version 10.4.1) Network Analysis and an updated street network dataset provided by the Environmental Systems Research Institute. For each street segment, the street network dataset includes information on the traffic, average speed, and type of street (main, secondary, or highway), allowing accurate estimation of the shortest time-distance (minutes) between the point locations of the hospitals. Hospital locations were geocoded using Google Maps. We added 10minutes to the estimated time of transportation to account for time delays related to preparation of the patient and staff in the ambulance.
To calculate individual GRACE 2.0 risk scores,12 we used “diuretic usage” as a surrogate for Killip class II for 39 patients; 19 patients had no information on ST-segment deviation. For CRUSADE bleeding scores,13 the hematocrit was obtained by the following formula: admission hemoglobin × 2.94.14
For antithrombotics QIs, patients with a high risk of bleeding (CRUSADE score > 50),13 with previous hemorrhagic stroke, or discharged on oral anticoagulants were not considered eligible. Current data indicate that patients with MINOCA (Myocardial Infarction With Non-obstructive Coronary Artery Disease) should be discharged on simple antiplatelet therapy.15 We performed a sensitivity analysis and considered patients with MINOCA (absence of obstructive coronary heart disease ≥ 50% stenosis) as ineligible for QIs including dual antiplatelet therapy.
Systolic blood pressure lower than 100 mmHg or severe renal failure (estimated glomerular filtration rate < 30 mL/min/1.73 m2) at discharge were contraindications for angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Contraindications for beta-blockers were systolic blood pressure lower than 100 mmHg at discharge, asthma, and second- or third-degree atrioventricular block ().
To calculate the opportunity-based main composite QI, the numerator was the sum of the points of individual main indicators and the denominator was the sum of the points of applicable indicators, with all 12 indicators weighted equally (if fulfilled = 1).
Data AnalysisTo examine differences between women and men, the chi-square or Fisher exact test was used for categorical variables and the Student t test or Mann-Whitney test for continuous variables. For QIs, proportions and standard errors were calculated for eligible patients and those without missing procedure or treatment data.
The GRACE risk score-adjusted 30-day mortality was estimated based on predicted probabilities derived from logistic regression. The association between the composite QI and crude 30-day mortality was assessed using a logistic regression model; independent variables affecting the performance were categorized as low, intermediate, or high attainment according to the tertile distribution of the whole study sample.
All analyses were performed using STATA version 11.1 for Windows (Stata Corp LP, College Station, Texas, United States) and R version 2.12.1 (R Foundation for Statistical Computing, Vienna, Austria), with statistical significance determined at 5%.
RESULTSBaseline CharacteristicsCompared with men, women (n = 202, 26.2%) were older (68.6 vs 61.4 years; P < .001), less educated, more likely to be unpartnered and disabled, and had a lower income. They more frequently had hypertension and diabetes and were more often obese and never smokers. Women were also more likely to have prior atrial fibrillation and cancer. There were no significant differences by sex regarding history of ischemic heart disease, heart failure, renal failure, and stroke. Women more frequently had cognitive impairment and disability for activities of daily living (Table 1).
