The 2019 European Society of Cardiology (ESC) guidelines on diabetes, prediabetes, and cardiovascular disease introduced the concept of cardiovascular (CV) risk as the basis for treating patients with diabetes and restratified it into 3 risk categories: moderate, high, and very high.1 Patients at high or very high risk should be treated with diabetes drugs with proven CV benefit, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and glucagon-like peptide 1 (GLP-1) receptor agonists.2 A need for greater participation by cardiologists in diabetes management has also been identified.2
The aim of the study was to evaluate the profile of patients with diabetes admitted to cardiology units. The study was divided into 2 phases. In the first phase, we analyzed preadmission data for patients with diabetes to assess CV risk according to the 2019 ESC guideline categories1 and prescription rates of statins, high-potency statins, SGLT2 inhibitors, and GLP-1 receptor agonists. In the second phase, we analyzed cardiology admission data to assess newly diagnosed diabetes, hemoglobin A1c (HbA1c) and proteinuria determination during admission, and treatment optimization at discharge.
Under a confidentiality agreement, the Ministry of Health of the Principality of Asturias (one of Spain's autonomous communities) was asked to furnish a list of hospital discharges for patients admitted to cardiology units over 3 consecutive months in 2019 (minimum stay, 4 days). Information on the study variables was obtained from hospital discharge reports.3
Using the R software program, we calculated descriptive statistics for patients with and without diabetes and analyzed treatments prescribed to patients with diabetes. Comparisons were made using the chi-square or Fisher exact test for categorical variables and the Kruskal-Wallis or Mann-Whitney U tests for numerical variables. Posthoc Benjamini-Hochberg correction was applied to variables with a P value <.05.
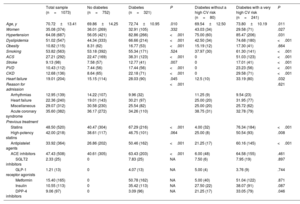
Of the 1200 patients selected, 127 were excluded due to incomplete discharge reports.3 The final sample thus comprised 1073 patients from 5 hospitals serving a population of 901 339 people (88.4% of the total population in Asturias). In total, 29.9% of the study population had diagnosed diabetes and 75% of these had a very high CV risk prior to admission. The baseline characteristics of the sample are summarized in table 1. A number of differences were observed between patients with and without diabetes and between patients with diabetes at very high CV risk and those with diabetes at high or moderate CV risk. Of note, almost half of the patients (48.5%) were on statins prior to admission, and the rate was significantly higher in those with diabetes (67%). When admitted, 76% of patients with diabetes and very high CV risk were on statins (high-potency in 50% of cases). SGLT2 inhibitors had been prescribed to 7.9% of patients with a very high CV risk and in 7.5% of those with a high or moderate risk. Analysis of prehospital glycemic control showed that 25.5% of patients had an HbA1c level <7% and 54.8% a low-density lipoprotein (LDL) cholesterol level <100mg/dL.
Baseline characteristics and previous treatments in patients with and without diabetes and patients with diabetes with and without a very high CV risk
| Total sample (n=1073) | No diabetes (n=752) | Diabetes (n=321) | P | Diabetes without a high CV risk (n=80) | Diabetes with a very high CV risk (n=241) | P | |
|---|---|---|---|---|---|---|---|
| Age, y | 70.72±13.41 | 69.86±14.25 | 72.74±10.95 | .010 | 69.54±12.50 | 73.80±10.19 | .011 |
| Women | 35.08 (374) | 36.01 (269) | 32.91 (105) | .332 | 43.03 (34) | 29.58 (71) | .027 |
| Hypertension | 64.08 (687) | 56.05 (421) | 82.86 (266) | <.001 | 75.00 (60) | 85.47 (206) | .031 |
| Dyslipidemia | 51.02 (547) | 44.34 (333) | 66.66 (214) | <.001 | 42.50 (34) | 74.68 (180) | <.001 |
| Obesity | 10.82 (115) | 8.31 (62) | 16.77 (53) | <.001 | 15.19 (12) | 17.30 (41) | .664 |
| Smoking | 53.82 (563) | 53.18 (392) | 55.34 (171) | .524 | 37.97 (30) | 61.30 (141) | <.001 |
| ACS | 27.21 (292) | 22.47 (169) | 38.31 (123) | <.001 | 0 | 51.03 (123) | <.001 |
| Stroke | 9.13 (98) | 7.58 (57) | 12.77 (41) | .007 | 0 | 17.01 (41) | <.001 |
| PVD | 10.43 (112) | 7.44 (56) | 17.44 (56) | <.001 | 0 | 23.23 (56) | <.001 |
| CKD | 12.68 (136) | 8.64 (65) | 22.18 (71) | <.001 | 0 | 29.58 (71) | <.001 |
| Heart failure | 19.01 (204) | 15.15 (114) | 28.03 (90) | .045 | 12.5 (10) | 33.19 (80) | .032 |
| Reason for admission | <.001 | .621 | |||||
| Arrhythmias | 12.95 (139) | 14.22 (107) | 9.96 (32) | 11.25 (9) | 9.54 (23) | ||
| Heart failure | 22.36 (240) | 19.01 (143) | 30.21 (97) | 25.00 (20) | 31.95 (77) | ||
| Miscellaneous | 29.07 (312) | 30.58 (230) | 25.54 (82) | 25.00 (20) | 25.72 (62) | ||