Baseline Demographic, Socioeconomic, and Medical History Characteristics of Women and Men With Acute Myocardial Infarction
| Women (n = 202) | Men (n = 569) | P | |
|---|---|---|---|
| Age, y | 68.6 ± 12.6 | 61.4 ± 12.7 | <.001 |
| Socioeconomic factors | |||
| Marital status | |||
| Partnered | 119 (59.2) | 467 (82.7) | <.001 |
| Education | |||
| Little formal education | 87 (43.5) | 58 (10.3) | |
| Elementary school | 64 (32.0) | 230 (40.9) | |
| High school | 26 (13.0) | 171 (30.4) | |
| Secondary education or more | 23 (11.5) | 104 (18.5) | <.001 |
| Employment status | |||
| Employed/homemaker | 60 (29.9) | 203 (35.9) | |
| Unemployed | 16 (8.0) | 85 (15.0) | |
| Retired | 82 (40.8) | 205 (36.3) | |
| Disabled | 43 (21.4) | 72 (12.7) | .001 |
| Household income, € | |||
| < 500 | 67 (33.2) | 106 (18.6) | |
| 501-1000 | 55 (27.2) | 187 (32.9) | |
| 1001-2000 | 19 (9.4) | 122 (21.4) | |
| > 2000 | 13 (6.4) | 67 (11.8) | |
| No response | 48 (23.8) | 87 (15.3) | .001 |
| Region | |||
| Porto | 98 (21.7) | 353 (78.3) | |
| Northeastern region of Portugal | 104 (32.5) | 216 (67.5) | .001 |
| Cardiovascular risk factors | |||
| Smoking | |||
| Never | 162 (80.2) | 155 (27.2) | |
| Current | 31 (15.4) | 236 (41.5) | |
| Former | 9 (4.5) | 178 (31.3) | <.001 |
| Hypertension | 163 (80.7) | 344 (60.5) | <.001 |
| Diabetes mellitus | 78 (38.6) | 159 (27.9) | .005 |
| Dyslipidemia | 124 (61.4) | 342 (60.2) | .769 |
| BMI, kg/m2 | 27.5 ± 5.0 | 26.9 ± 4.2 | .157 |
| Under- or normal weight | 72 (37.3) | 179 (33.7) | |
| Overweight | 71 (36.8) | 247 (46.5) | |
| Obese | 50 (25.9) | 105 (19.8) | .048 |
| Family history of CVD | 87 (46.3) | 205 (40.4) | .160 |
| Medical history | |||
| Myocardial infarction, PCI, and/or CABG | 31 (15.4) | 104 (18.4) | .332 |
| Heart failure | 16 (7.9) | 33 (5.8) | .297 |
| Renal failure | 11 (5.5) | 42 (7.4) | .350 |
| Atrial fibrillation | 18 (8.9) | 24 (4.2) | .012 |
| Stroke | 25 (12.4) | 48 (8.4) | .100 |
| Cancer | 22 (10.9) | 38 (6.7) | .055 |
| Cognitive impairment, MMSE score | 71 (37.2) | 91 (17.6) | <.001 |
| Disability, BI score | 41 (21.4) | 38 (7.2) | <.001 |
BI, Barthel index; BMI, body mass index; CABG, coronary artery bypass graft; CVD, cardiovascular diseases; MMSE, Mini-Mental State Examination; PCI, percutaneous coronary intervention.
Data are expressed as No. (%) or mean ± standard deviation.
Total may not add to 100% due to missing data.
Non—ST-segment elevation myocardial infarction was the final diagnosis in 412 patients (53.4%); 64% patients were initially admitted to a PCI-capable hospital and 24% were admitted through a fast-track system, without differences by sex (Table 2).
Clinical Presentation, Patient and System Delays, Risk Stratification, and Management of Women and Men With Acute Myocardial Infarction
| Women (n = 202) | Men (n = 569) | P | |
|---|---|---|---|
| NSTEMI (vs STEMI) | 113 (55.9) | 299 (52.6) | .406 |
| Admission to a PCI-capable hospital | 126 (62.4) | 367 (64.5) | .589 |
| Admission through fast-track system | 34 (20.6) | 120 (25.0) | .253 |
| Patient and system delays | |||
| STEMI, min | |||
| Symptom onset to FMC | 119 [60-300] | 81 [45-190] | .040 |
| FMC to arterial access | 197 [113-630] | 183 [95-415] | .411 |
| Symptom onset to arterial access | 460 [220-1096] | 308 [190-779] | .078 |
| PCI-capable hospital admission to arterial access | 96 [55-189] | 66 [34-203] | .028 |
| First hospital admission to arterial access | 124 [79-477] | 107 [52-336] | .133 |
| Door-in door-out time for transferred patients | 156 [96-378] | 134 [73-248] | .230 |
| Symptom onset to diagnosis | |||
| < 12 h | 77 (89.5) | 242 (92.0) | |
| 12-24 h | 6 (7.0) | 11 (4.2) | |
| < 24 h | 3 (3.5) | 10 (3.8) | .582 |
| NSTEMI | |||
| Symptom onset to FMC, min | 185 [60-395] | 120 [60-333] | .119 |
| Hospital admission to coronary angiography time, h | 32 [20-70] | 27 [17-55] | .049 |
| Admission variables/risk stratification | |||
| Heart rate, bpm | 81 ± 23 | 77 ± 18 | .003 |
| Systolic blood pressure, mmHg | 146 ± 63 | 141 ± 42 | .286 |
| Cardiac arrest at admission | 10 (5.0) | 22 (3.9) | .507 |
| ST-segment deviation at admission | 143 (72.6) | 410 (73.9) | .725 |
| Hemodynamic instability at admission* | 26 (12.9) | 24 (4.2) | <.001 |
| Baseline hematocrit at admission, % | 38.3 ± 4.7 | 42.8 ± 5.4 | <.001 |
| eGFR (CG) | 79.0 ± 37.4 | 95.8 ± 41.4 | <.001 |
| Calculated GRACE risk score | |||
| NSTEMI | 142 ± 3.8 | 132 ± 2.0 | .014 |
| STEMI | 168 ± 4.6 | 141 ± 2.0 | <.001 |
| Calculated CRUSADE risk score | |||
| NSTEMI | 41 ± 17 | 21 ± 16 | <.001 |
| STEMI | 36 ± 15 | 19 ± 13 | <.001 |
| Management approach | |||
| STEMI | |||
| Coronary angiography | 86 (96.6) | 269 (99.6) | .019 |
| Primary PCI | 52 (74.3) | 196 (86.3) | .017 |
| Thrombolysis | 10 (11.2) | 18 (6.7) | .163 |
| NSTEMI | |||
| Coronary angiography | 101 (89.4) | 286 (95.7) | .017 |
| Revascularization | 64 (56.6) | 220 (73.6) | <.001 |
| PCI | 54 (47.8) | 158 (52.8) | .036 |
| CABG | 11 (9.7) | 65 (21.7) | .005 |
| Moderate or severe left ventricular systolic dysfunction | 42 (20.9) | 94 (16.8) | .188 |
CABG, coronary artery bypass graft; eGFR (CG), estimated glomerular filtration rate (Cockcroft-Gault); FMC, first medical contact; NSTEMI, non—ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Total may not add to 100% due to missing data.
Patient and system delays16 were longer for women than men for both types of AMI (Table 2). Among STEMI patients, women had significantly higher median times for symptom onset to first medical contact and for PCI-capable hospital, admission to arterial access. The median time between hospital admission and coronary angiography was significantly longer in women with NSTEMI than in men (Table 2).
Compared with men, women were more often admitted with hemodynamic instability, had a lower mean estimated glomerular filtration rate, scored higher GRACE and CRUSADE scores, and were less likely to undergo invasive procedures, regardless of myocardial infarction type (Table 2).
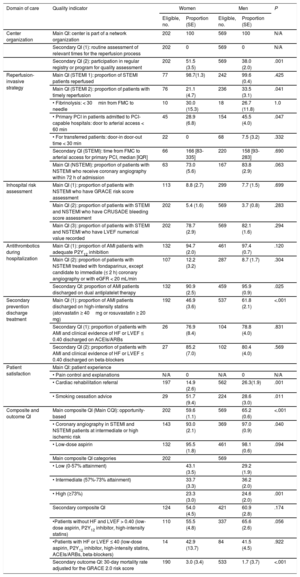
Quality IndicatorsDomain 1: Center OrganizationThe 2 centers do not routinely assess relevant times for the reperfusion process in STEMI patients and 1 center participates in a standard registry for quality assessment (Table 3).
Quality of Care According to the European Society of Cardiology Acute Cardiovascular Care Association Quality Indicators for Women and Men With AMI
| Domain of care | Quality indicator | Women | Men | P | ||
|---|---|---|---|---|---|---|
| Eligible, no. | Proportion (SE) | Eligible, no. | Proportion (SE) | |||
| Center organization | Main QI: center is part of a network organization | 202 | 100 | 569 | 100 | N/A |
| Secondary QI (1): routine assessment of relevant times for the reperfusion process | 202 | 0 | 569 | 0 | N/A | |
| Secondary QI (2): participation in regular registry or program for quality assessment | 202 | 51.5 (3.5) | 569 | 38.0 (2.0) | .001 | |
| Reperfusion-invasive strategy | Main QI (STEMI 1): proportion of STEMI patients reperfused | 77 | 98.7(1.3) | 242 | 99.6 (0.4) | .425 |
| Main QI (STEMI 2): proportion of patients with timely reperfusion | 76 | 21.1 (4.7) | 236 | 33.5 (3.1) | .041 | |
| • Fibrinolysis: < 30min from FMC to needle | 10 | 30.0 (15.3) | 18 | 26.7 (11.8) | 1.0 | |
| • Primary PCI in patients admitted to PCI-capable hospitals: door to arterial access < 60 min | 45 | 28.9 (6.8) | 154 | 45.5 (4.0) | .047 | |