| Acute coronary syndrome | 35.60 (382) | 36.17 (272) | 34.26 (110) | 38.75 (31) | 32.78 (79) | ||
| Previous treatment | |||||||
| Statins | 48.50 (520) | 40.47 (304) | 67.29 (216) | <.001 | 4.00 (32) | 76.34 (184) | <.001 |
| High-potency statins | 42.00 (218) | 38.61 (117) | 46.75 (101) | .064 | 25.00 (8) | 50.54 (93) | .008 |
| Antiplatelet agents | 33.92 (364) | 26.86 (202) | 50.46 (162) | <.001 | 21.25 (17) | 60.16 (145) | <.001 |
| ACE inhibitors | 47.43 (508) | 40.61 (305) | 63.43 (203) | <.001 | 6.00 (48) | 64.58 (155) | .461 |
| SGLT2 inhibitors | 2.33 (25) | 0 | 7.83 (25) | NA | 7.50 (6) | 7.95 (19) | .897 |
| GLP-1 receptor agonists | 1.21 (13) | 0 | 4.07 (13) | NA | 5.00 (4) | 3.76 (9) | .744 |
| Metformin | 15.40 (165) | 0 | 50.78 (162) | NA | 5.00 (40) | 51.04 (122) | .871 |
| Insulin | 10.55 (113) | 0 | 35.42 (113) | NA | 27.50 (22) | 38.07 (91) | .087 |
| DPP-4 inhibitors | 9.06 (97) | 0 | 3.09 (96) | NA | 21.25 (17) | 33.05 (79) | .046 |
ACE, angiotensin-converting enzyme; ACS, acute coronary syndrome; CKD, chronic kidney disease; CV, cardiovascular; DPP-4, dipeptidy peptidase 4; ERC, GLP-1 RA, glucagon-like peptide 1; NA, not applicable; SGLT2, sodium-glucose cotransporter 2.
Values are expressed as mean±SD or No. (%).
According to the discharge reports, 19 patients were newly diagnosed with diabetes during hospitalization, that is, 2.5% of all patients without diabetes at baseline. HbA1c was measured in 45.5% of patients, and the differences between those with and without diabetes were nonsignificant. LDL cholesterol was measured in 70.7% of the patients overall and in 68.2% of those with diabetes. The respective percentages for proteinuria determination were 7% and 9.3%.
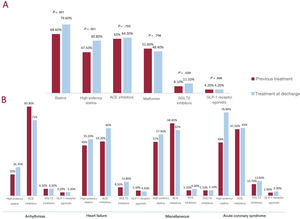
Changes to diabetes and lipid-lowering treatments noted on the discharge reports of patients with diabetes are shown in figure 1. There was a slight but significant increase in the percentage of patients prescribed SGLT2 inhibitors (from 8.1% to 11.1%, P=.039). No changes were observed in GLP-1 receptor agonist prescriptions. On analyzing the use of diabetes drugs with IA recommendations for patients at very high CV risk1 and excluding contraindications (type 1 diabetes, renal function according to 2019 summary of product characteristics, and body mass index precluding reimbursement for GLP-1 receptor agonists), we observed that just 16.1% of patients eligible for SGLT2 inhibitors and 21.3% of those eligible for GLP-1 receptor agonists had been prescribed these drugs. The increase in the use of statins is more striking. Changes in drug prescriptions according to reason for admission are shown in figure 1B. Overall increases were observed for high-potency statins (particularly in patients with acute coronary syndrome) and SGLT2 inhibitors (particularly in patients with heart failure).
A. percentages of patients with diabetes prescribed statins in general, high-potency statins, ACE inhibitors, metformin, SGLT2 inhibitors, and GLP-1 receptor agonists before hospitalization and at discharge. B. percentage of patients with diabetes prescribed high-potency statins, ACE inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists before hospitalization and at discharge. ACE, angiotensin-converting enzyme; GLP-1, glucagon-like peptide; SGLT2i, sodium-glucose cotransporter 2.
According to a recent study, just 7% of patients with diabetes are in the lowest CV risk category (moderate risk).4 There is thus ample room for improving CV risk factors before patients are admitted to hospital. In our series alone, 19 patients were newly diagnosed with diabetes, indicating that, in opposition to the 2019 ESC recommendations, proactive screening for diabetes is sorely lacking.1 We believe that cardiology admissions should be viewed as an opportunity to improve CV risk factors, regardless of the reason for admission.
Our study has some limitations, including its retrospective design. It was also conducted just months before the publication of the 2019 ESC guidelines1 and targeted just one region in Spain, although the data collection process was exhaustive.
Cardiologists could play an enhanced role in the management of CV risk in patients with diabetes before and during hospitalization for CV disorders. There is also room for improvement in screening for occult diabetes, detection of subclinical kidney disease, and prescription of new diabetes drugs with cardiovascular benefit.
FundingNone.
Authors’ ContributionsJ. Cuevas, J.M. de la Hera: data collection, study design, drafting and final revision of manuscript. D. Morena, L. Gutiérrez, P. Flórez: data collection. V. Chiminazzo: statistical analysis.
Conflicts of InterestNone
.
We would like to thank the Asturian Cardiology Society for their support and encouragement throughout this study.