| • For transferred patients: door-in door-out time < 30 min | 22 | 0 | 68 | 7.5 (3.2) | .332 | |
| Secondary QI (STEMI): time from FMC to arterial access for primary PCI, median [IQR] | 66 | 166 [83-335] | 220 | 158 [93-283] | .690 | |
| Main QI (NSTEMI): proportion of patients with NSTEMI who receive coronary angiography within 72 h of admission | 63 | 73.0 (5.6) | 167 | 83.8 (2.9) | .063 | |
| Inhospital risk assessment | Main QI (1): proportion of patients with NSTEMI who have GRACE risk score assessment | 113 | 8.8 (2.7) | 299 | 7.7 (1.5) | .699 |
| Main QI (2): proportion of patients with STEMI and NSTEMI who have CRUSADE bleeding score assessment | 202 | 5.4 (1.6) | 569 | 3.7 (0.8) | .283 | |
| Main QI (3): proportion of patients with STEMI and NSTEMI who have LVEF numerical value recorded | 202 | 78.7 (2.9) | 569 | 82.1 (1.6) | .294 | |
| Antithrombotics during hospitalization | Main QI (1): proportion of AMI patients with adequate P2Y12 inhibition | 132 | 94.7 (2.0) | 461 | 97.4 (0.7) | .120 |
| Main QI (2): proportion of patients with NSTEMI treated with fondaparinux, except candidate to immediate (≤ 2 h) coronary angiography or with eGFR < 20 mL/min | 107 | 12.2 (3.2) | 287 | 8.7 (1.7) | .304 | |
| Secondary QI: proportion of AMI patients discharged on dual antiplatelet therapy | 132 | 90.9 (2.5) | 459 | 95.9 (0.9) | .025 | |
| Secondary prevention discharge treatment | Main QI (1): proportion of AMI patients discharged on high-intensity statins (atorvastatin ≥ 40mg or rosuvastatin ≥ 20 mg) | 192 | 46.9 (3.6) | 537 | 61.8 (2.1) | <.001 |
| Secondary QI (1): proportion of patients with AMI and clinical evidence of HF or LVEF ≤ 0.40 discharged on ACEIs/ARBs | 26 | 76.9 (8.4) | 104 | 78.8 (4.0) | .831 | |
| Secondary QI (2): proportion of patients with AMI and clinical evidence of HF or LVEF ≤ 0.40 discharged on beta-blockers | 27 | 85.2 (7.0) | 102 | 80.4 (4.0) | .569 | |
| Patient satisfaction | Main QI: patient experience | |||||
| • Pain control and explanations | N/A | 0 | N/A | 0 | N/A | |
| • Cardiac rehabilitation referral | 197 | 14.9 (2.6) | 562 | 26.3(1.9) | .001 | |
| • Smoking cessation advice | 29 | 51.7 (9.4) | 224 | 28.6 (3.0) | .011 | |
| Composite and outcome QI | Main composite QI (Main CQI): opportunity-based | 202 | 59.6 (1.1) | 569 | 65.2 (0.6) | <.001 |
| • Coronary angiography in STEMI and NSTEMI patients at intermediate or high ischemic risk | 143 | 93.0 (2.1) | 369 | 97.0 (0.9) | .040 | |
| • Low-dose aspirin | 132 | 95.5 (1.8) | 461 | 98.1 (0.6) | .094 | |
| Main composite QI categories | 202 | 569 | ||||
| • Low (0-57% attainment) | 43.1 (3.5) | 29.2 (1.9) | ||||
| • Intermediate (57%-73% attainment) | 33.7 (3.3) | 36.2 (2.0) | ||||
| • High (≥73%) | 23.3 (3.0) | 24.6 (2.0) | .001 | |||
| Secondary composite QI | 124 | 54.0 (4.5) | 421 | 60.9 (2.8) | .174 | |
| •Patients without HF and LVEF > 0.40 (low-dose aspirin, P2Y12 inhibitor, high-intensity statins) | 110 | 55.5 (4.8) | 337 | 65.6 (2.6) | .056 | |
| •Patients with HF or LVEF ≤ 40 (low-dose aspirin, P2Y12 inhibitor, high-intensity statins, ACEIs/ARBs, beta-blockers) | 14 | 42.9 (13.7) | 84 | 41.5 (4.5) | .922 | |
| Secondary outcome QI: 30-day mortality rate adjusted for the GRACE 2.0 risk score | 190 | 3.0 (3.4) | 533 | 1.7 (3.7) | <.001 | |
ACEIs/ARBs, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers; AMI, acute myocardial infarction; eGFR, estimated glomerular filtration rate; FMC, first medical contact; HF, heart failure; LVEF, left ventricular ejection fraction; NSTEMI, non-ST-segment elevation acute myocardial infarction; PCI, percutaneous coronary intervention; QI, quality indicator; SE, standard error; STEMI, ST-segment elevation myocardial infarction.
Only 21.1% of women and 33.5% of men received timely reperfusion (P = .041). The median time from first medical contact to arterial access for primary PCI patients was similar in women and men. Among NSTEMI patients, eligible women received coronary angiography within 72hours of admission less often than men (73.0% vs 83.8%; P = .063) (Table 3).
Domain 3: Inhospital Risk AssessmentGRACE risk score was only assessed in 8% of NSTEMI patients and the CRUSADE bleeding score in 4.2% of all AMI patients, with no differences by sex. Left ventricular ejection fraction was recorded at similar rates in women and men (82.1% vs 78.7%; P = .294) (Table 3).
Domain 4: Antithrombotics During HospitalizationMore than 90% of patients received P2Y12 inhibitors, and a similar proportion was treated with fondaparinux or low-molecular-weight heparin (91.6% vs 94.4% for women and men, respectively; P = .359). Fondaparinux alone was prescribed to only about 10% of patients. There was a significant difference in the proportion of eligible women discharged on dual antiplatelet therapy vs men (90.9% vs 95.9%; P = .025). After the exclusion of patients with MINOCA (20 women [9.9%] and 26 men [4.6%]), this difference was still observed (89.7% vs 96.1% for women and men, respectively; P = .006) (Table 3).
Domain 5: Secondary Prevention Discharge TreatmentSignificantly fewer women than men were discharged on high-intensity statins (atorvastatin ≥ 40 mg or rosuvastatin ≥ 20 mg) (46.9% vs 61.8%; P < .001), but there was no difference between the sexes for prescriptions of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and beta-blockers at discharge (Table 3).
Domain 6: Patient SatisfactionIn contrast to referral for cardiac rehabilitation, eligible women received smoking cessation advice more often than men (14.9% vs 26.3%; P = .001; and 51.7% vs 28.6%; P = .011, respectively) (Table 3).
Domain 7: Composite Quality IndicatorsAbout 60% of women and 65% of men received the interventions for which they were eligible (P < .001). For the secondary composite QI, 54.0% of women and 60.9% of men with AMI received all secondary prevention drugs for which they were eligible (P = .174). Similar results were observed after the exclusion of patients with MINOCA (54.1% vs 60.8%; P = .212).
Outcome Quality IndicatorThere were 15 deaths within 30 days of admission, 8 in women and 7 in men. The mean GRACE 2.0 risk score-adjusted 30-day mortality was 3.0% in women and 1.7% in men (P < .001) (Table 3).
Quality Indicators and MortalityAn inverse association between the composite opportunity-based QI (by attainment tertiles) and crude 30-day mortality was observed for both women and men (Figure). Patients with higher attainment of recommended care were less likely to die vs patients in the “low” category of attainment of care (odds ratio [OR], 0.15; 95% confidence interval [95%CI], 0.03-0.66; and OR, 0.08; 95%CI, 0.01-0.64 for patients with intermediate and high attainment, respectively).
DISCUSSIONAs determined using the EPIHeart prospective cohort study, 6 of the 7 ESC ACCA QI domains for AMI showed worse performance for women than for men. Fewer women than men received timely reperfusion, were discharged on dual antiplatelet therapy and high-intensity statins, and were referred for cardiac rehabilitation. They also scored lower in the main composite QI for advisable interventions. An inverse association between the attainment of composite QI and mortality was observed for both sexes. Without differences by sex, we found low levels of ischemic and bleeding risk stratification assessment using the GRACE and CRUSADE prognostic tools and use of fondaparinux in eligible NSTEMI patients.
The ACS care pathway is complex and difficult to evaluate. Patient and system factors have competing effects on patient flow through the health care system. These factors often influence each other and act at different times during an episode of illness and care.17 Disparities in health care and outcomes between women and men are multifactorial and occur at different levels of the ACS process of care pathway.18,19 The differences in demographic, socioeconomic, and cardiovascular risk factors, comorbidities, and presentation severity between women and men in our cohort are in line with recent data focused on the multifactorial determinants of sex disparities in coronary heart disease management and outcomes.2
The QI results for the reperfusion/invasive strategy strengthen the importance of timeliness of health care delivery in the provision of care. Time-based QIs are significantly influenced by hospital system factors adjusted for patient factors, namely patient delay times.20 In fact, the high level of reperfusion distracts attention from the low level of timely reperfusion for both sexes–which is even significantly lower for women–and for patients admitted to both PCI- and non-PCI-capable hospitals. The very low proportion of patients, particularly women, transferred from non-PCI-capable hospitals for primary PCI within the target 30-minute door-in door-out time is particularly relevant in terms of health policy and planning. According to the Codi Infart registry of Catalonia, a first medical contact to arterial access time exceeding 120 minutes is strongly associated with initial admittance of a patient to a center without a catheterization laboratory.21 Implementation of the national coronary fast-track system in Portugal largely contributed to a 2-fold increase in primary angioplasty incidence from 2010 to 2015,22 but there are no data on the parallel achievement and improvement of timely reperfusion. Because these networks favor primary angioplasty rather than thrombolysis, their implementation might result in time delays that outweigh the benefits of mechanical reperfusion.21 The difference between the proportions of women and men undergoing coronary angiography within 72hours of admission is not significant, which may indicate an improvement in the timeliness of this invasive strategy for NSTEMI patients. Among patients with NSTEMI, the indication for an invasive approach depends on numerous patient factors.3 Factors possibly influencing this indication include frailty, poor cognitive status, and other comorbidities. In addition, estimated life expectancy decreases with age, and women in our cohort were significantly older than men. Not all of these factors were considered in the QI assessment. However, the main NSTEMI QI for an invasive strategy is a time-based indicator that measures time delays and not the decision to proceed with an invasive approach.
The very low level of performance of the GRACE and CRUSADE assessments among both women and men should be addressed because objective risk assessment using risk scores provides superior risk discrimination when compared with physician estimated risk.23
Use of incomplete drug combinations after an ACS is associated with a higher risk of cardiovascular morbidity and all-cause mortality.24 Results from a retrospective cohort study revealed that in Portugal women with STEMI were less likely to be discharged on aspirin and clopidogrel.25 These results are in line with our findings that a lower proportion of eligible women were discharged on dual antiplatelet therapy. High-intensity statins are recommended in all patients with AMI, irrespective of the cholesterol concentration at presentation.26 Previous studies reporting on the very high number of statin prescriptions for secondary prevention after an ACS among women and men did not address the specific types of statins.5,25 However, inadequate adherence to recommendations for high-intensity statins has already been reported27 and our results from the EPIHeart study amplify preexisting knowledge on sex differences in these prescription practices. The use of lower-intensity statin therapy may be considered in patients with an increased risk of adverse effects from statins (ie, elderly patients and those with hepatic or renal impairment, previous adverse effects, or a potential interaction with another essential concomitant therapy).26 In actual practice, frail patients who also have very low baseline low-density lipoprotein cholesterol are more likely to be discharged on lower-intensity statin therapy. However, no information was available in this study on the low-density lipoprotein cholesterol levels at presentation or the patient subgroup with an increased risk of adverse effects from statins. There were no observed differences by sex for antithrombotics and secondary prevention discharge treatment, with high levels of performance for all treatments, except for anticoagulation therapy with fondaparinux. Treatment with fondaparinux was also the QI with the widest hospital variation in the Myocardial Ischaemia National Audit Project registry.5 Although not all drug class-relative contraindications were taken into account, the most relevant variables were considered to achieve our objectives.
Increased referral to cardiac rehabilitation after an ACS, especially among women, can further reduce differences in mortality by sex because cardiac rehabilitation referral and attendance is associated with a more significant reduction in mortality in women than in men.28 The higher rates of smoking cessation advice observed for eligible women vs men may be due to evidence that this guidance is more appropriate for women because female smokers have a greater risk of developing cardiovascular disease than male smokers.1
After adjustment for GRACE score, women had twice the 30-day mortality rate of men. However, factors not captured by the GRACE risk score may have had an impact on outcomes, such as frailty and patient adherence to secondary prevention. These omissions likely limit definitive conclusions on the association between sex and the 30-day mortality rate.29,30
Due to the small number of deaths in our cohort, along with the difficulty in demonstrating the association between a single QI and the clinical outcome,31 the composite QI was used to measure the relationship between process and outcome indicators. An inverse association was found between crude mortality and attainment of this QI covering the spectrum of the AMI care pathway. However, this finding must be considered with caution because the small number of deaths, within the tertiles of attainment of the composite QI, precluded adjustment for possible confounders. Adherence to the recommended guidelines for management and treatment performance indicators has already been associated with outcomes for patients with AMI.32,33 Our results are in line with findings that sex-related differences have not been eliminated, although more than a decade has passed since sex disparities in management and outcomes were first described in a large-scale observational study.34–36 Additional in-depth studies are needed to explain our findings, particularly to explore the causal pathways for the associations between sex management and outcomes in ACS patients.
The QIs state the required explicit diagnostic or therapeutic actions, as well as define how to identify patients needing a specific action. A unique and universal standardized set of QIs for ACS does not exist. In 2015, the Spanish Society of Cardiology and the Spanish Society of Thoracic and Cardiovascular Surgery organized a task force to define outcome and process indicators for hospital cardiology practice.37 Measurement and reporting of variations by sex using validated QIs has the potential to further reduce sex inequalities in quality of care, with the ultimate goal of decreasing the higher 30-day mortality for women with AMI.
LimitationsThis study reports findings from only 2 centers and thus does not represent the national scenario for ACS quality of care and outcomes. Due to our eligibility criteria, small samples were used for some QIs. However, patient enrollment was consecutive and the 2 hospitals contributed 320 and 451 patients each. Although the door-in door-out time for transferred STEMI patients was indirectly ascertained, we do not expect systematic calculation errors with the methodology used.
Patients who died before the 6-month follow-up interview were older, more likely to be women (66.7% vs 26.0%; P < .001), and more frequently diagnosed with STEMI. Patients who were not enrolled because of clinical instability or inability to understand the questionnaire because of cognitive impairment were older, but there were no differences in the sex proportion (male 68.2% vs 74.1%; P = .389) or ACS type. Patients who refused to participate were older, less likely to be partnered, and had little formal education compared with enrolled study participants. Refusals were equally as likely as participants to be male (65.3% vs 73.8%; P = .119) and diagnosed with STEMI. The higher risk of noninclusion of women due to death in the early hours of admission means that a greater difference by sex in mortality would be expected. We do not have any more information on additional characteristics and outcomes for these high-risk patients.
CONCLUSIONSApplying the ESC ACCA QIs, we found differences in quality of care at different levels of the care pathway between women and men with AMI. These findings, along with the association of the composite QI with 30-day mortality, which is still higher in women (and although we cannot conclude that this difference in outcome is explained by sex per se) provide evidence to support measuring these validated QIs separately by sex, so as to improve guideline recommendations for management and reduce mortality from AMI in women.
FUNDINGThis work was supported by FEDER through the Operational Programme Competitiveness and Internationalization and national funding from the Foundation for Science and Technology – FCT (Portuguese Ministry of Science, Technology and Higher Education) (FCOMP-01-0124-FEDER-028709), under the project “Inequalities in coronary heart disease management and outcomes in Portugal” (Ref. FCT PTDC/DTP-EPI/0434/2012) and Unidade de Investigação em Epidemiologia - Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (POCI-01-0145-FEDER-006862; Ref. UID/DTP/04750/2013).
CONFLICTS OF INTERESTNone declared.
- –
Differences in AMI management and outcomes have been observed between women and men. Suboptimal care for women with AMI remains an issue. Use of the ESC ACCA QIs, which capture the key aspects of the AMI care pathway, has the potential to improve care and reduce unwarranted variation in death.
- –
Adherence to validated performance measures for AMI is still lower in women than in men and is associated with higher 30-day mortality. Timely reperfusion, discharge on dual antiplatelet therapy and high-intensity statins, and referral to cardiac rehabilitation were identified as targets to reduce sex inequalities in the management of these patients. Use of the ESC ACCA QIs for AMI management also has the potential to bridge the disparity gap between women and men.
The authors gratefully acknowledge the collaboration of Ana Isabel Ribeiro for the calculation of the door-in door-out time.